J Pathol Transl Med.
2015 Jan;49(1):85-88. 10.4132/jptm.2014.10.28.
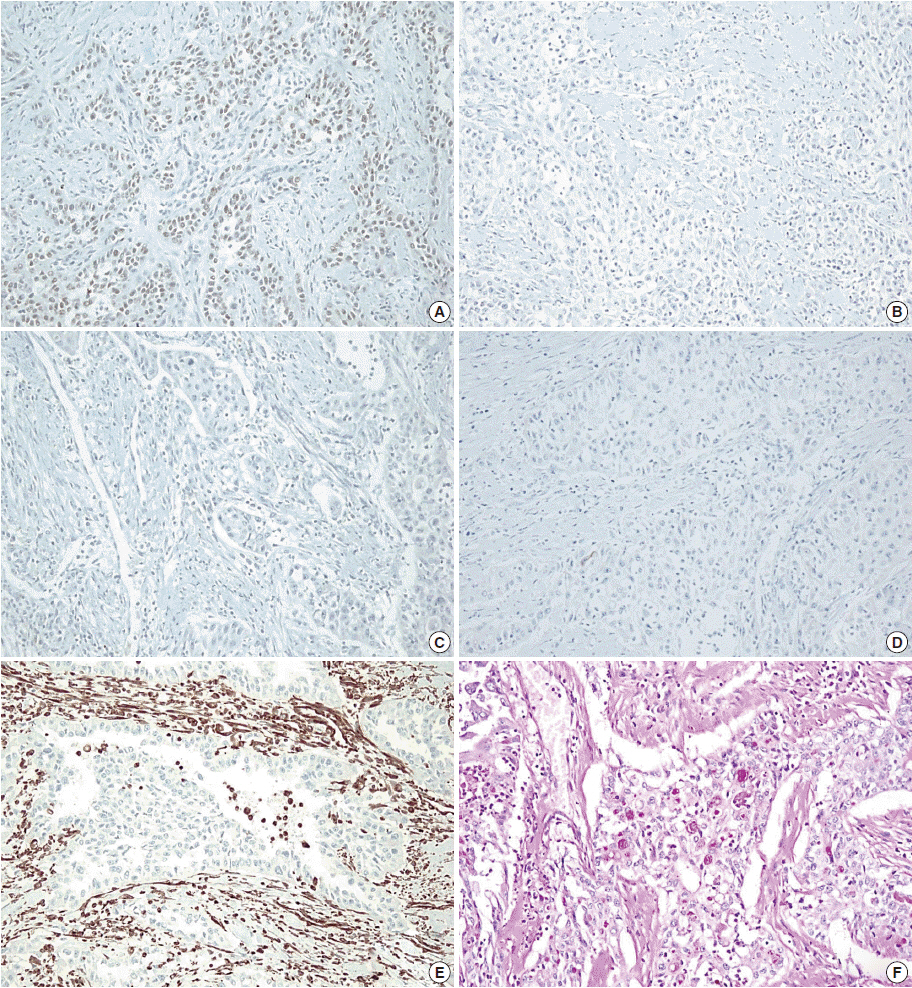
Squamous Cell Carcinoma of the Seminal Vesicle from Zinner Syndrome: A Case Report and Review of Literature
- Affiliations
-
- 1Department of Pathology, Seoul National University College of Medicine, Seoul, Korea. blue7270@snu.ac.kr
- KMID: 2381360
- DOI: http://doi.org/10.4132/jptm.2014.10.28
Abstract
- No abstract available.
MeSH Terms
Figure
Reference
-
1. Lorber G, Pizov G, Gofrit ON, Pode D. Seminal vesicle cystadenoma: a rare clinical perspective. Eur Urol. 2011; 60:388–91.
Article2. Tabata K, Irie A, Ishii D, Yanagisawa N, Iwamura M, Baba S. Primary squamous cell carcinoma of the seminal vesicle. Urology. 2002; 59:445.
Article3. Yanagisawa N, Saegusa M, Yoshida T, Okayasu I. Squamous cell carcinoma arising from a seminal vesicular cyst: possible relationship between chronic inflammation and tumor development. Pathol Int. 2002; 52:249–53.
Article4. Wang J, Yue X, Zhao R, Cheng B, Wazir R, Wang K. Primary squamous cell carcinoma of seminal vesicle: an extremely rare case report with literature review. Int Urol Nephrol. 2013; 45:135–8.
Article5. Shoda T, Mitsumori K, Imazawa T, et al. A spontaneous seminal vesicle adenocarcinoma in an aged F344 rat. Toxicol Pathol. 1998; 26:448–51.
Article6. Ghirardini G, Magnani A. Mayer-Rokitansky-Küster-Hauser syndrome and ovarian cancer: report of a case. Clin Exp Obstet Gynecol. 1995; 22:247–8.7. Mermerkaya M, Burgu B, Hamidi N, et al. Mayer-Rokitansky-Küster-Hauser syndrome accompanied by renal cell carcinoma: a case report. J Pediatr Hematol Oncol. 2013; 35:e309–10.8. Okada Y, Tanaka H, Takeuchi H, Yoshida O. Papillary adenocarcinoma in a seminal vesicle cyst associated with ipsilateral renal agenesis: a case report. J Urol. 1992; 148:1543–5.
Article9. Lee BH, Seo JW, Han YH, Kim YH, Cha SJ. Primary mucinous adenocarcinoma of a seminal vesicle cyst associated with ectopic ureter and ipsilateral renal agenesis: a case report. Korean J Radiol. 2007; 8:258–61.
Article10. Ocque R, Tochigi N, Ohori NP, Dacic S. Usefulness of immunohistochemical and histochemical studies in the classification of lung adenocarcinoma and squamous cell carcinoma in cytologic specimens. Am J Clin Pathol. 2011; 136:81–7.
Article