J Korean Neurosurg Soc.
2017 May;60(3):315-321. 10.3340/jkns.2017.0101.012.
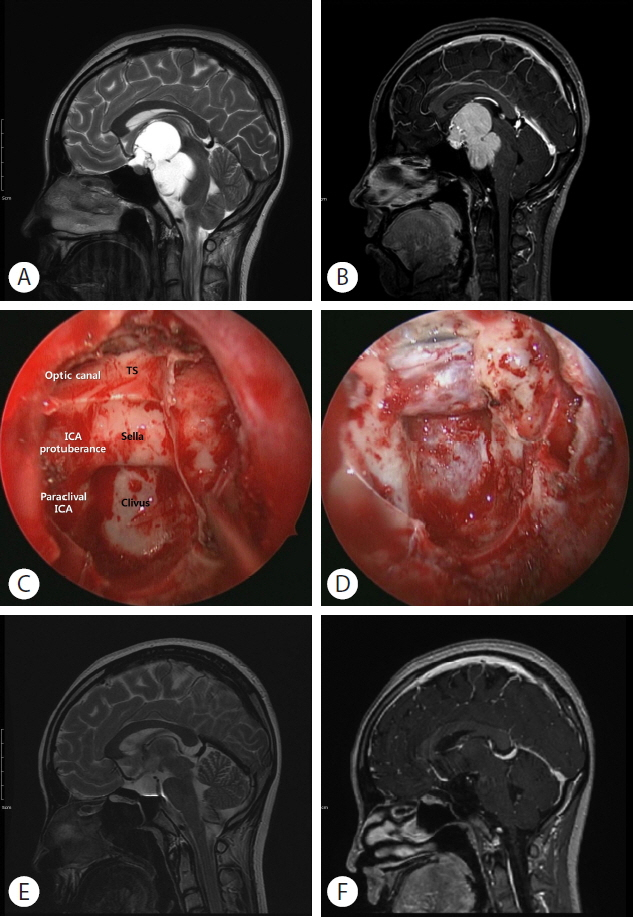
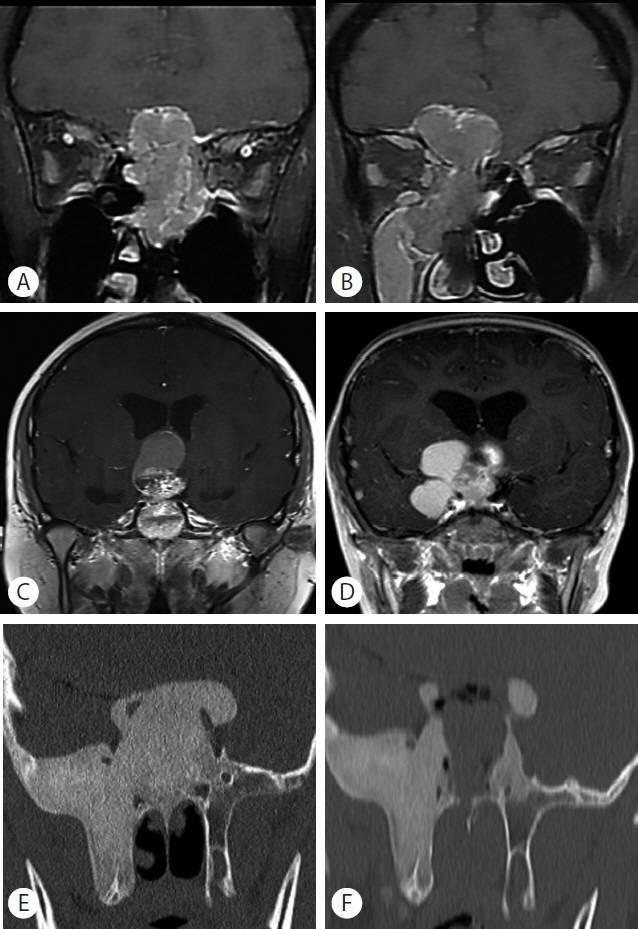
Endoscopic Endonasal Approach for Suprasellar Lesions in Children: Complications and Prevention
- Affiliations
-
- 1Department of Neurosurgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. nsthomas@snu.ac.kr
- 2Division of Pediatric Neurosurgery, Seoul National University Children’s Hospital, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2382766
- DOI: http://doi.org/10.3340/jkns.2017.0101.012
Abstract
- The endoscopic endonasal approach (EEA) has been popularized in adults and has been applied to an expanding range of surgical modules and indications in this population. However, its clinical application in pediatric neurosurgery has been impeded by the differences in anatomical features and the relatively low incidence of diseases to which it is applicable. In this review article, we mainly discuss the surgical indications, feasibility, and complications of EEA for suprasellar lesions in children based on a review of the literature, focusing especially on the age-related anatomical features of the nasal cavity, various pathologic entities, and the impact of EEA on long-term craniofacial growth.
