Ann Dermatol.
2011 Nov;23(4):463-467.
Second Intention Healing after Shave Excision of Benign Tumors on the Lid Margin
- Affiliations
-
- 1Department of Ophthalmology, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea.
- 2Department of Ophthalmology, Korea University College of Medicine, Seoul, Korea. shbaek6534@korea.ac.kr
- 3Kong Eye Center, Seoul, Korea.
Abstract
- BACKGROUND
Defects caused by excision of benign lid margin tumors are conventionally repaired by reconstructive surgery. However, second intention healing is another option for managing wounds on the lid margin.
OBJECTIVE
To evaluate the effectiveness of second intention healing after a shave excision of benign tumors on the lid margin.
METHODS
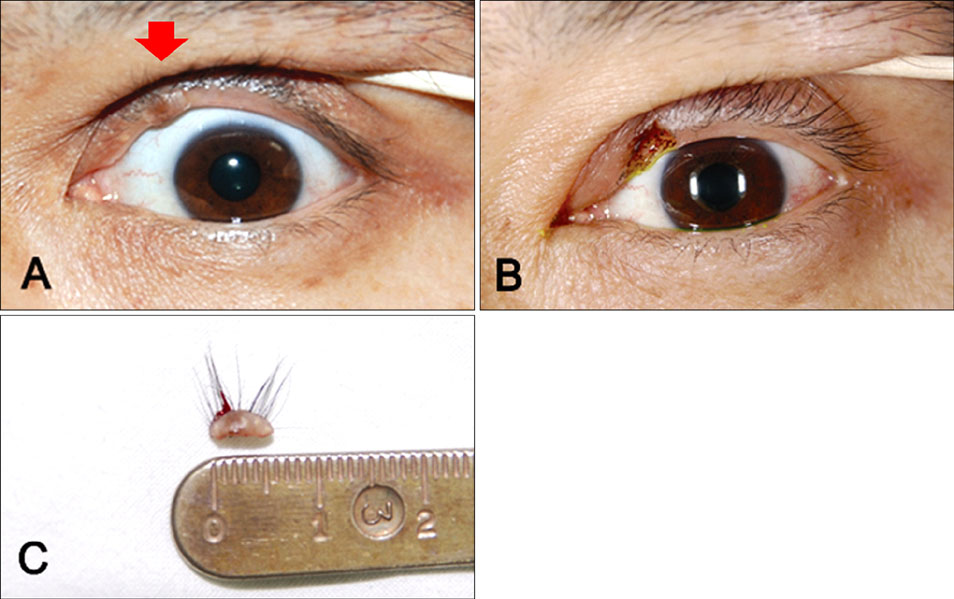
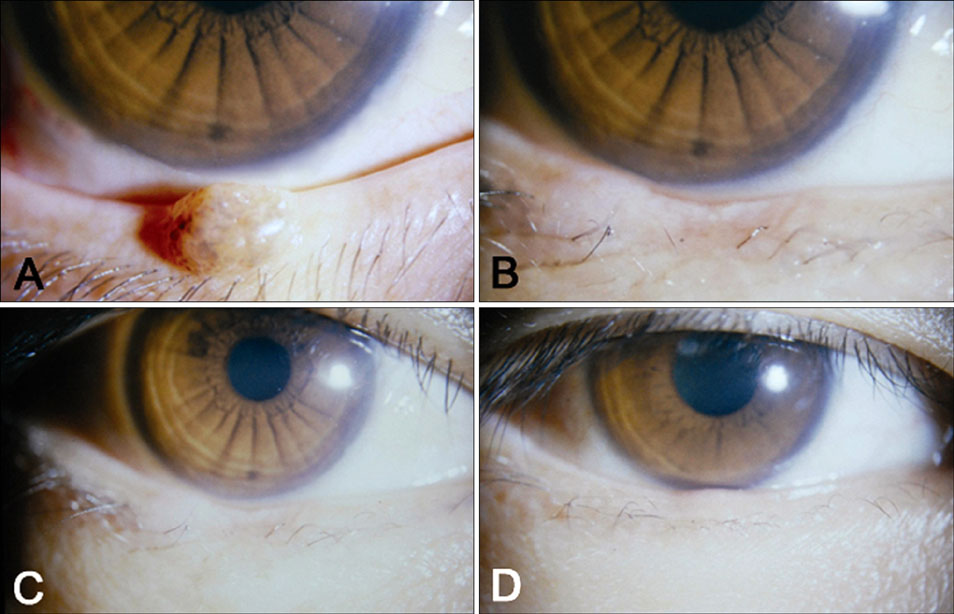
Lid defects following a shave excision of the lid margin tumor were allowed to heal by second intention in 25 patients (26 lesions). The epithelialzation period was calculated, and cosmetic and functional results and complications were evaluated by photographs and ophthalmological examination.
