J Educ Eval Health Prof.
2013;10:10.
Is it time for integration of surgical skills simulation into the United Kingdom undergraduate medical curriculum? A perspective from King's College London School of Medicine
- Affiliations
-
- 1Department of Surgery, Imperial College London, London, UK.
- 2Department of Plastic and Reconstructive Surgery, Queen Elizabeth Hospital Birmingham, Birmingham, UK. hazim.sadideen@doctors.org.uk
- 3Department of Orthopaedic Surgery, King Saud University, Riyadh, Saudi Arabia.
- 4Department of General Surgery, North West London Hospitals NHS Trust, London, UK.
- 5Department of Surgery, William Harvey Hospital, East Kent Foundation Trust, Ashford, UK.
- 6Centre for Global Health, King's College London, Weston Education Centre, London, UK.
Abstract
- PURPOSE
Changes in undergraduate medical curricula, combined with reforms in postgraduate education, have training implications for surgical skills acquisition in a climate of reduced clinical exposure. Confidence and prior experience influences the educational impact of learning. Currently there is no basic surgical skills (BSS) programme integrated into undergraduate curricula in the United Kingdom. We explored the role of a dedicated BSS programme for undergraduates in improving confidence and influencing careers in King's College London School of Medicine, and the programme was evaluated.
METHODS
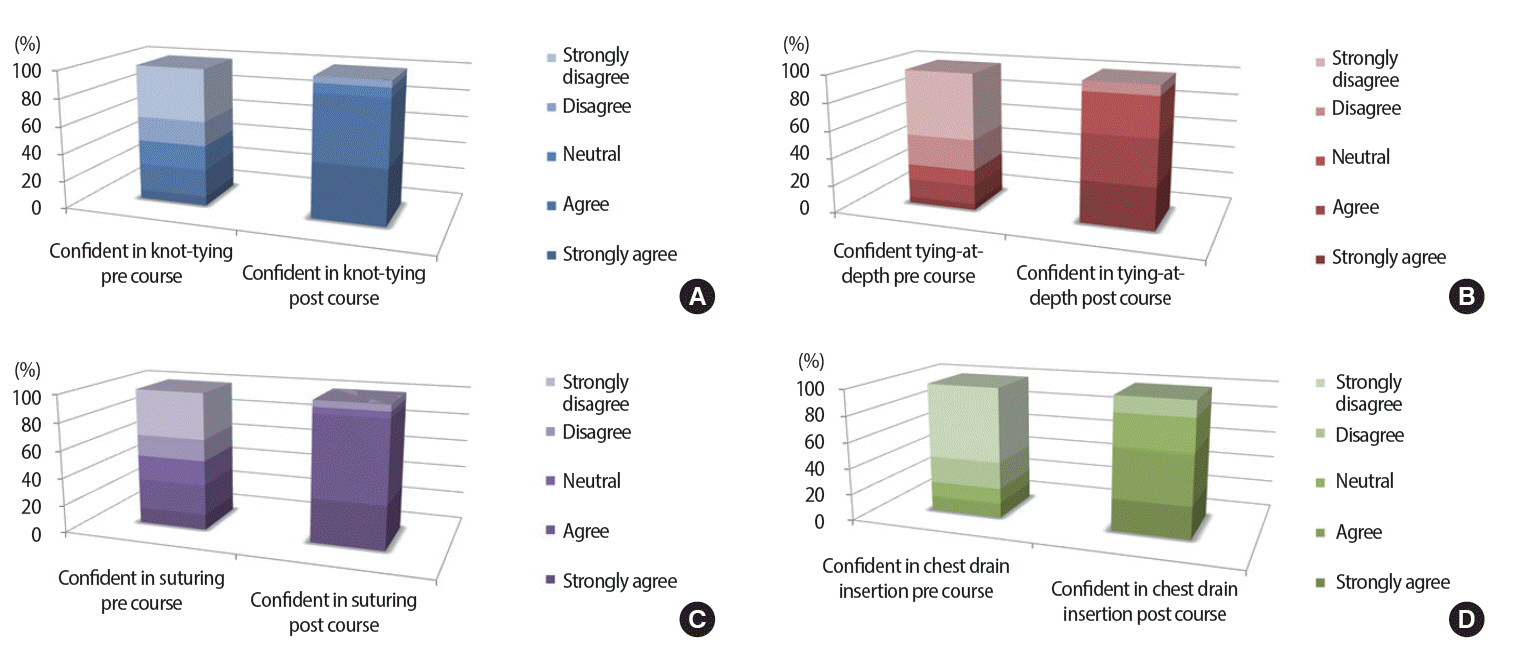
A programme was designed in-line with the established Royal College of Surgeons course. Undergraduates were taught four key skills over four weeks: knot-tying, basic-suturing, tying-at-depth and chest-drain insertion, using low-fidelity bench-top models. A Likert-style questionnaire was designed to determine educational value and influence on career choice. Qualitative data was collected.
