Ann Rehabil Med.
2016 Oct;40(5):769-778. 10.5535/arm.2016.40.5.769.
Reliability and Validity of Korean Version of Apraxia Screen of TULIA (K-AST)
- Affiliations
-
- 1Department of Rehabilitation Medicine, Konkuk University School of Medicine and Konkuk University Medical Center, Seoul, Korea. leej@kuh.ac.kr
- KMID: 2382908
- DOI: http://doi.org/10.5535/arm.2016.40.5.769
Abstract
OBJECTIVE
To evaluate the reliability and validity of Korean version of AST (K-AST) as a bedside screening test of apraxia in patients with stroke for early and reliable detection.
METHODS
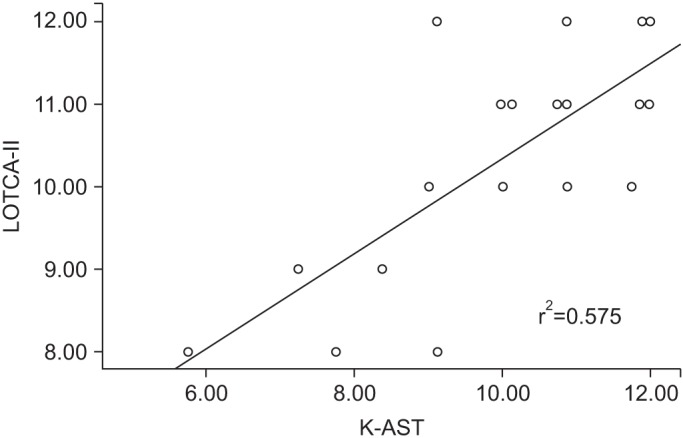
AST was translated into Korean, and the translated version received authorization from the author of AST. The performances of K-AST in 26 patients (21 males, 5 females; mean age 65.42±17.31 years) with stroke (23 ischemic, 3 hemorrhagic) were videotaped. To test the reliability and validity of K-AST, the recorded performances were assessed by two physiatrists and two occupational therapists twice at a 1-week interval. The patient performances at admission in Korean version of Mini-Mental State Examination (K-MMSE), self-care and transfer categories of Functional Independence Measure (FIM), and motor praxis area of Loewenstein Occupational Therapy Cognitive Assessment, the second edition (LOTCA-II) were also evaluated. Scores of motor praxis area of LOTCA-II was used to assess the validity of K-AST.
RESULTS
Inter-rater reliabilities were 0.983 (p<0.001) at the first assessment and 0.982 (p<0.001) at the second assessment. For intra-rater (test-retest) reliabilities, the values of four raters were 0.978 (p<0.001), 0.957 (p<0.001), 0.987 (p<0.001), and 0.977 (p<0.001). K-AST showed significant correlation (r=0.758, p<0.001) with motor praxis area of LOTCA-II test. K-AST also showed positive correlations with the total FIM score (r=0.694, p<0.001), the selfcare category of FIM (r=0.705, p<0.001) and the transfer category of FIM (r=653, p<0.001).
CONCLUSION
K-AST is a reliable and valid test for bedside screening of apraxia.
Keyword
MeSH Terms
Figure
Reference
-
1. Ochipa C, Gonzalez Rothi LJ. Limb apraxia. Semin Neurol. 2000; 20:471–478. PMID: 11149703.
Article2. Heilman KM, Maher LM, Greenwald ML, Rothi LJ. Conceptual apraxia from lateralized lesions. Neurology. 1997; 49:457–464. PMID: 9270577.
Article3. De Renzi E, Motti F, Nichelli P. Imitating gestures: a quantitative approach to ideomotor apraxia. Arch Neurol. 1980; 37:6–10. PMID: 7350907.4. Wu AJ, Burgard E, Radel J. Inpatient rehabilitation outcomes of patients with apraxia after stroke. Top Stroke Rehabil. 2014; 21:211–219. PMID: 24985388.
Article5. Buxbaum LJ, Haaland KY, Hallett M, Wheaton L, Heilman KM, Rodriguez A, et al. Treatment of limb apraxia: moving forward to improved action. Am J Phys Med Rehabil. 2008; 87:149–161. PMID: 18209511.6. Hanna-Pladdy B, Heilman KM, Foundas AL. Ecological implications of ideomotor apraxia: evidence from physical activities of daily living. Neurology. 2003; 60:487–490. PMID: 12578932.7. Sunderland A, Shinner C. Ideomotor apraxia and functional ability. Cortex. 2007; 43:359–367. PMID: 17533759.
Article8. Sundet K, Finset A, Reinvang I. Neuropsychological predictors in stroke rehabilitation. J Clin Exp Neuropsychol. 1988; 10:363–379. PMID: 3403700.
Article9. Dovern A, Fink GR, Weiss PH. Diagnosis and treatment of upper limb apraxia. J Neurol. 2012; 259:1269–1283. PMID: 22215235.
Article10. Vanbellingen T, Kersten B, Van de Winckel A, Bellion M, Baronti F, Muri R, et al. A new bedside test of gestures in stroke: the apraxia screen of TULIA (AST). J Neurol Neurosurg Psychiatry. 2011; 82:389–392. PMID: 20935324.
Article11. Wetter S, Poole JL, Haaland KY. Functional implications of ipsilesional motor deficits after unilateral stroke. Arch Phys Med Rehabil. 2005; 86:776–781. PMID: 15827931.
Article12. Saeki S, Hachisuka K. The association between stroke location and return to work after first stroke. J Stroke Cerebrovasc Dis. 2004; 13:160–163. PMID: 17903969.
Article13. Vanbellingen T, Kersten B, Van Hemelrijk B, Van de Winckel A, Bertschi M, Muri R, et al. Comprehensive assessment of gesture production: a new test of upper limb apraxia (TULIA). Eur J Neurol. 2010; 17:59–66. PMID: 19614961.
Article14. Zwinkels A, Geusgens C, van de Sande P, Van Heugten C. Assessment of apraxia: inter-rater reliability of a new apraxia test, association between apraxia and other cognitive deficits and prevalence of apraxia in a rehabilitation setting. Clin Rehabil. 2004; 18:819–827. PMID: 15573839.
Article15. Jang Y, Chern JS, Lin KC. Validity of the Loewenstein Occupational Therapy Cognitive Assessment in people with intellectual disabilities. Am J Occup Ther. 2009; 63:414–422. PMID: 19708470.
Article16. Itzkovich M, Elazar B, Averbuch S, Katz N. Loewenstein Occupational Therapy Cognitive Assessment (LOTCA) battery. 2nd ed. Pequannock: Maddak;2000.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reliability and Validity of the Comprehensive Limb and Oral Apraxia Test: Standardization and Clinical Application in Korean Patients With Stroke
- Validation of Korean Version of the Oxford Cognitive Screen (K-OCS), a Post Stroke-Specific Cognitive Screening Tool
- Korean Version of the Revised UCLA Loneliness Scale: Reliability and Validity Test
- Validity and Reliability of the Korean Version of the Index of Dental Anxiety and Fear
- Neuroanatomical Basis of Apraxia