J Korean Med Assoc.
2017 Apr;60(4):323-329. 10.5124/jkma.2017.60.4.323.
Overdiagnosis in health care: impact of cancer screening
- Affiliations
-
- 1Department of Preventive Medicine, Korea University College of Medicine, Seoul, Korea. ahnhann@gmail.com
- KMID: 2378216
- DOI: http://doi.org/10.5124/jkma.2017.60.4.323
Abstract
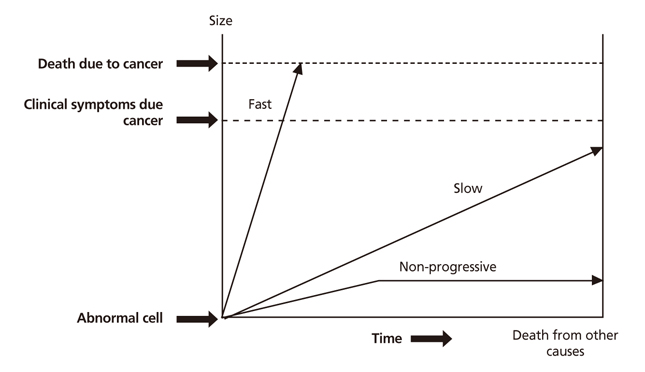
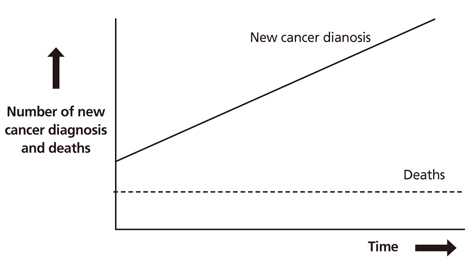
- While overtreatment in medical services has for a long time been a topic of interest among the medical community, the concept of overdiagnosis has recently attracted interest because of the increasing scientific evidence supporting it; there are numerous academic papers investigating "˜overdiagnosis' which have been published. Overdiagnosis is the phenomenon of a disease being diagnosed that will never progress to the point of causing symptoms or death. In certain individuals, even despite the detection of cancer cells, the person will die of other disease before the cancer can progress. It is known that overdiagnosis occurs in various diseases, such as high blood pressure, diabetes, and various psychiatric disorders. In cancer, there exist slow growing cancers in which symptoms and death often occur late and thus the patient will ultimately die of another cause before they are affected by the cancer. Through this, there is a potential of overdiagnosis due to early cancer screening. Overdiagnosed patients are harmed by the diagnosis and treatment which in no way benefit them. The general public as well as health care professionals should be informed of the balance between the benefits and harms. This article will analyze the problems related to overdiagnosis with a focus on early screening in cancer.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Trends in Prostate Cancer Prevalence and Radical Prostatectomy Rate according to Age Structural Changes in South Korea between 2005 and 2015
Hyun Young Lee, Suyeon Park, Seung Whan Doo, Won Jae Yang, Yun Seob Song, Jae Heon Kim
Yonsei Med J. 2019;60(3):257-266. doi: 10.3349/ymj.2019.60.3.257.
Reference
-
1. Welch HG, Black WC. Overdiagnosis in cancer. J Natl Cancer Inst. 2010; 102:605–613.
Article2. Welch HG, Schwartz L, Woloshin S. Overdiagnosed: making people sick in the pursuit of health. Boston: Random House;2011.3. Welch HG, Schwartz LM, Woloshin S. Are increasing 5-year survival rates evidence of success against cancer? JAMA. 2000; 283:2975–2978.
Article4. Gotzsche PC, Hartling OJ, Nielsen M, Brodersen J, Jorgensen KJ. Breast screening: the facts: or maybe not. BMJ. 2009; 338:b86.5. Bach PB. Is our natural-history model of lung cancer wrong? Lancet Oncol. 2008; 9:693–697.
Article6. Ahn HS, Welch HG. South Korea's thyroid-cancer “epidemic”: turning the tide. N Engl J Med. 2015; 373:2389–2390.
Article7. Ezzat S, Sarti DA, Cain DR, Braunstein GD. Thyroid incidentalomas: prevalence by palpation and ultrasonography. Arch Intern Med. 1994; 154:1838–1840.
Article8. Brito JP, Kim HJ, Han SJ, Lee YS, Ahn HS. Geographic distribution and evolution of thyroid cancer epidemic in South Korea. Thyroid. 2016; 26:864–865.
Article9. Udelsman R, Zhang Y. The epidemic of thyroid cancer in the United States: the role of endocrinologists and ultrasounds. Thyroid. 2014; 24:472–479.
