J Korean Ophthalmol Soc.
2017 Jun;58(6):718-724. 10.3341/jkos.2017.58.6.718.
Treatment of Rhino-Orbito-Cerebral Aspergillosis with Combination of Amphotericin, Posaconazole and Amphotericin Irrigation: A Case Report
- Affiliations
-
- 1Department of Ophthalmology, Wonkwang University School of Medicine, Iksan, Korea. sangduck@wonkwang.ac.kr
- 2Institute of Wonkwang Medical Science, Wonkwang University, Iksan, Korea.
- 3Department of Pathology, Wonkwang University School of Medicine, Iksan, Korea.
- KMID: 2382682
- DOI: http://doi.org/10.3341/jkos.2017.58.6.718
Abstract
- PURPOSE
To report a case of rhino-orbito-cerebral aspergillosis successfully treated with a combination of amphotericin B, posaconazole and amphotericin B irrigation.
CASE SUMMARY
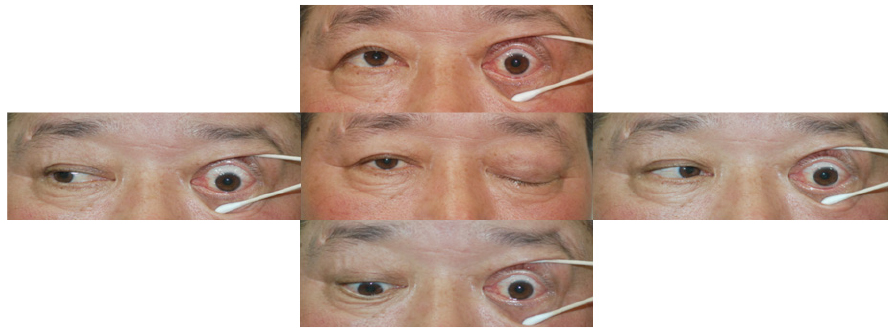
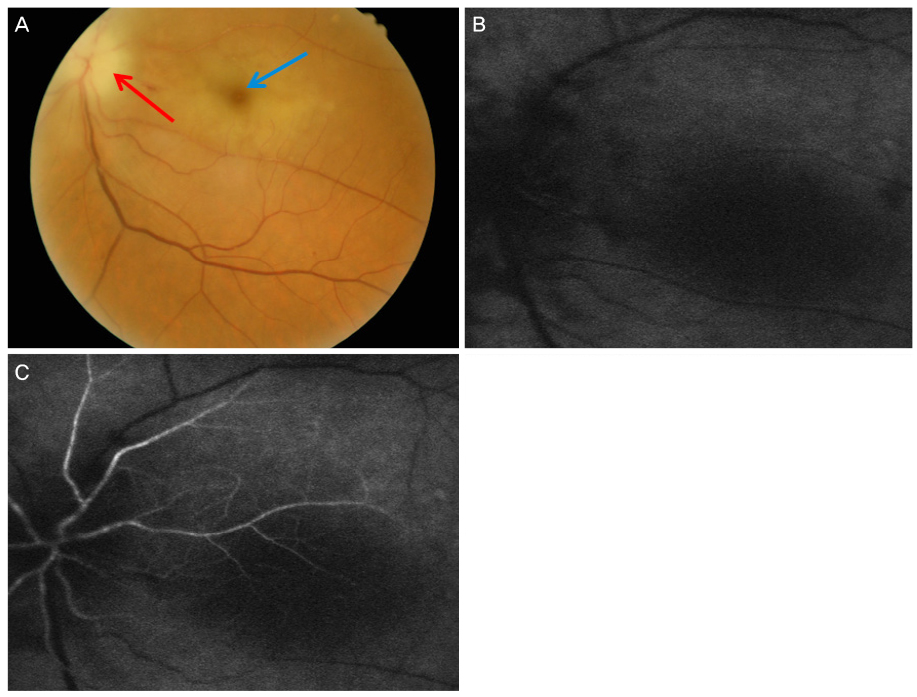
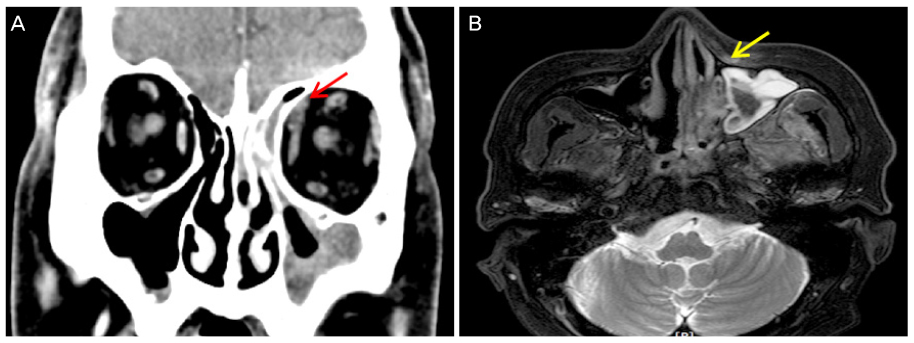
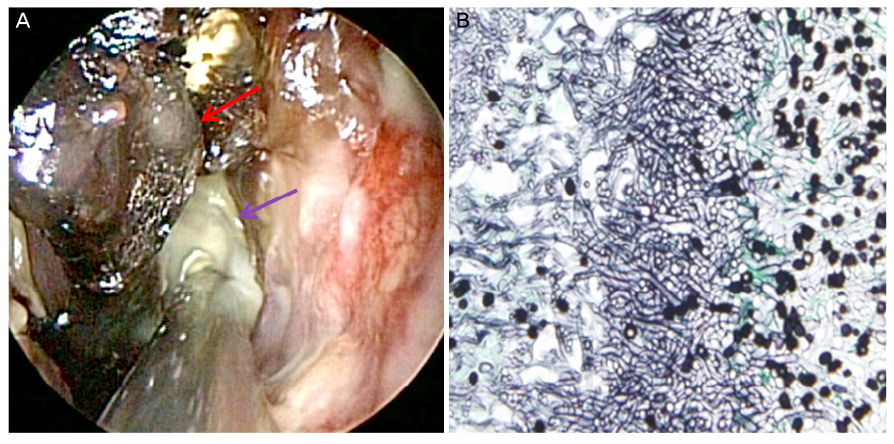
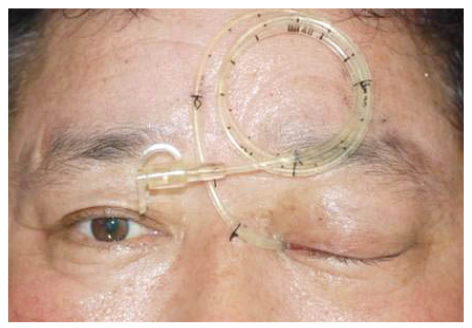
A 59-year-old male with hypertension, diabetes mellitus and hyperlipidemia was admitted to our neurology department for left facial paresthesia, pain and consulted to ophthalmology for left eyeball pain. His visual acuity was no light perception in the left eye, and fundus examination showed papilledema and a cherry-red spot. Left exophthalmos and complete ptosis with ophthalmoplegia were also observed. Orbital computed tomography revealed left maxillary and ethmoid sinusitis, and nasal endoscopic examination revealed a black eschar adjacent to the middle turbinate. Subsequent biopsy suggested mucormycosis. The patient was immediately treated with a combination of amphotericin B and posaconazole. In addition, left endoscopic sinus surgery was performed and aspergillosis was histopathologically confirmed. The patient underwent amphotericin B irrigation for 5 days after canula insertion up to orbital apex. The patient survived for 18 months and is still alive.
CONCLUSIONS
A combination of amphotericin B, posaconazole and amphotericin B irrigation using the canula through the orbital apex may be helpful in treating patients with rhino-orbito-cerebral aspergillosis who refuse orbital exenteration.
