Ann Surg Treat Res.
2017 May;92(5):365-369. 10.4174/astr.2017.92.5.365.
Anatomic and clinical risk factors for pulmonary embolism in patients with deep venous thrombosis of the lower extremity
- Affiliations
-
- 1Department of Surgery, Kyung Hee University Hospital at Gangdong, Kyung Hee University School of Medicine, Seoul, Korea. jhjoh@khu.ac.kr
- KMID: 2377708
- DOI: http://doi.org/10.4174/astr.2017.92.5.365
Abstract
- PURPOSE
Iliac vein compression is a known culprit of deep vein thrombosis (DVT). In contrast, the compression may prevent the pulmonary embolism (PE). The aim of this study was to evaluate the anatomic and clinical risk factors of PE in patients with lower extremity DVT.
METHODS
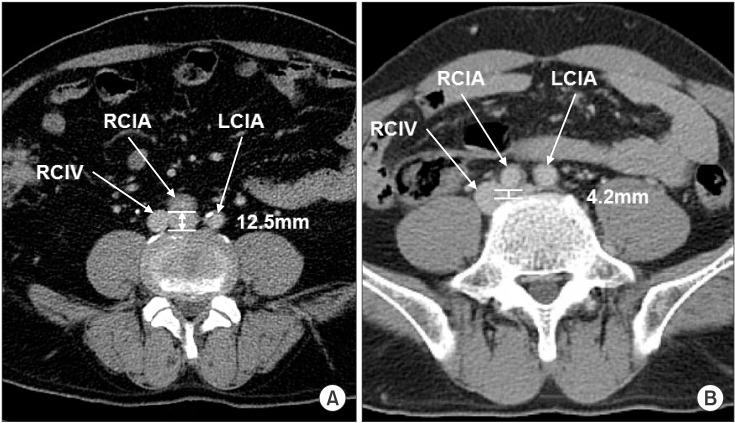
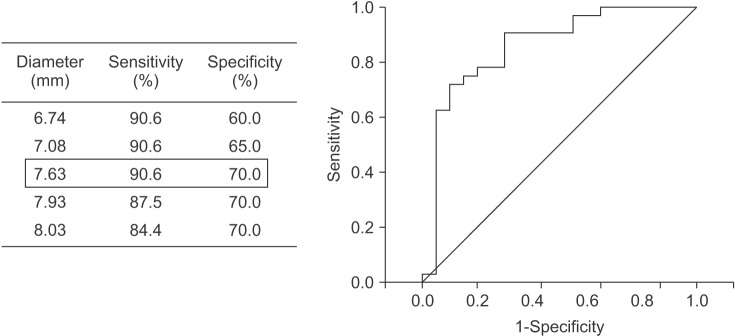
PE was evaluated using chest computed tomography in patients with lower extremity DVT. The patients were classified into group I (DVT without PE) and group II (DVT with PE) and analyzed to clarify the anatomic and clinical risk factors associated with PE in patients with DVT. As the anatomic factor, the shortest length between the common iliac artery (CIA) and spinal body (SB) was measured. Statistical analyses utilized the multivariable logistic regression model, and receiver operating characteristic (ROC) curve analysis.
RESULTS
We examined 114 patients (age; 62.7 ± 16.9 years, 41.7% men) with DVT with/without PE. The prevalence of concurrent DVT with PE was 52.6%. Blood tests showed no difference between the 2 groups. Of all the assessed patients' characteristics, only infection was significantly and independently associated with PE (P = 0.04). The shortest length between CIA and SB was 6.7 ± 3.5 mm in group I and 11.3 ± 3.7 mm in group II (P < 0.001). ROC curve analysis showed that 7.6 mm was the cut-off value for the anatomic risk of PE.
CONCLUSION
Infection was significantly associated with concurrent DVT and PE. The shortest length between CIA and SB (<7.6 mm) may prevent PE in patients with DVT.
Keyword
MeSH Terms
Figure
Reference
-
1. Heit JA. Epidemiology of venous thromboembolism. Nat Rev Cardiol. 2015; 12:464–474. PMID: 26076949.
Article2. Heit JA. Venous thromboembolism: disease burden, outcomes and risk factors. J Thromb Haemost. 2005; 3:1611–1617. PMID: 16102026.