RESULTS
The locations of the defects were as follows: upper lid (n=13), lower lid (n=11), and both upper and lower lids (n=1). The mean tumor size was 3.8x3.6 mm, and the mean epithelialization period by second intention was 6.1+/-1.2 weeks. Pathological examinations revealed intradermal nevus (12 cases), compound nevus (five cases), squamous papilloma (five cases), and epidermal cyst (three cases). No patients had a corneal erosion, trichiasis, or hypertrophic scar, except loss of cilia in two cases. The functional and cosmetic results were satisfactory in all patients.
CONCLUSION
Healing by second intention is a safe and effective alternative to surgical reconstruction after a shave excision of benign lid margin tumors.
MeSH Terms
Figure
Reference
-
1. Tenzel RR, Stewart WB. Eyelid reconstruction by the semicircle flap technique. Ophthalmology. 1978. 85:1164–1169.
Article2. Rohrich RJ, Zbar RI. The evolution of the Hughes tarso-conjunctival flap for the lower eyelid reconstruction. Plast Reconstr Surg. 1999. 104:518–522.
Article3. Sayag D, Ducasse A, Coicaud C, Gotzamanis A, Segal A. Tarsomarginal graft. Indication and results in palpebral surgery. J Fr Ophtalmol. 2001. 24:724–728.4. Hawes MJ. Free autogenous grafts in eyelid tarsoconjunctival reconstruction. Ophthalmic Surg. 1987. 18:37–41.
Article5. Brown JB, Fryer MP. Carcinoma of eyelids and canthal region. Geriatrics. 1957. 12:181–184.6. DaCosta J, Oworu O, Jones CA. Laissez-faire: how far can you go? Orbit. 2009. 28:12–15.
Article7. Zitelli JA. Secondary intention healing: an alternative to surgical repair. Clin Dermatol. 1984. 2:92–106.
Article8. Lowry JC, Bartley GB, Garrity JA. The role of secondintention healing in periocular reconstruction. Ophthal Plast Reconstr Surg. 1997. 13:174–188.
Article9. Harrington JN. Reconstruction of the medial canthus by spontaneous granulation (Laissez-Faire): a review. Ann Ophthalmol. 1982. 14:956–960.10. Lawrence CM, Comaish JS, Dahl MG. Excision of skin tumours without wound closure. Br J Dermatol. 1986. 115:563–571.
Article11. Bernstein G. Healing by secondary intention. Dermatol Clin. 1989. 7:645–660.
Article12. Thomas JR, Frost TW. Immediate versus delayed repair of skin defects following resection of carcinoma. Otolaryngol Clin North Am. 1993. 26:203–213.
Article13. Shankar J, Nair RG, Sullivan SC. Management of peri-ocular skin tumours by laissez-faire technique: analysis of functional and cosmetic results. Eye (Lond). 2002. 16:50–53.
Article14. Zitelli JA. Wound healing by secondary intention. A cosmetic appraisal. J Am Acad Dermatol. 1983. 9:407–415.15. Fox SA, Beard C. Spontaneous Lid Repair. Am J Ophthalmol. 1964. 58:947–952.
Article16. Mehta HK. Spontaneous reformation of lower eyelid. Br J Ophthalmol. 1981. 65:202–208.
Article17. Fier RH, Older JJ. Spontaneous repair of the medial canthus after removal of basal cell carcinoma. Ophthalmic Surg. 1982. 13:737–740.
Article18. Moscona R, Pnini A, Hirshowitz B. In favor of healing by secondary intention after excision of medial canthal basal cell carcinoma. Plast Reconstr Surg. 1983. 71:189–195.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Analysis of Benign Eyelid and Conjunctival Tumors
- The Effectiveness of Partial Lid Margin Excision Including Hair Follicles in Diffuse Trichiasis and Distichiasis
- Is wide excision really needed? Correlation between resection margin and recurrence in benign phyllodes tumors of the breast
- Treatment of External Ear Keloids with the Application of Imiquimod 5% Cream after a Parallel Shave Excision
- Plasmacytoma presented as a lid mass: A case report