J Cardiovasc Ultrasound.
2017 Jun;25(2):57-62. 10.4250/jcu.2017.25.2.57.
Epicardial Fat Thickness is Correlated with Vagal Hyperactivity in Patients with Neurally-Mediated Syncope
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Kosin University College of Medicine, Busan, Korea.
- 2Division of Cardiology, Department of Internal Medicine, Catholic University of Daegu College of Medicine, Daegu, Korea. mdleeys@cu.ac.kr
- 3Division of Cardiology, Department of Internal Medicine, Dongguk University College of Medicine, Gyeongju, Korea.
- KMID: 2385076
- DOI: http://doi.org/10.4250/jcu.2017.25.2.57
Abstract
- BACKGROUND
Epicardial fat tissue has unique endocrine and paracrine functions that affect the cardiac autonomic system. The head-up tilt test (HUTT) is a simple non-invasive measurement that assesses autonomic nervous system dysfunction. We investigated the association between epicardial fat thickness (EFT) and autonomic neural tone, such as vagal tone.
METHODS
A total of 797 consecutive patients (mean age 46.5 years, male: 45.7%) who underwent HUTT and echocardiography between March 2006 and June 2015 were enrolled. EFT was measured during the diastolic phase of the parasternal long axis view. We excluded patients with prior percutaneous coronary intervention, old age (* 70 years old), valvular heart disease, symptomatic arrhythmias and diabetes. We divided patients into two groups based on the HUTT (positive vs. negative).
RESULTS
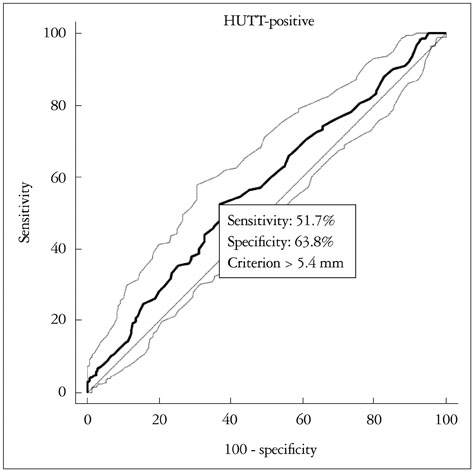
There were 329 patients (41.3%) with a negative HUTT result and 468 patients (58.7%) with a positive result. The HUTT-positive patients showed a significantly lower waist circumference, body mass index and systolic and diastolic blood pressure, although a significantly higher EFT as compared to the HUTT-negative patients (HUTT-positive, 5.69 ± 1.76 mm vs. HUTT-negative, 5.24 ± 1.60 mm; p < 0.001). EFT > 5.4 mm was associated with a positive HUTT result with 51.7% sensitivity and 63.8% specificity (p < 0.001) on receiving operator characteristic analysis. Multivariate Cox regression analysis revealed that EFT (hazard ratio: 1.02, 95% confidence interval: 1.01-1.30, p = 0.004) was an independent predictor of HUTT-positivity. CONCLSION: EFT was significantly correlated with positive HUTT, which suggests an association between EFT and autonomic dysregulation.
MeSH Terms
Figure
Reference
-
1. Ganzeboom KS, Mairuhu G, Reitsma JB, Linzer M, Wieling W, van Dijk N. Lifetime cumulative incidence of syncope in the general population: a study of 549 Dutch subjects aged 35-60 years. J Cardiovasc Electrophysiol. 2006; 17:1172–1176.2. Kapoor WN, Smith MA, Miller NL. Upright tilt testing in evaluating syncope: a comprehensive literature review. Am J Med. 1994; 97:78–88.3. Mark AL. The Bezold-Jarisch reflex revisited: clinical implications of inhibitory reflexes originating in the heart. J Am Coll Cardiol. 1983; 1:90–102.4. Kochiadakis G, Marketou M, Koukouraki S, Parthenakis F, Chlouverakis G, Karkavitsas N, Vardas P. Cardiac autonomic disturbances in patients with vasovagal syndrome: comparison between iodine-123-metaiodobenzylguanidine myocardial scintigraphy and heart rate variability. Europace. 2012; 14:1352–1358.5. Shinohara T, Ebata Y, Ayabe R, Fukui A, Okada N, Yufu K, Nakagawa M, Takahashi N. Cardiac autonomic dysfunction in patients with head-up tilt test-induced vasovagal syncope. Pacing Clin Electrophysiol. 2014; 37:1694–1701.6. Mahabadi AA, Massaro JM, Rosito GA, Levy D, Murabito JM, Wolf PA, O'Donnell CJ, Fox CS, Hoffmann U. Association of pericardial fat, intrathoracic fat, and visceral abdominal fat with cardiovascular disease burden: the Framingham Heart Study. Eur Heart J. 2009; 30:850–856.7. Sengul C, Duman D. The association of epicardial fat thickness with blunted heart rate recovery in patients with metabolic syndrome. Tohoku J Exp Med. 2011; 224:257–262.8. Rosito GA, Massaro JM, Hoffmann U, Ruberg FL, Mahabadi AA, Vasan RS, O'Donnell CJ, Fox CS. Pericardial fat, visceral abdominal fat, cardiovascular disease risk factors, and vascular calcification in a community-based sample: the Framingham Heart Study. Circulation. 