Keyword
MeSH Terms
Figure
Reference
-
1. Zuniga MG, Turner JH. Treatment outcomes in acute invasive fungal rhinosinusitis. Curr Opin Otolaryngol Head Neck Surg. 2014; 22:242–248.2. Levin LA, Avery R, Shore JW, et al. The spectrum of orbital aspergillosis: a clinicopathological review. Surv Ophthalmol. 1996; 41:142–154.3. Choi HS, Choi JY, Yoon JS, et al. Clinical characteristics and prognosis of orbital invasive aspergillosis. Ophthal Plast Reconstr Surg. 2008; 24:454–459.4. Sivak-Callcott JA, Livesley N, Nugent RA, et al. Localised invasive sino-orbital aspergillosis: characteristic features. Br J Ophthalmol. 2004; 88:681–687.5. Wakabayashi T, Oda H, Kinoshita N, et al. Retrobulbar amphotericin B injections for treatment of invasive sino-orbital aspergillosis. Jpn J Ophthalmol. 2007; 51:309–311.6. Kusaka K, Shimamura I, Ohashi Y, Ota S. Long term survival of patient with invasive aspergillosis involving orbit, paranasal sinus, and central nervous system. Br J Ophthalmol. 2003; 87:791–792.7. Dökmetaş HS, Canbay E, Yilmaz S, et al. Diabetic ketoacidosis and rhino-orbital mucormycosis. Diabetes Res Clin Pract. 2002; 57:139–142.8. Arora V, Nagarkar NM, Dass A, Malhotra A. Invasive rhino-orbital aspergillosis. Indian J Otolaryngol Head Neck Surg. 2011; 63:325–329.9. Walsh TJ, Hiemenz JW, Seibel NL, et al. Amphotericin B lipid complex for invasive fungal infections: analysis of safety and efficacy in 556 cases. Clin Infect Dis. 1998; 26:1383–1396.10. Trief D, Gray ST, Jakobiec FA, et al. Invasive fungal disease of the sinus and orbit: a comparison between mucormycosis and Aspergillus. Br J Ophthalmol. 2016; 100:184–188.11. Torres-Damas W, Yumpo-Cárdenas D, Mota-Anaya E. Coinfection of rhinocerebral mucormycosis and sinus aspergillosis. Rev Peru Med Exp Salud Publica. 2015; 32:813–817.12. Rickerts V, Just-Nübling G, Konrad F, et al. Diagnosis of invasive aspergillosis and mucormycosis in immunocompromised patients by seminested PCR assay of tissue samples. Eur J Clin Microbiol Infect Dis. 2006; 25:8–13.13. Walsh TJ, Finberg RW, Arndt C, et al. Liposomal amphotericin B for empirical therapy in patients with persistent fever and neutropenia. National Institute of Allergy and Infectious Diseases Mycoses Study Group. N Engl J Med. 1999; 340:764–771.14. Lim SH, Sung SH, Lim KH. A case of invasive aspergillosis involving the orbital apex and occipital lobe: successful treatment with voriconazole. J Korean Ophthalmol Soc. 2013; 54:540–544.15. Herbrecht R, Denning DW, Patterson TF, et al. Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med. 2002; 347:408–415.16. Diekema DJ, Messer SA, Hollis RJ, et al. Activities of caspofungin, itraconazole, posaconazole, ravuconazole, voriconazole, and amphotericin B against 448 recent clinical isolates of filamentous fungi. J Clin Microbiol. 2003; 41:3623–3626.17. Mahomed S, Basanth S, Mlisana K. The successful use of amphotericin B followed by oral posaconazole in a rare case of invasive fungal sinusitis caused by co-infection with mucormycosis and aspergillus. IDCases. 2015; 2:116–117.18. Dhiwakar M, Thakar A, Bahadur S. Invasive sino-orbital aspergillosis: surgical decisions and dilemmas. J Laryngol Otol. 2003; 117:280–285.19. Arndt S, Aschendorff A, Echternach M, et al. Rhino-orbital-cerebral mucormycosis and aspergillosis: differential diagnosis and treatment. Eur Arch Otorhinolaryngol. 2009; 266:71–76.20. Seiff SR, Choo PH, Carter SR. Role of local amphotericin B therapy for sino-orbital fungal infections. Ophthal Plast Reconstr Surg. 1999; 15:28–31.21. Foster CS, Lass JH, Moran-Wallace K, Giovanoni R. Ocular toxicity of topical antifungal agents. Arch Ophthalmol. 1981; 99:1081–1084.22. Cho HJ, Jang MS, Hong SD, et al. Prognostic factors for survival in patients with acute invasive fungal rhinosinusitis. Am J Rhinol Allergy. 2015; 29:48–53.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Rhino-Orbital-Cerebral Mucormycosis Successfully Treated by Surgical Treatment and Posaconazole
- Recurrent Cerebral Infarction due to Rhino-Orbito-Cerebral Mucormycosis
- Successful Treatment of a Case with Rhino-Orbital-Cerebral Mucormycosis by the Combination of Neurosurgical Intervention and the Sequential Use of Amphotericin B and Posaconazole
- Successful Treatment of Rhino-Orbital Mucormycosis with Posaconazole after Combination of Surgical Treatment and Amphotericin B
- A Case of the Orbital Aspergillosis