RESULTS
Only 29% and 42% of students had undertaken previous practice in knot-tying and basic suturing, respectively. 96% agreed that skills exposure prior to starting surgical rotations was essential and felt a dedicated course would augment undergraduate training. There was a significant increase in confidence in the practice and knowledge of all skills taught (p<0.01), with a greater motivation to be actively involved in the surgical firm and theatres.
CONCLUSION
A simple, structured BSS programme can increase the confidence and motivation of students. Early surgical skills targeting is valuable for students entering surgical, related allied, and even traditionally non-surgical specialties such as general practice. Such experience can increase the confidence of future junior doctors and trainees. We advocate the introduction of a BSS programme into United Kingdom undergraduate curricula.
Keyword
MeSH Terms
Figure
Reference
-
1. Wass V. Monitoring the medical education revolution. BMJ. 2003; 327:1362. http://dx.doi.org/10.1136/bmj.327.7428.1362.
Article2. Naylor R a, Hollett L a, Castellvi A, Valentine RJ, Scott DJ. Preparing medical students to enter surgery residencies. Am J Surg. 2010; 199:105–109. http://dx.doi.org/10.1016/j.amjsurg.2009.09.003.
Article3. Sanfey H, Dunnington G. Verification of proficiency: a prerequisite for clinical experience. Surg Clin North Am. 2010; 90:559–567. http://dx.doi.org/10.1016/j.suc.2010.02.008.
Article4. Meyers MO, Meyer AA, Stewart RD, Dreesen EB, Barrick J, Lange PA, Farrell TM. Teaching technical skills to medical students during a surgery clerkship: results of a small group curriculum. J Surg Res. 2011; 166:171–175. http://dx.doi.org/ 10.1016/j.jss.2010.05.019.
Article5. Zaid H, Ward D, Sammann A, Tendick F, Topp KS, Maa J. Integrating surgical skills education into the anatomy laboratory. J Surg Res. 2010; 158:36–42. http://dx.doi.org/10.1016/j.jss.2008.08.012.
Article6. Sadideen H, Kneebone R. Practical skills teaching in contemporary surgical education: how can educational theory be applied to promote effective learning? Am J Surg. 2012; 204:396–401. http://dx.doi.org/10.1016/j.amjsurg.2011.12.020.
Article7. Kneebone R, Arora S, King D, Bello F, Sevdalis N, Kassab E, Aggarwal R, Darzi A, Nestel D. Distributed simulation--accessible immersive training. Med teach. 2010; 32:65–70. http://dx.doi.org/10.3109/01421590903419749.8. DiMaggio PJ, Waer AL, Desmarais TJ, Sozanski J, Timmerman H, Lopez JA, Poskus DM, Tatum J, Adamas-Rappaport WJ. The use of a lightly preserved cadaver and full thickness pig skin to teach technical skills on the surgery clerkship: a response to the economic pressures facing academic medicine today. Am J Surg. 2010; 200:162–166. http://dx.doi.org/10.1016/j.amjsurg.2009.07.039.9. Royal College of General Practitioners [Internet]. London: Royal College of General Practitioners; [cited 2013 Apr 16]. Available from: http://www.rcgp.org.uk/new_professionals/students.aspx .10. NICE update of guidance on the treatment and care of people with skin cancer May 2010 [Internet]. London: National Institute for Health and Care Excellence; 2010 [cited 2013 June 6] Available from: http://www.nice.org.uk/newsroom/pressreleases/NICEUpdatesSkinCancerGuidance.jsp?domedia=1&mid=CFD181FC-19B9-E0B5-D4A6D733187B4EE6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A comparative analysis of single port versus multi-port robotic assisted radical prostatectomy for prostate cancer
- Is Hib Vaccine of Economic Value in South Korea?
- The Introduction and Development of Graduate Entry Programmes in the United Kingdom
- Development of e-learning in medical education: a student's perspective
- Nutcracker Phenomenon and Syndrome May Be More Prevalent Than Previously Thought