Endocrinol Metab.
2014 Dec;29(4):584-589. 10.3803/EnM.2014.29.4.584.
Incidentally Detected Inoperable Malignant Pheochromocytoma with Hepatic Metastasis Treated by Transcatheter Arterial Chemoembolization
- Affiliations
-
- 1Department of Internal Medicine, Pusan National University School of Medicine, Busan, Korea. pons71@hanmail.net
- 2Medical Research Institute, Pusan National University School of Medicine, Busan, Korea.
- KMID: 2384259
- DOI: http://doi.org/10.3803/EnM.2014.29.4.584
Abstract
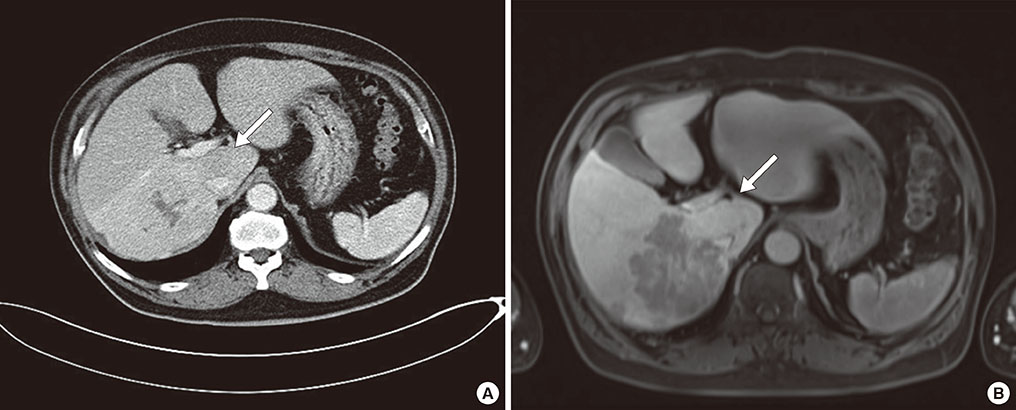
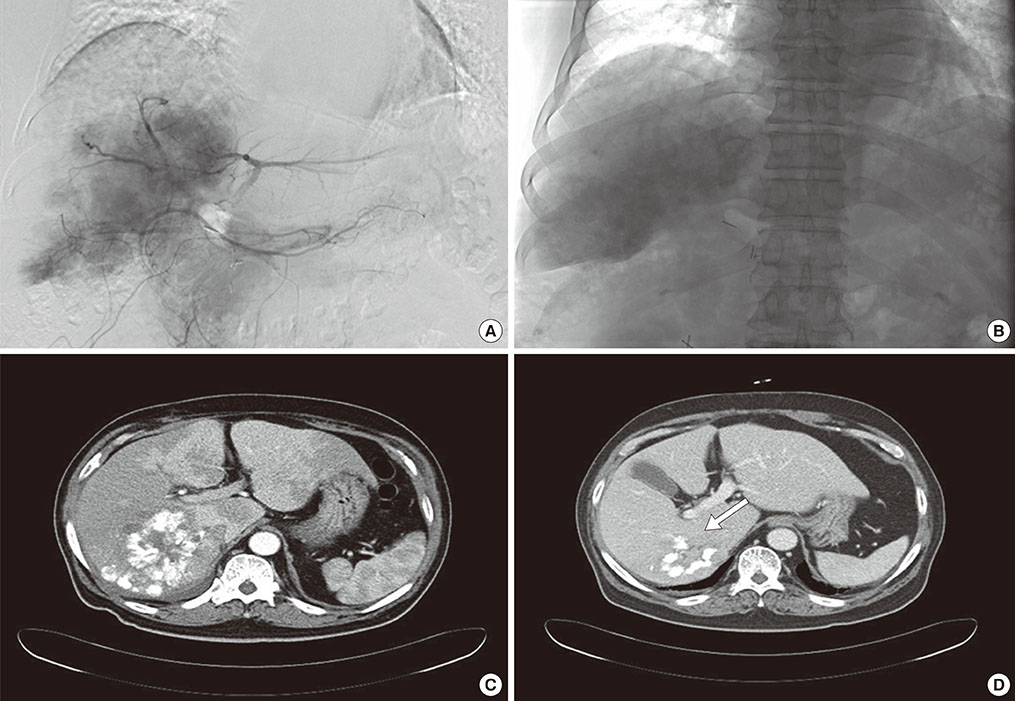
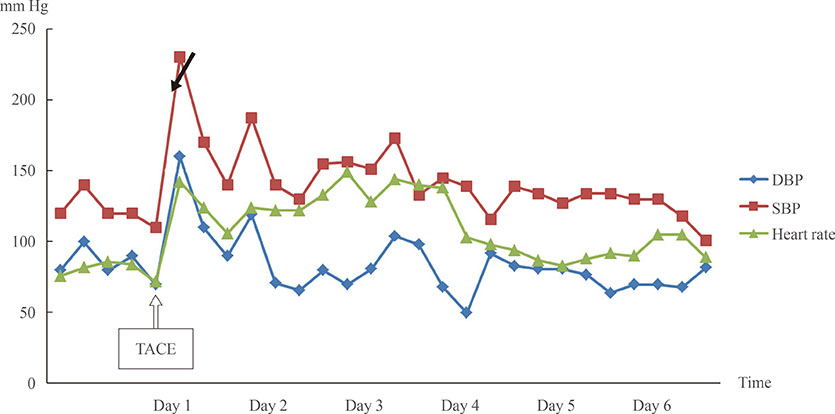
- Malignant pheochromocytoma (PCC) is a rare condition. Although the liver is the second most frequent site of metastasis in malignant PCC, no definite treatments have been established. Herein, we report a case of liver metastasis of PCC that was successfully treated by transcatheter arterial chemoembolization (TACE). A 69-year-old man was admitted to the Department of Gastroenterology for evaluation of an incidental hepatic mass in August 2013. He had undergone right adrenalectomy in May 2005 and PCC had been confirmed on the basis of histopathological findings. Liver biopsy was performed, and metastatic PCC was diagnosed. The lesion appeared inoperable because of invasion of the portal vein and metastases in the lymph nodes along the hepatoduodenal ligament. Thus, TACE was performed instead. After TACE, symptoms including dizziness and cold sweating improved, and the patient's serum catecholamine levels decreased. On the basis of this case, we believe that TACE may be a useful treatment for liver metastasis in malignant PCC.