2008; 117:605–613.9. Levy D, Savage DD, Garrison RJ, Anderson KM, Kannel WB, Castelli WP. Echocardiographic criteria for left ventricular hypertrophy: the Framingham Heart Study. Am J Cardiol. 1987; 59:956–960.10. Shim IK, Cho KI, Kim HS, Heo JH, Cha TJ. Impact of gender on the association of epicardial fat thickness, obesity, and circadian blood pressure pattern in hypertensive patients. J Diabetes Res. 2015; 2015:924539.11. Wallin BG, Sundlöf G. Sympathetic outflow to muscles during vasovagal syncope. J Auton Nerv Syst. 1982; 6:287–291.12. Gupta BN, Thames MD. Behavior of left ventricular mechanoreceptors with myelinated and nonmyelinated afferent vagal fibers in cats. Circ Res. 1983; 52:291–301.13. Abi-Samra F, Maloney JD, Fouad-Tarazi FM, Castle LW. The usefulness of head-up tilt testing and hemodynamic investigations in the workup of syncope of unknown origin. Pacing Clin Electrophysiol. 1988; 11:1202–1214.14. Lagi A, Tamburini C, Fattorini L, Cencetti S. Autonomic control of heart rate variability in vasovagal syncope: a study of the nighttime period in 24-hour recordings. Clin Auton Res. 1999; 9:179–183.15. Jardine DL, Ikram H, Frampton CM, Frethey R, Bennett SI, Crozier IG. Autonomic control of vasovagal syncope. Am J Physiol. 1998; 274(6 Pt 2):H2110–H2115.16. Jardine DL, Ikram H, Crozier IG. Autonomic control of asystolic vasovagal syncope. Heart. 1996; 75:528–530.17. Vaddadi G, Esler MD, Dawood T, Lambert E. Persistence of muscle sympathetic nerve activity during vasovagal syncope. Eur Heart J. 2010; 31:2027–2033.18. Tercedor L, Díaz JF, Aguado MJ, Moreno E, Molina E, Alvarez M, Ramírez JA, Pérez de la Cruz JM, Azpitarte J. [The tilt-table test in assessing syncope of unknown origin: do differences exist between children and adults?]. Rev Esp Cardiol. 1999; 52:189–195.19. Gaborit B, Venteclef N, Ancel P, Pelloux V, Gariboldi V, Leprince P, Amour J, Hatem SN, Jouve E, Dutour A, Clément K. Human epicardial adipose tissue has a specific transcriptomic signature depending on its anatomical peri-atrial, peri-ventricular, or peri-coronary location. Cardiovasc Res. 2015; 108:62–73.20. Iacobellis G, Corradi D, Sharma AM. Epicardial adipose tissue: anatomic, biomolecular and clinical relationships with the heart. Nat Clin Pract Cardiovasc Med. 2005; 2:536–543.21. Sarin S, Wenger C, Marwaha A, Qureshi A, Go BD, Woomert CA, Clark K, Nassef LA, Shirani J. Clinical significance of epicardial fat measured using cardiac multislice computed tomography. Am J Cardiol. 2008; 102:767–771.22. Chen PS, Turker I. Epicardial adipose tissue and neural mechanisms of atrial fibrillation. Circ Arrhythm Electrophysiol. 2012; 5:618–620.23. Ardell JL. The cardiac neuronal hierarchy and susceptibility to arrhythmias. Heart Rhythm. 2011; 8:590–591.24. Balcioğlu AS, Çiçek D, Akinci S, Eldem HO, Bal UA, Okyay K, Müderrisoğlu H. Arrhythmogenic evidence for epicardial adipose tissue: heart rate variability and turbulence are influenced by epicardial fat thickness. Pacing Clin Electrophysiol. 2015; 38:99–106.25. Takanashi M, Odajima T, Aota S, Sudoh M, Yamaga Y, Ono Y, Yoshinaga K, Motoji T, Matsuzaki K, Satake M, Sugimori H, Nakajima K. Risk factor analysis of vasovagal reaction from blood donation. Transfus Apher Sci. 2012; 47:319–325.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anesthesia-Related Neurally Mediated Syncope in the Perioperative Period: Two Case Reports
- Gender Difference in Patients with Recurrent Neurally Mediated Syncope
- The Clinical Characteristics and the Usefulness of the Ocular Compression Test in Syncope of Children Test
- Seizure-Like Activities during Head-Up Tilt Test-Induced Syncope
- Clinical Approach and Diagnosis of Syncope