J Korean Fract Soc.
2017 Apr;30(2):89-101. 10.12671/jkfs.2017.30.2.89.
Treatment Options for the Nonunions with Critical Sized Bone Loss
- Affiliations
-
- 1Department of Orthopedic Surgery, Korea University Guro Hospital, Seoul, Korea. jkoh@korea.ac.kr
- KMID: 2376615
- DOI: http://doi.org/10.12671/jkfs.2017.30.2.89
Abstract
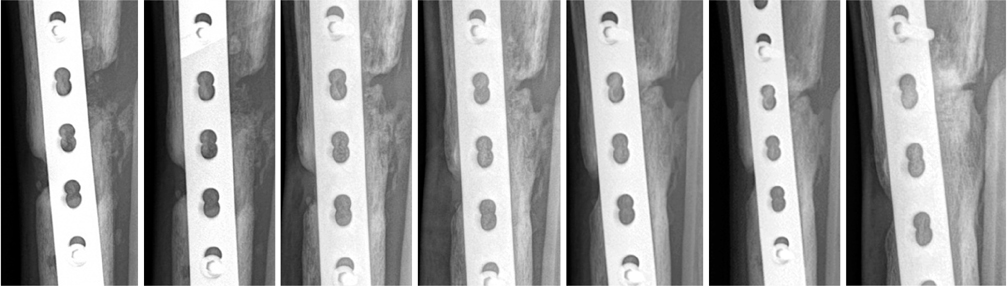
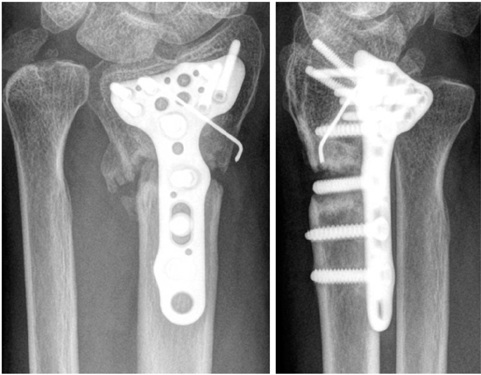
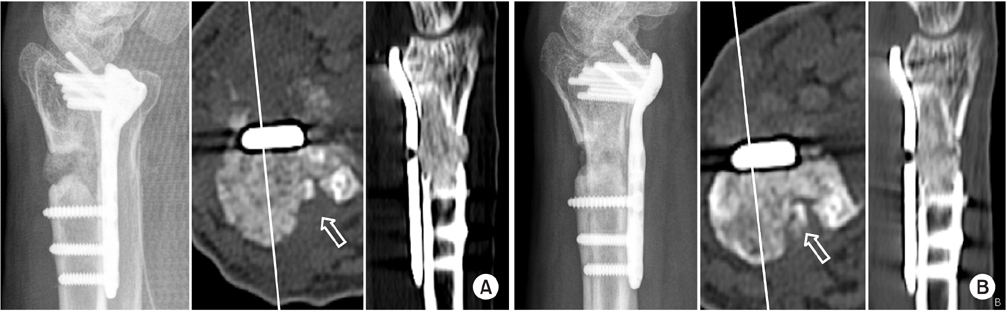
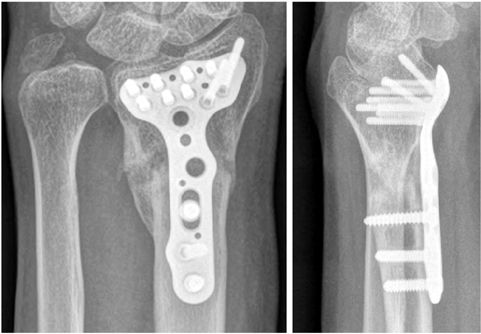
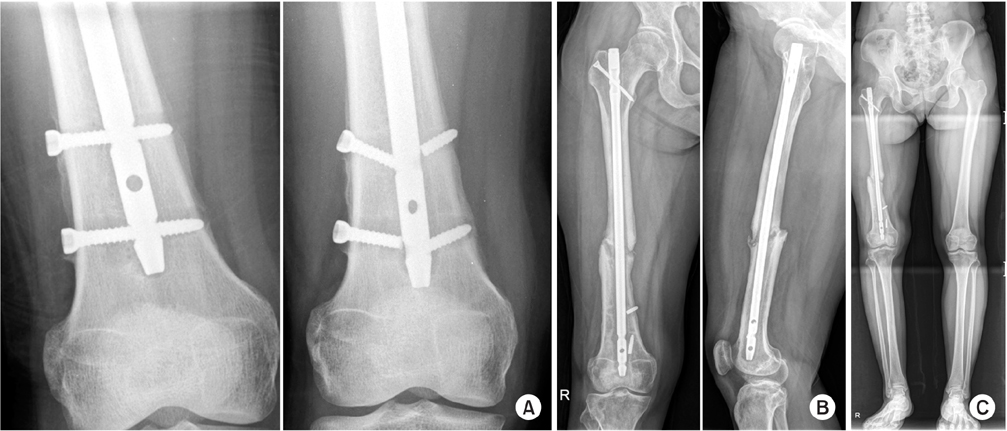
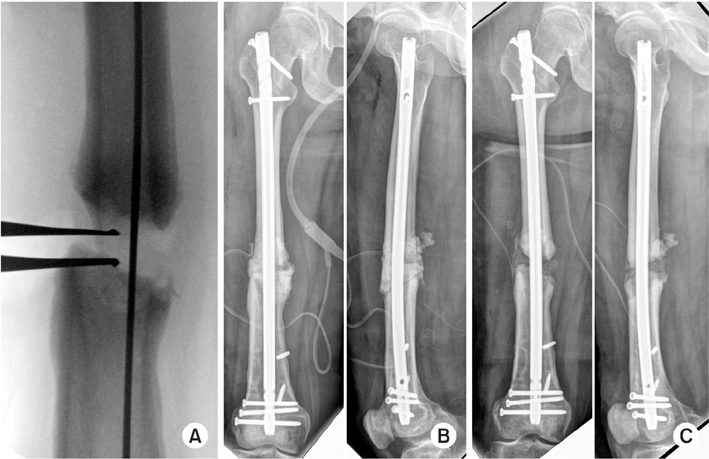
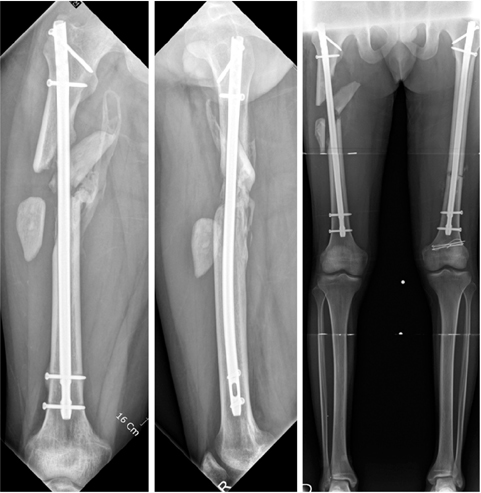
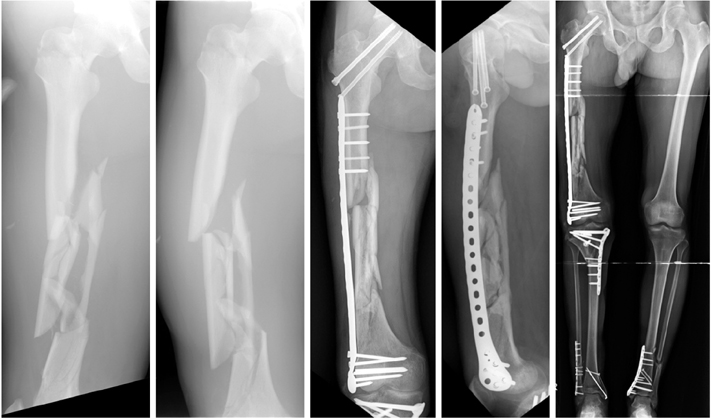
- The management of nonunion with severe bone loss is a challenging task to both surgeons and patients. It often requires prolonged and potentially painful treatments. Moreover, it also represents serious socioeconomic issues for patients. Inadequate fracture stability, disrupted biology, such as blood supply and soft tissue, as well as severe bone loss or presence of infection are possible reasons for nonunion. Several different treatment modalities are available, including nail dynamization, plate osteosynthesis, exchange nailing, and adjuvant alternatives, such as electrical or ultrasound stimulation. Autogenous bone graft remains the standard method to reconstruct small defects. Distraction osteogenesis and induced membrane techniques are contemporary strategies of choice for the reconstruction of larger bony defects. Herein, we attempt to describe the key techniques that may be employed in treating nonunion with severe bone loss.