MeSH Terms
Figure
Reference
-
1. Gruber M, Darr R, Eisenhofer G. Pheochromocytoma: update on diagnosis and therapy. Dtsch Med Wochenschr. 2014; 139:486–490.2. Hidaka S, Hiraoka A, Ochi H, Uehara T, Ninomiya T, Miyamoto Y, Hasebe A, Tanihira T, Tanabe A, Ichiryu M, Nakahara H, Tazuya N, Ninomiya I, Michitaka K. Malignant pheochromocytoma with liver metastasis treated by transcatheter arterial chemo-embolization (TACE). Intern Med. 2010; 49:645–651.3. Hori T, Yamagiwa K, Hayashi T, Yagi S, Iida T, Taniguchi K, Kawarada Y, Uemoto S. Malignant pheochromocytoma: Hepatectomy for liver metastases. World J Gastrointest Surg. 2013; 5:309–313.4. Fishbein L, Orlowski R, Cohen D. Pheochromocytoma/paraganglioma: review of perioperative management of blood pressure and update on genetic mutations associated with pheochromocytoma. J Clin Hypertens (Greenwich). 2013; 15:428–434.5. Martucci VL, Pacak K. Pheochromocytoma and paraganglioma: diagnosis, genetics, management, and treatment. Curr Probl Cancer. 2014; 38:7–41.6. Sutton MG, Sheps SG, Lie JT. Prevalence of clinically unsuspected pheochromocytoma. Review of a 50-year autopsy series. Mayo Clin Proc. 1981; 56:354–360.7. Mlika M, Kourda N, Zorgati MM, Bahri S, Ben Ammar S, Zermani R. Prognostic value of Pheochromocytoma of the Adrenal Gland Scaled Score (Pass score) tests to separate benign from malignant neoplasms. Tunis Med. 2013; 91:209–215.8. Scholz T, Eisenhofer G, Pacak K, Dralle H, Lehnert H. Clinical review: current treatment of malignant pheochromocytoma. J Clin Endocrinol Metab. 2007; 92:1217–1225.9. Hodin R, Lubitz C, Phitayakorn R, Stephen A. Diagnosis and management of pheochromocytoma. Curr Probl Surg. 2014; 51:151–187.10. Morikawa T, Suzuki M, Unno M, Endo K, Katayose Y, Matsuno S. Malignant pheochromocytoma with hepatic metastasis diagnosed 10 years after a resection of the primary incidentaloma adrenal lesion: report of a case. Surg Today. 2001; 31:80–84.11. Gimenez-Roqueplo AP, Dahia PL, Robledo M. An update on the genetics of paraganglioma, pheochromocytoma, and associated hereditary syndromes. Horm Metab Res. 2012; 44:328–333.12. Lowery AJ, Walsh S, McDermott EW, Prichard RS. Molecular and therapeutic advances in the diagnosis and management of malignant pheochromocytomas and paragangliomas. Oncologist. 2013; 18:391–407.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Palliative Transcatheter Arterial Chemoembolization for Relieving Metastatic Bone Pain due to Hepatocellular Carcinoma: A Case Report
- Pirarubicin, UFT, Leucovorin Chemotherapy in Non-embolizable and Transcatheter Arterial Chemoembolization-Failed Hepatocellular Carcinoma Patients; A Phase II Clinical Study
- A case of metastatic hepatocellular carcinoma of the rib, treated by transcatheter arterial chemoembolization
- Necrosis of Hepatocellular Carcinoma Caused by Iatrogenic Hepatic Artery Dissection during Transcatheter Arterial Chemoembolization
- Hepatocellular Carcinoma Extending to the Inferior Vena Cava and Right Atrium-A Case Report of 4 Years Survival after Repeated Transcatheter Arterial Chemoembolization Therapy -