Article10. Davies L, Welch HG. Increasing incidence of thyroid cancer in the United States, 1973-2002. JAMA. 2006; 295:2164–2167.
Article11. Harach HR, Franssila KO, Wasenius VM. Occult papillary carcinoma of the thyroid: a “normal” finding in Finland: a systematic autopsy study. Cancer. 1985; 56:531–538.
Article12. Chung JH. Prevalence of thyroid nodules detected by ultrasonography in adults for health check-up and analysis of fine needle aspiration cytology. J Korean Endocr Soc. 2008; 23:391–394.
Article13. Burke JP, Hay ID, Dignan F, Goellner JR, Achenbach SJ, Oberg AL, Melton LJ 3rd. Long-term trends in thyroid carcinoma: a population-based study in Olmsted County, Minnesota, 1935-1999. Mayo Clin Proc. 2005; 80:753–758.
Article14. Kilfoy BA, Zhang Y, Park Y, Holford TR, Schatzkin A, Hollenbeck A, Ward MH. Dietary nitrate and nitrite and the risk of thyroid cancer in the NIH-AARP diet and health Study. Int J Cancer. 2011; 129:160–172.
Article15. Pellegriti G, Frasca F, Regalbuto C, Squatrito S, Vigneri R. Worldwide increasing incidence of thyroid cancer: update on epidemiology and risk factors. J Cancer Epidemiol. 2013; 2013:965212.
Article16. Almquist M, Johansen D, Bjorge T, Ulmer H, Lindkvist B, Stocks T, Hallmans G, Engeland A, Rapp K, Jonsson H, Selmer R, Diem G, Haggstrom C, Tretli S, Stattin P, Manjer J. Metabolic factors and risk of thyroid cancer in the Metabolic syndrome and Cancer project (Me-Can). Cancer Causes Control. 2011; 22:743–751.
Article17. Brito JP, Morris JC, Montori VM. Thyroid cancer: zealous imaging has increased detection and treatment of low risk tumours. BMJ. 2013; 347:f4706.
Article18. Brito JP, Yarur AJ, Prokop LJ, McIver B, Murad MH, Montori VM. Prevalence of thyroid cancer in multinodular goiter versus single nodule: a systematic review and meta-analysis. Thyroid. 2013; 23:449–455.
Article19. Montie JE, Wood DP Jr, Pontes JE, Boyett JM, Levin HS. Adenocarcinoma of the prostate in cystoprostatectomy specimens removed for bladder cancer. Cancer. 1989; 63:381–385.
Article20. Sakr WA, Grignon DJ, Haas GP, Heilbrun LK, Pontes JE, Crissman JD. Age and racial distribution of prostatic intraepithelial neoplasia. Eur Urol. 1996; 30:138–144.21. Thompson IM, Goodman PJ, Tangen CM, Lucia MS, Miller GJ, Ford LG, Lieber MM, Cespedes RD, Atkins JN, Lippman SM, Carlin SM, Ryan A, Szczepanek CM, Crowley JJ, Coltman CA Jr. The influence of finasteride on the development of prostate cancer. N Engl J Med. 2003; 349:215–224.
Article22. Thompson IM Jr, Goodman PJ, Tangen CM, Parnes HL, Minasian LM, Godley PA, Lucia MS, Ford LG. Long-term survival of participants in the prostate cancer prevention trial. N Engl J Med. 2013; 369:603–610.
Article23. Thompson IM, Pauler DK, Goodman PJ, Tangen CM, Lucia MS, Parnes HL, Minasian LM, Ford LG, Lippman SM, Crawford ED, Crowley JJ, Coltman CA Jr. Prevalence of prostate cancer among men with a prostate-specific antigen level < or =4.0 ng per milliliter. N Engl J Med. 2004; 350:2239–2246.
Article24. Zackrisson S, Andersson I, Janzon L, Manjer J, Garne JP. Rate of over-diagnosis of breast cancer 15 years after end of Malmo mammographic screening trial: follow-up study. BMJ. 2006; 332:689–692.25. Welch HG, Black WC. Using autopsy series to estimate the disease “reservoir” for ductal carcinoma in situ of the breast: how much more breast cancer can we find? Ann Intern Med. 1997; 127:1023–1028.
Article26. Welch HG, Robertson DJ. Colorectal cancer on the decline: why screening can't explain it all. N Engl J Med. 2016; 374:1605–1607.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Overdiagnosis: epidemiologic concepts and estimation
- Responses to Overdiagnosis in Thyroid Cancer Screening among Korean Women
- Epidemiological evidences on overdiagnosis of prostate and kidney cancers in Korean
- The Incidence of Thyroid Cancer Is Affected by the Characteristics of a Healthcare System
- Development and application of patient decision aids