Endocrinol Metab.
2014 Dec;29(4):470-478. 10.3803/EnM.2014.29.4.470.
Clinical Characteristics, Management, and Outcome of 22 Cases of Primary Hypophysitis
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 2Division of Endocrinology and Metabolism, Department of Internal Medicine, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea.
- 3Division of Endocrinology and Metabolism, Department of Internal Medicine, Andong Sungso hospital, Andong, Korea.
- 4Division of Endocrinology and Metabolism, Department of Internal Medicine, Dong-A Medical Center, Dong-A University College of Medicine, Busan, Korea.
- 5Division of Endocrinology and Metabolism, Department of Internal Medicine, Gachon University Gil Medical Center, Gachon University of Medicine and Science, Incheon, Korea. kwkim@gilhospital.com
- KMID: 2384244
- DOI: http://doi.org/10.3803/EnM.2014.29.4.470
Abstract
- BACKGROUND
Primary hypophysitis causes varying degrees of endocrine dysfunction and mass effect. The natural course and best treatment have not been well established.
METHODS
Medical records of 22 patients who had been diagnosed with primary hypophysitis between January 2001 and March 2013 were retrospectively reviewed. Based on the anatomical location, we classified the cases as adenohypophysitis (AH), infundibuloneurohypophysitis (INH), and panhypophysitis (PH). Clinical presentation, endocrine function, pathologic findings, magnetic resonance imaging findings, and treatment courses were reviewed.
RESULTS
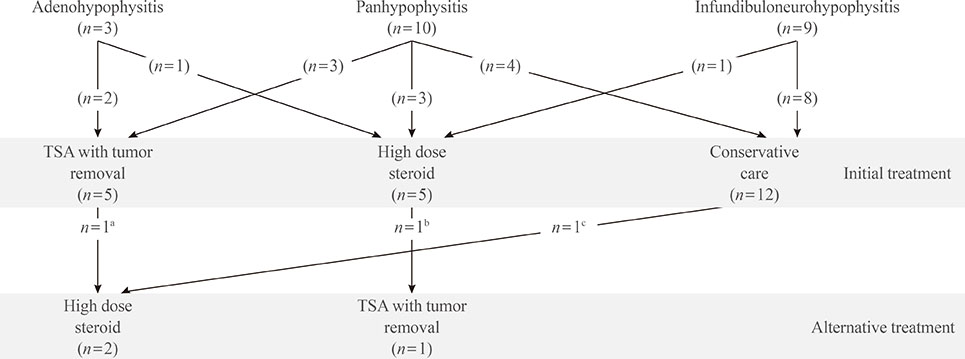
Among 22 patients with primary hypophysitis, 81.8% (18/22) had involvement of the posterior pituitary lobe. Two patients of the AH (2/3, 66.6%) and three patients of the PH (3/10, 30%) groups initially underwent surgical mass reduction. Five patients, including three of the PH (3/10, 33.3%) group and one from each of the AH (1/3, 33.3%) and INH (1/9, 11.1%) groups, initially received high-dose glucocorticoid treatment. Nearly all of the patients treated with surgery or high-dose steroid treatment (9/11, 82%) required continuous hormone replacement during the follow-up period. Twelve patients received no treatment for mass reduction due to the absence of acute symptoms and signs related to a compressive mass effect. Most of them (11/12, 92%) did not show disease progression, and three patients recovered partially from hormone deficiency.
CONCLUSION
Deficits of the posterior pituitary were the most common features in our cases of primary hypophysitis. Pituitary endocrine defects responded less favorably to glucocorticoid treatment and surgery. In the absence of symptoms related to mass effect and with the mild defect of endocrine function, it may not require treatment to reduce mass except hormone replacement.