Article3. Jang MJ, Bang SM, Oh D. Incidence of venous thromboembolism in Korea: from the Health Insurance Review and Assessment Service database. J Thromb Haemost. 2011; 9:85–91. PMID: 20942850.
Article4. Meignan M, Rosso J, Gauthier H, Brunengo F, Claudel S, Sagnard L, et al. Systematic lung scans reveal a high frequency of silent pulmonary embolism in patients with proximal deep venous thrombosis. Arch Intern Med. 2000; 160:159–164. PMID: 10647753.
Article5. Stein PD, Matta F, Musani MH, Diaczok B. Silent pulmonary embolism in patients with deep venous thrombosis: a systematic review. Am J Med. 2010; 123:426–431. PMID: 20399319.
Article6. Fraser DG, Moody AR, Martel A, Morgan PS. Re-evaluation of iliac compression syndrome using magnetic resonance imaging in patients with acute deep venous thromboses. J Vasc Surg. 2004; 40:604–611. PMID: 15472584.
Article7. Chan KT, Popat RA, Sze DY, Kuo WT, Kothary N, Louie JD, et al. Common iliac vein stenosis and risk of symptomatic pulmonary embolism: an inverse correlation. J Vasc Interv Radiol. 2011; 22:133–141. PMID: 21276911.
Article8. Epaulard O, Foote A, Bosson JL. Chronic Infection and Venous Thromboembolic Disease. Semin Thromb Hemost. 2015; 41:644–649. PMID: 26313667.
Article9. Obi AT, Pannucci CJ, Nackashi A, Abdullah N, Alvarez R, Bahl V, et al. Validation of the caprini venous thromboembolism risk assessment model in critically Ill surgical patients. JAMA Surg. 2015; 150:941–948. PMID: 26288124.
Article10. Smeeth L, Cook C, Thomas S, Hall AJ, Hubbard R, Vallance P. Risk of deep vein thrombosis and pulmonary embolism after acute infection in a community setting. Lancet. 2006; 367:1075–1079. PMID: 16581406.
Article11. Song Y, Wang L, Yang F, Wu X, Duan Q, Gong Z. Increased expressions of integrin subunit β1, β2 and β3 in patients with acute infection. Int J Med Sci. 2015; 12:639–643. PMID: 26283883.
Article12. Song Y, Yang F, Wang L, Duan Q, Jin Y, Gong Z. Increased expressions of integrin subunit β1, β2 and β3 in patients with venous thromboembolism: new markers for venous thromboembolism. Int J Clin Exp Med. 2014; 7:2578–2584. PMID: 25356112.13. Alikhan R, Cohen AT, Combe S, Samama MM, Desjardins L, Eldor A, et al. Risk factors for venous thromboembolism in hospitalized patients with acute medical illness: analysis of the MEDENOX Study. Arch Intern Med. 2004; 164:963–968. PMID: 15136304.14. Cha SI, Choi KJ, Shin KM, Lim JK, Yoo SS, Lee J, et al. Clinical characteristics of pulmonary embolism with concomitant pneumonia. Blood Coagul Fibrinolysis. 2016; 27:281–286. PMID: 26366829.
Article15. Zhang Y, Zhou Q, Zou Y, Song X, Xie S, Tan M, et al. Risk factors for pulmonary embolism in patients preliminarily diagnosed with community-acquired pneumonia: a prospective cohort study. J Thromb Thrombolysis. 2016; 41:619–627. PMID: 26370200.
Article16. Carr S, Chan K, Rosenberg J, Kuo WT, Kothary N, Hovsepian DM, et al. Correlation of the diameter of the left common iliac vein with the risk of lower-extremity deep venous thrombosis. J Vasc Interv Radiol. 2012; 23:1467–1472. PMID: 23101919.
Article17. Forauer AR, Gemmete JJ, Dasika NL, Cho KJ, Williams DM. Intravascular ultrasound in the diagnosis and treatment of iliac vein compression (May-Thurner) syndrome. J Vasc Interv Radiol. 2002; 13:523–527. PMID: 11997362.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Upper Extremity Deep Vein Thrombosis and Pulmonary Thromboembolism in a Severely Obese Man
- Clinical Year in Review of Venous Thromboembolism
- The Incidence of Deep Vein Thrombosis in the Lower Extremity
- Management of Venous Thrombosis in Atypical Location
- Risk Factors and Prophylactic Anticoagulation Therapy of Deep Vein Thrombosis in Lower Extremity