Endocrinol Metab.
2017 Jun;32(2):221-229. 10.3803/EnM.2017.32.2.221.
Utility of the Visceral Adiposity Index and Hypertriglyceridemic Waist Phenotype for Predicting Incident Hypertension
- Affiliations
-
- 1Isfahan Endocrine and Metabolism Research Center, Isfahan, Iran. janghorbani@hlth.mui.ac.ir
- 2Department of Medical Physics and Medical Engineering, Isfahan University of Medical Sciences, Isfahan, Iran.
- KMID: 2384081
- DOI: http://doi.org/10.3803/EnM.2017.32.2.221
Abstract
- BACKGROUND
The aim of this study was to assess the utility of the visceral adiposity index (VAI) and the hypertriglyceridemic waist (HTGW) phenotype as possible hypertension (HTN) predictors in a high-risk population without diabetes and HTN.
METHODS
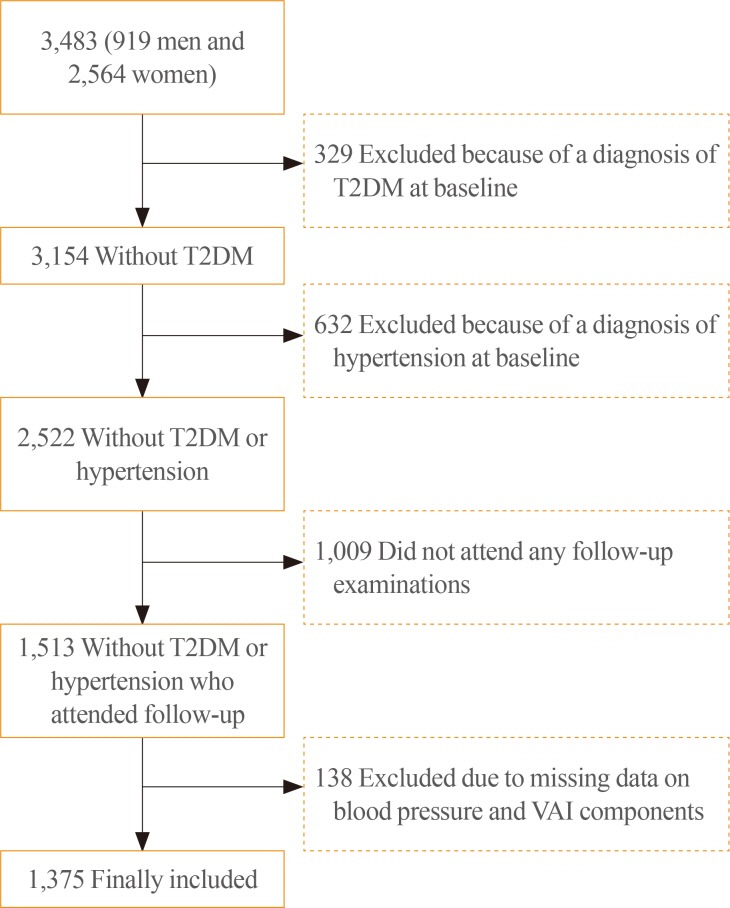
Incident HTN over a 7-year follow-up was assessed among 1,375 first-degree non-diabetic and non-hypertensive relatives of consecutive patients with type 2 diabetes who were 30 to 70 years of age. HTN was defined as a blood pressure reading ≥140/90 mm Hg or the use of antihypertensive medications. We examined the incidence of HTN across VAI quintiles and four groups defined according to baseline fasting serum triglyceride (TG) levels and waist circumference (WC).
RESULTS
The VAI and the HTGW phenotype at baseline were related to an increased risk for HTN. In comparison with the lowest VAI quintile, the highest VAI quintile showed a significant associated with HTN in an age- and gender-adjusted model (odds ratio [OR], 1.65; 95% confidence interval [CI], 1.07 to 2.55). Those with HTGW were 2.3 times (OR, 2.27; 95% CI, 1.54 to 3.35) more likely to develop HTN than those with a normal WC and normal TG levels.
CONCLUSION
Greater VAI values weakly predicted HTN, whereas the HTGW phenotype was a stronger predictor of incident HTN in an Iranian high-risk population.
MeSH Terms
Figure
Cited by 1 articles
-
Visceral-to-Subcutaneous Abdominal Fat Ratio Is Associated with Nonalcoholic Fatty Liver Disease and Liver Fibrosis
Chan-Hee Jung, Eun-Jung Rhee, Hyemi Kwon, Yoosoo Chang, Seungho Ryu, Won-Young Lee
Endocrinol Metab. 2020;35(1):165-176. doi: 10.3803/EnM.2020.35.1.165.
Reference
-
1. Poulter NR, Prabhakaran D, Caulfield M. Hypertension. Lancet. 2015; 386:801–812. PMID: 25832858.
Article2. Esteghamati A, Meysamie A, Khalilzadeh O, Rashidi A, Haghazali M, Asgari F, et al. Third national Surveillance of Risk Factors of Non-Communicable Diseases (SuRFNCD-2007) in Iran: methods and results on prevalence of diabetes, hypertension, obesity, central obesity, and dyslipidemia. BMC Public Health. 2009; 9:167. PMID: 19480675.
Article3. Gillum RF, Mussolino ME, Madans JH. Body fat distribution and hypertension incidence in women and men. The NHANES I Epidemiologic Follow-up Study. Int J Obes Relat Metab Disord. 1998; 22:127–134. PMID: 9504320.