Figure
Reference
-
References
1. Bunin GR, Surawicz TS, Witman PA, Preston-Martin S, Davis F, Bruner JM. The descriptive epidemiology of craniopharyngioma. J Neurosurg. 89:547–551. 1998.
Article2. Cappabianca P, Alfieri A, de Divitiis E. Endoscopic endonasal transsphenoidal approach to the sella: towards functional endoscopic pituitary surgery (FEPS). Minim Invasive Neurosurg. 41:66–73. 1998.
Article3. Chin OY, Ghosh R, Fang CH, Baredes S, Liu JK, Eloy JA. Internal carotid artery injury in endoscopic endonasal surgery: a systematic review. Laryngoscope. 126:582–590. 2016.
Article4. Chivukula S, Koutourousiou M, Snyderman CH, Fernandez-Miranda JC, Gardner PA, Tyler-Kabara EC. Endoscopic endonasal skull base surgery in the pediatric population. J Neurosurg Pediatr. 11:227–241. 2013.
Article5. de Lara D, Ditzel Filho LF, Prevedello DM, Carrau RL, Kasemsiri P, Otto BA, et al. Endonasal endoscopic approaches to the paramedian skull base. World Neurosurg. 82(6 Suppl):S121–S129. 2014.
Article6. Elhadi AM, Kalb S, Perez-Orribo L, Little AS, Spetzler RF, Preul MC. The journey of discovering skull base anatomy in ancient Egypt and the special influence of Alexandria. Neurosurg Focus. 33:E2. 2012.
Article7. Fanous AA, Couldwell WT. Transnasal excerebration surgery in ancient Egypt. J Neurosurg. 116:743–748. 2012.
Article8. Gandhi CD, Christiano LD, Eloy JA, Prestigiacomo CJ, Post KD. The historical evolution of transsphenoidal surgery: facilitation by technological advances. Neurosurg Focus. 27:E8. 2009.
Article9. Gardner PA, Tormenti MJ, Pant H, Fernandez-Miranda JC, Snyderman CH, Horowitz MB. Carotid artery injury during endoscopic endonasal skull base surgery: incidence and outcomes. Neurosurgery. 73(2 Suppl Operative):ons261–269. discussion ons269–ons270. 2013.
Article10. Gruber DP, Brockmeyer D. Pediatric skull base surgery. 1. Embryology and developmental anatomy. Pediatr Neurosurg. 38:2–8. 2003.11. Hadad G, Bassagasteguy L, Carrau RL, Mataza JC, Kassam A, Snyderman CH, et al. A novel reconstructive technique after endoscopic expanded endonasal approaches: vascular pedicle nasoseptal flap. Laryngoscope. 116:1882–1886. 2006.
Article12. Hong SD, Nam DH, Kong DS, Kim HY, Chung SK, Dhong HJ. Endoscopic modified transseptal transsphenoidal approach for maximal preservation of sinonasal quality of life and olfaction. World Neurosurg. 87:162–169. 2016.
Article13. Hwang JM, Kim YH, Kim JW, Kim DG, Jung HW, Chung YS. Feasibility of endoscopic endonasal approach for recurrent pituitary adenomas after microscopic trans-sphenoidal approach. J Korean Neurosurg Soc. 54:317–322. 2013.
Article14. Jankowski R, Auque J, Simon C, Marchal JC, Hepner H, Wayoff M. Endoscopic pituitary tumor surgery. Laryngoscope. 102:198–202. 1992.
Article15. Jho HD, Carrau RL, Ko Y, Daly MA. Endoscopic pituitary surgery: an early experience. Surg Neurol. 47:213–222. discussion 222–213. 1997.
Article16. Kaptain GJ, Vincent DA, Sheehan JP, Laws ER Jr. Transsphenoidal approaches for the extracapsular resection of midline suprasellar and anterior cranial base lesions. Neurosurgery. 49:94–100. discussion 100–101. 2001.
Article17. Kassam A, Snyderman CH, Carrau RL, Gardner P, Mintz A. Endoneurosurgical hemostasis techniques: lessons learned from 400 cases. Neurosurg Focus. 19:E7. 2005.
Article18. Kassam A, Snyderman CH, Mintz A, Gardner P, Carrau RL. Expanded endonasal approach: the rostrocaudal axis. Part I. Crista galli to the sella turcica. Neurosurg Focus. 19:E3. 2005.
