Korean J Pain.
2017 Jul;30(3):214-219. 10.3344/kjp.2017.30.3.214.
Earlier treatment improves the chances of complete relief from postherpetic neuralgia
- Affiliations
-
- 1Department of Anesthesia and Pain Medicine, School of Medicine, Pusan National University, Yangsan, Korea. pain@pusan.ac.kr
- KMID: 2385354
- DOI: http://doi.org/10.3344/kjp.2017.30.3.214
Abstract
- BACKGROUND
As herpes zoster progresses via postherpetic neuralgia (PHN) to well-established PHN, it presents its recalcitrant nature to the treatment. At this point, the well-established PHN is fixed as a non-treatable, but manageable chronic painful neuropathic disorder. This study evaluated the incidence of complete relief from PHN according to PHN duration at their first visit, and the other factors influencing it.
METHODS
A retrospective chart review was performed on patients with PHN at a university-based pain clinic over 7 years. The responders were defined as patients who had complete relief from pain after 1 year of active treatment. Age, sex, PHN duration at their first visit, dermatomal distribution, and underlying disorders were compared in the responder and non-responder groups. Responders were also compared according to these factors.
RESULTS
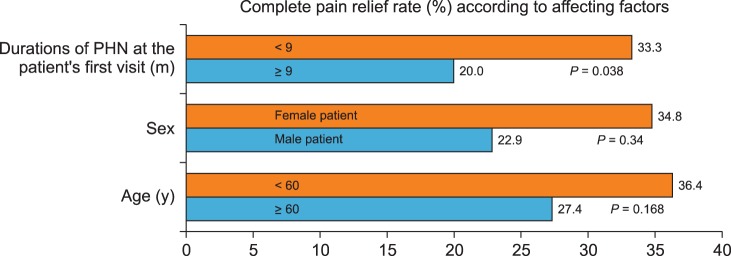
Among 117 PHN patients (M/F = 48/69), 35 patients (29.9%) had complete relief from PHN. Mean ages were 64.3 ± 10.6 and 66.9 ± 10.7 years, numbers of male to female patients were 11/24 and 37/45, and mean durations of PHN at their first visit were 8.5 ± 6.3 and 15.3 ± 10.7 months in the responder and non- responder groups, respectively. In addition, PHN patients who visited the clinic before 9 months showed a better result. Dermatomal distribution and underlying disorders did not show significant differences.
CONCLUSIONS
Almost 30% of PHN patients received complete relief. Those who sought treatment in a pain clinic before 9 months received a better result.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Modalities in managing postherpetic neuralgia
Meera Shrestha, Aijun Chen
Korean J Pain. 2018;31(4):235-243. doi: 10.3344/kjp.2018.31.4.235.
Reference
-
1. De Moragas JM, Kierland RR. The outcome of patients with herpes zoster. AMA Arch Derm. 1957; 75:193–196. PMID: 13393787.
Article2. Dworkin RH, Gnann JW Jr, Oaklander AL, Raja SN, Schmader KE, Whitley RJ. Diagnosis and assessment of pain associated with herpes zoster and postherpetic neuralgia. J Pain. 2008; 9:S37–S44. PMID: 18166464.
Article3. Thakur R, Kent JL, Dworkin RH. Herpes zoster and postherpetic neuralgia. In : Fishman SM, Ballantyne JC, Rathmell JP, editors. Bonica's management of pain. 4th ed. Philadelphia (PA): Lippincott Williams & Wilkins;2010. p. 338–357.5. Forbes HJ, Thomas SL, Smeeth L, Clayton T, Farmer R, Bhaskaran K, et al. A systematic review and meta-analysis of risk factors for postherpetic neuralgia. Pain. 2016; 157:30–54. PMID: 26218719.
Article6. Yang JY, Lee WI, Shin WK, Kim CH, Baik SW, Kim KH. Administration of four different doses of gabapentin reduces awakening from breakthrough pain and adverse effects in outpatients with neuropathic pain during the initial titration. Korean J Anesthesiol. 2013; 65:48–54. PMID: 23904939.
Article7. Joo YC, Ko ES, Cho JG, Ok YM, Jung GY, Kim KH. Intravenous nefopam reduces postherpetic neuralgia during the titration of oral medications. Korean J Pain. 2014; 27:54–62. PMID: 24478902.
Article8. Kim KH. Safe sedation and hypnosis using dexmedetomidine for minimally invasive spine surgery in a prone position. Korean J Pain. 2014; 27:313–320. PMID: 25317279.
Article9. Ok YM, Cheon JH, Choi EJ, Chang EJ, Lee HM, Kim KH. Nefopam reduces dysesthesia after percutaneous endoscopic lumbar discectomy. Korean J Pain. 2016; 29:40–47. PMID: 26839670.
Article10. Kim KH, Byeon GJ, Kim HY, Baek SH, Shin SW, Koo ST. Mechanical antiallodynic effect of intrathecal nefopam in a rat neuropathic pain model. J Korean Med Sci. 2015; 30:1189–1196. PMID: 26240499.
Article11. Kim KH, Abdi S. Rediscovery of nefopam for the treatment of neuropathic pain. Korean J Pain. 2014; 27:103–111. PMID: 24748937.
Article12. Ragozzino MW, Melton LJ 3rd, Kurland LT, Chu CP, Perry HO. Population-based study of herpes zoster and its sequelae. Medicine (Baltimore). 1982; 61:310–316. PMID: 6981045.
Article