Article4. Harris MM, Stevens J, Thomas N, Schreiner P, Folsom AR. Associations of fat distribution and obesity with hypertension in a bi-ethnic population: the ARIC study. Atherosclerosis Risk in Communities Study. Obes Res. 2000; 8:516–524. PMID: 11068957.5. Folsom AR, Prineas RJ, Kaye SA, Munger RG. Incidence of hypertension and stroke in relation to body fat distribution and other risk factors in older women. Stroke. 1990; 21:701–706. PMID: 2339449.
Article6. Cassano PA, Segal MR, Vokonas PS, Weiss ST. Body fat distribution, blood pressure, and hypertension. A prospective cohort study of men in the normative aging study. Ann Epidemiol. 1990; 1:33–48. PMID: 1669488.7. Troisi RJ, Weiss ST, Segal MR, Cassano PA, Vokonas PS, Landsberg L. The relationship of body fat distribution to blood pressure in normotensive men: the normative aging study. Int J Obes. 1990; 14:515–525. PMID: 2401588.8. Amato MC, Giordano C, Galia M, Criscimanna A, Vitabile S, Midiri M, et al. Visceral adiposity index: a reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care. 2010; 33:920–922. PMID: 20067971.9. Lemieux I, Poirier P, Bergeron J, Almeras N, Lamarche B, Cantin B, et al. Hypertriglyceridemic waist: a useful screening phenotype in preventive cardiology? Can J Cardiol. 2007; 23(Suppl B):23B–31B.
Article10. Elisha B, Messier V, Karelis A, Coderre L, Bernard S, Prud'homme D, et al. The visceral adiposity index: relationship with cardiometabolic risk factors in obese and overweight postmenopausal women: a MONET group study. Appl Physiol Nutr Metab. 2013; 38:892–899. PMID: 23855278.11. Hayashi T, Boyko EJ, Leonetti DL, McNeely MJ, Newell-Morris L, Kahn SE, et al. Visceral adiposity is an independent predictor of incident hypertension in Japanese Americans. Ann Intern Med. 2004; 140:992–1000. PMID: 15197016.
Article12. Hayashi T, Boyko EJ, Leonetti DL, McNeely MJ, Newell-Morris L, Kahn SE, et al. Visceral adiposity and the prevalence of hypertension in Japanese Americans. Circulation. 2003; 108:1718–1723. PMID: 12975250.
Article13. Fox CS, Massaro JM, Hoffmann U, Pou KM, Maurovich-Horvat P, Liu CY, et al. Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study. Circulation. 2007; 116:39–48. PMID: 17576866.14. Foy CG, Hsu FC, Haffner SM, Norris JM, Rotter JI, Henkin LF, et al. Visceral fat and prevalence of hypertension among African Americans and Hispanic Americans: findings from the IRAS family study. Am J Hypertens. 2008; 21:910–916. PMID: 18566594.
Article15. Oka R, Miura K, Sakurai M, Nakamura K, Yagi K, Miyamoto S, et al. Impacts of visceral adipose tissue and subcutaneous adipose tissue on metabolic risk factors in middle-aged Japanese. Obesity (Silver Spring). 2010; 18:153–160. PMID: 19498348.
Article16. Koh H, Hayashi T, Sato KK, Harita N, Maeda I, Nishizawa Y, et al. Visceral adiposity, not abdominal subcutaneous fat area, is associated with high blood pressure in Japanese men: the Ohtori study. Hypertens Res. 2011; 34:565–572. PMID: 21228782.
Article17. Boyko EJ, Leonetti DL, Bergstrom RW, Newell-Morris L, Fujimoto WY. Visceral adiposity, fasting plasma insulin, and blood pressure in Japanese-Americans. Diabetes Care. 1995; 18:174–181. PMID: 7729294.
Article18. Kanai H, Matsuzawa Y, Kotani K, Keno Y, Kobatake T, Nagai Y, et al. Close correlation of intra-abdominal fat accumulation to hypertension in obese women. Hypertension. 1990; 16:484–490. PMID: 2228147.
Article19. Johnson D, Prud'homme D, Despres JP, Nadeau A, Tremblay A, Bouchard C. Relation of abdominal obesity to hyperinsulinemia and high blood pressure in men. Int J Obes Relat Metab Disord. 1992; 16:881–890. PMID: 1337343.20. Amini M, Janghorbani M. Diabetes and impaired glucose regulation in first-degree relatives of patients with type 2 diabetes in isfahan, iran: prevalence and risk factors. Rev Diabet Stud. 2007; 4:169–176. PMID: 18084674.
Article21. Executive summary: standards of medical care in diabetes 2013. Diabetes Care. 2013; 36(Suppl 1):S4–S10. PMID: 23264424.22. Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 2003; 26(Suppl 1):S5–S20. PMID: 12502614.23. James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014; 311:507–520. PMID: 24352797.24. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972; 18:499–502. PMID: 4337382.
Article25. Janghorbani M, Amini M. Utility of hypertriglyceridemic waist phenotype for predicting incident type 2 diabetes: the Isfahan Diabetes Prevention Study. J Diabetes Investig. 2016; 7:860–866.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Letter: Utility of the Visceral Adiposity Index and Hypertriglyceridemic Waist Phenotype for Predicting Incident Hypertension (Endocrinol Metab 2017;32:221-9, Mohsen Janghorbani et al.)
- Response: Utility of the Visceral Adiposity Index and Hypertriglyceridemic Waist Phenotype for Predicting Incident Hypertension (Endocrinol Metab 2017;32:221-9, Mohsen Janghorbani et al.)
- Predictive ability of the Chinese visceral adiposity index for incident hypertension in working-aged Koreans
- Associations between Abdominal Adiposity and Three-dimensional Breast Density Using Digital Mammography
- Visceral Obesity