Figure
Reference
-
1. Ryaby JT. Clinical effects of electromagnetic and electric fieldson fracture healing. Clin Orthop Relat Res. 1998; 355 Suppl. S205–S215.2. Boyd HB. Symposium: treatment of ununited fractures of the long bones; introduction. J Bone Joint Surg Am. 1965; 47:167–168.3. Connolly JF. Common avoidable problems in nonunions. Clin Orthop Relat Res. 1985; (194):226–235.
Article4. Heckman JD, Sarasohn-Kahn J. The economics of treating tibia fractures. The cost of delayed unions. Bull Hosp Jt Dis. 1997; 56:63–72.5. Bishop JA, Palanca AA, Bellino MJ, Lowenberg DW. Assessment of compromised fracture healing. J Am Acad Orthop Surg. 2012; 20:273–282.
Article6. Services DoHaH. Medicare claims processing manual. Baltimore: Centers for Medicare & Medicaid Services;2010.7. Sanders DW, Bhandari M, Guyatt G, et al. Critical-sized defect in the tibia: is it critical? Results from the SPRINT trial. J Orthop Trauma. 2014; 28:632–635.8. Jones AL, Bucholz RW, Bosse MJ, et al. Recombinant human BMP-2 and allograft compared with autogenous bone graft for reconstruction of diaphyseal tibial fractures with cortical defects. A randomized, controlled trial. J Bone Joint Surg Am. 2006; 88:1431–1441.
Article9. Oh JK, Hwang JH, Lee SJ, Kim JI. Dynamization of locked plating on distal femur fracture. Arch Orthop Trauma Surg. 2011; 131:535–539.
Article10. Dreiseidler T, Kaunisaho V, Neugebauer J, Zöller JE, Rothamel D, Kreppel M. Changes in volume during the four months' remodelling period of iliac crest grafts in reconstruction of the alveolar ridge. Br J Oral Maxillofac Surg. 2016; 54:751–756.
Article11. Sbordone L, Toti P, Menchini-Fabris GB, Sbordone C, Piombino P, Guidetti F. Volume changes of autogenous bone grafts after alveolar ridge augmentation of atrophic maxillae and mandibles. Int J Oral Maxillofac Surg. 2009; 38:1059–1065.
Article12. Macey LR, Kana SM, Jingushi S, Terek RM, Borretos J, Bolander ME. Defects of early fracture-healing in experimental diabetes. J Bone Joint Surg Am. 1989; 71:722–733.
Article13. Oh JK, Bae JH, Oh CW, Biswal S, Hur CR. Treatment of femoral and tibial diaphyseal nonunions using reamed intramedullary nailing without bone graft. Injury. 2008; 39:952–959.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ilizarov Method for Treatment of Tibia Nonunion Associated with Bone Defects
- The Treatment of Infected Nonunions of Femur using Sequestrectomy and Distraction Osteogenesis
- The Treatment of Infected Nonunions of the Tibia by the Methods of Ilizarov
- Treatment of Femoral Shaft Nonunions with Dynamic Compression using Interlocking-Compression (IC) Nail
- The Operative Treatment of Nonunions of Midshaft Clavicular Fractures: Reconstruction Plate Fixation and Bone Grafting