Keyword
MeSH Terms
Figure
Reference
-
1. Caturegli P, Newschaffer C, Olivi A, Pomper MG, Burger PC, Rose NR. Autoimmune hypophysitis. Endocr Rev. 2005; 26:599–614.2. Abe T. Lymphocytic infundibulo-neurohypophysitis and infundibulo-panhypophysitis regarded as lymphocytic hypophysitis variant. Brain Tumor Pathol. 2008; 25:59–66.3. Kojima H, Nojima T, Nagashima K, Ono Y, Kudo M, Ishikura M. Diabetes insipidus caused by lymphocytic infundibuloneurohypophysitis. Arch Pathol Lab Med. 1989; 113:1399–1401.4. Leung GK, Lopes MB, Thorner MO, Vance ML, Laws ER Jr. Primary hypophysitis: a single-center experience in 16 cases. J Neurosurg. 2004; 101:262–271.5. Cosman F, Post KD, Holub DA, Wardlaw SL. Lymphocytic hypophysitis: report of 3 new cases and review of the literature. Medicine (Baltimore). 1989; 68:240–256.6. Joung JY, Jeong H, Cho YY, Huh K, Suh YL, Kim KW, Bae JC. Steroid responsive xanthomatous hypophysitis associated with autoimmune thyroiditis: a case report. Endocrinol Metab (Seoul). 2013; 28:65–69.7. Rivera JA. Lymphocytic hypophysitis: disease spectrum and approach to diagnosis and therapy. Pituitary. 2006; 9:35–45.8. Gutenberg A, Hans V, Puchner MJ, Kreutzer J, Brück W, Caturegli P, Buchfelder M. Primary hypophysitis: clinical-pathological correlations. Eur J Endocrinol. 2006; 155:101–107.9. Imura H, Nakao K, Shimatsu A, Ogawa Y, Sando T, Fujisawa I, Yamabe H. Lymphocytic infundibuloneurohypophysitis as a cause of central diabetes insipidus. N Engl J Med. 1993; 329:683–689.10. Tanaka S, Tatsumi KI, Kimura M, Takano T, Murakami Y, Takao T, Hashimoto K, Kato Y, Amino N. Detection of autoantibodies against the pituitary-specific proteins in patients with lymphocytic hypophysitis. Eur J Endocrinol. 2002; 147:767–775.11. Nishiki M, Murakami Y, Ozawa Y, Kato Y. Serum antibodies to human pituitary membrane antigens in patients with autoimmune lymphocytic hypophysitis and infundibuloneurohypophysitis. Clin Endocrinol (Oxf). 2001; 54:327–333.12. Lury KM. Inflammatory and infectious processes involving the pituitary gland. Top Magn Reson Imaging. 2005; 16:301–306.13. Bellastella A, Bizzarro A, Coronella C, Bellastella G, Sinisi AA, De Bellis A. Lymphocytic hypophysitis: a rare or underestimated disease. Eur J Endocrinol. 2003; 149:363–376.14. Ishihara T, Hino M, Kurahachi H, Kobayashi H, Kajikawa M, Moridera K, Ikekubo K, Hattori N. Long-term clinical course of two cases of lymphocytic adenohypophysitis. Endocr J. 1996; 43:433–440.15. Castle D, de Villiers JC, Melvill R. Lymphocytic adenohypophysitis. Report of a case with demonstration of spontaneous tumour regression and a review of the literature. Br J Neurosurg. 1988; 2:401–405.16. Leiba S, Schindel B, Weinstein R, Lidor I, Friedman S, Matz S. Spontaneous postpartum regression of pituitary mass with return of function. JAMA. 1986; 255:230–232.17. Zeller JR, Cerletty JM, Rabinovitch RA, Daniels D. Spontaneous regression of a postpartum pituitary mass demonstrated by computed tomography. Arch Intern Med. 1982; 142:373–374.18. Hashimoto K, Takao T, Makino S. Lymphocytic adenohypophysitis and lymphocytic infundibuloneurohypophysitis. Endocr J. 1997; 44:1–10.19. Bitton RN, Slavin M, Decker RE, Zito J, Schneider BS. The course of lymphocytic hypophysitis. Surg Neurol. 1991; 36:40–43.20. McGrail KM, Beyerl BD, Black PM, Klibanski A, Zervas NT. Lymphocytic adenohypophysitis of pregnancy with complete recovery. Neurosurgery. 1987; 20:791–793.21. Kristof RA, Van Roost D, Klingmuller D, Springer W, Schramm J. Lymphocytic hypophysitis: non-invasive diagnosis and treatment by high dose methylprednisolone pulse therapy. J Neurol Neurosurg Psychiatry. 1999; 67:398–402.22. Nussbaum CE, Okawara SH, Jacobs LS. Lymphocytic hypophysitis with involvement of the cavernous sinus and hypothalamus. Neurosurgery. 1991; 28:440–444.23. Feigenbaum SL, Martin MC, Wilson CB, Jaffe RB. Lymphocytic adenohypophysitis: a pituitary mass lesion occurring in pregnancy. Proposal for medical treatment. Am J Obstet Gynecol. 1991; 164(6 Pt 1):1549–1555.24. Yamagami K, Yoshioka K, Sakai H, Fukumoto M, Yamakita T, Hosoi M, Ishii T, Sato T, Tanaka S, Fujii S. Treatment of lymphocytic hypophysitis by high-dose methylprednisolone pulse therapy. Intern Med. 2003; 42:168–173.25. Beressi N, Cohen R, Beressi JP, Dumas JL, Legrand M, Iba-Zizen MT, Modigliani E. Pseudotumoral lymphocytic hypophysitis successfully treated by corticosteroid alone: first case report. Neurosurgery. 1994; 35:505–508.26. Cheung CC, Ezzat S, Smyth HS, Asa SL. The spectrum and significance of primary hypophysitis. J Clin Endocrinol Metab. 2001; 86:1048–1053.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lymphocytic Hypophysitis Presenting with Diabetes Insipidus in a Man: Report of a case
- Maternal Death Due to Lymphocytic Hypophysitis: A Case Report
- Lymphocytic Hypophysitis in a Patient with Testicular Feminization Syndrome
- Primary Granulomatous Hypophysitis Presenting with Panhypopituitarism and Central Diabetes Insipidus
- Lymphocytic Hypophysitis: A Cases Report