Article19. Kassam A, Snyderman CH, Mintz A, Gardner P, Carrau RL. Expanded endonasal approach: the rostrocaudal axis. Part II. Posterior clinoids to the foramen magnum. Neurosurg Focus. 19:E4. 2005.
Article20. Kassam AB, Prevedello DM, Carrau RL, Snyderman CH, Thomas A, Gardner P, et al. Endoscopic endonasal skull base surgery: analysis of complications in the authors’ initial 800 patients. J Neurosurg. 114:1544–1568. 2011.
Article21. Kassam AB, Thomas A, Carrau RL, Snyderman CH, Vescan A, Prevedello D, et al. Endoscopic reconstruction of the cranial base using a pedicled nasoseptal flap. Neurosurgery. 63(1 Suppl 1):ONS44–ONS52. discussion ONS52–ONS53. 2008.
Article22. Kassam AB, Vescan AD, Carrau RL, Prevedello DM, Gardner P, Mintz AH, et al. Expanded endonasal approach: vidian canal as a landmark to the petrous internal carotid artery. J Neurosurg. 108:177–183. 2008.
Article23. Little AS, Kelly DF, Milligan J, Griffiths C, Prevedello DM, Carrau RL, et al. Comparison of sinonasal quality of life and health status in patients undergoing microscopic and endoscopic transsphenoidal surgery for pituitary lesions: a prospective cohort study. J Neurosurg. 123:799–807. 2015.
Article24. Liu JK, Cohen-Gadol AA, Laws ER Jr, Cole CD, Kan P, Couldwell WT. Harvey Cushing and Oskar Hirsch: early forefathers of modern transsphenoidal surgery. J Neurosurg. 103:1096–1104. 2005.
Article25. Naunheim MR, Sedaghat AR, Lin DT, Bleier BS, Holbrook EH, Curry WT, et al. Immediate and delayed complications following endoscopic skull base surgery. J Neurol Surg B Skull Base. 76:390–396. 2015.
Article26. Ostrom QT, Gittleman H, Fulop J, Liu M, Blanda R, Kromer C, et al. CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2008–2012. Neuro Oncol. 17(Suppl 4):iv1–iv62. 2015.
Article27. Rastatter JC, Snyderman CH, Gardner PA, Alden TD, Tyler-Kabara E. Endoscopic endonasal surgery for sinonasal and skull base lesions in the pediatric population. Otolaryngol Clin North Am. 48:79–99. 2015.
Article28. Sgouros S, Natarajan K, Hockley AD, Goldin JH, Wake M. Skull base growth in childhood. Pediatr Neurosurg. 31:259–268. 1999.
Article29. Shah MV, Haines SJ. Pediatric skull, skull base, and meningeal tumors. Neurosurg Clin N Am. 3:893–924. 1992.
Article30. Sindwani R, Woodard TD, Recinos PF. Building a successful endoscopic skull base and pituitary surgery practice. Otolaryngol Clin North Am. 49:1–8. 2016.
Article31. Snyderman C, Kassam A, Carrau R, Mintz A, Gardner P, Prevedello DM. Acquisition of surgical skills for endonasal skull base surgery: a training program. Laryngoscope. 117:699–705. 2007.
Article32. Tatreau JR, Patel MR, Shah RN, McKinney KA, Wheless SA, Senior BA, et al. Anatomical considerations for endoscopic endonasal skull base surgery in pediatric patients. Laryngoscope. 120:1730–1737. 2010.
Article33. Valentine R, Boase S, Jervis-Bardy J, Dones Cabral JD, Robinson S, Wormald PJ. The efficacy of hemostatic techniques in the sheep model of carotid artery injury. Int Forum Allergy Rhinol. 1:118–122. 2011.
Article34. Venkatramani R, Pan H, Furman WL, Marron JM, Haduong J, Friedrich-Medina P, et al. Multimodality treatment of pediatric esthesioneuroblastoma. Pediatr Blood Cancer. 63:465–470. 2016.
Article35. Zhan R, Xin T, Li X, Li W, Li X. Endonasal endoscopic transsphenoidal approach to lesions of the sellar region in pediatric patients. J Craniofac Surg. 26:1818–1822. 2015.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Deliberate Two-Staged Endoscopic Endonasal Transsphenoidal Surgery in Large Pituitary Adenomas
- Endoscopic Endonasal Skull Base Repair with Nasoseptal Flap
- The endoscopic transnasal approach to the lesions of the craniocervical junction: two case reports
- Two Cases of Frontal Sinus Inverted Papilloma Treated With a Combined Bifrontal Craniotomy and Endonasal Endoscopic Approach
- Clinical Analysis for Complications after Endoscopic Sinus Surgery in Korea during Past 7 Years