Tuberc Respir Dis.
2017 Apr;80(2):159-168. 10.4046/trd.2017.80.2.159.
Mutations in Streptomycin Resistance Genes and Their Relationship to Streptomycin Resistance and Lineage of Mycobacterium tuberculosis Thai Isolates
- Affiliations
-
- 1Graduate Program in Biomedical Sciences, Faculty of Allied Health Sciences, Thammasat University, Pathumthani, Thailand. Spotjane@tu.ac.th
- 2Bamrasnaradura Infectious Diseases Institute, Nonthaburi, Thailand.
- KMID: 2375985
- DOI: http://doi.org/10.4046/trd.2017.80.2.159
Abstract
- BACKGROUND
Streptomycin (SM) is recommended by the World Health Organization (WHO) as a part of standard regimens for retreating multidrug-resistant tuberculosis (MDR-TB) cases. The incidence of MDR-TB in retreatment cases was 19% in Thailand. To date, information on SM resistance (SMR) gene mutations correlated to the SMR of Mycobacterium tuberculosis Thai isolates is limited. In this study, the mutations in rpsL, rrs, gidB, and whiB7 were investigated and their association to SMR and the lineage of M. tuberculosis were explored.
METHODS
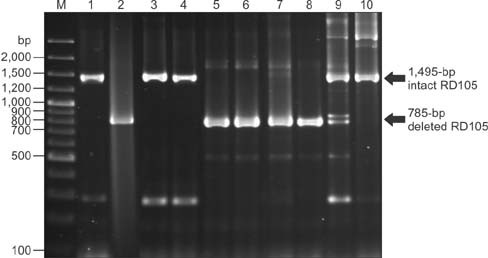
The lineages of 287 M. tuberculosis collected from 2007 to 2011 were identified by spoligotyping. Drug susceptibility profiles were evaluated by the absolute concentration method. Mutations in SMR genes of 46 SM-resistant and 55 SM-susceptible isolates were examined by DNA sequencing.
RESULTS
Three rpsL (Lys43Arg, Lys88Arg, and Lys88Thr) and two gidB (Trp45Ter and Gly69Asp) mutations were present exclusively in the SM resistant M. tuberculosis. Lys43Arg rpsL was the most predominant SMR mutations (69.6%) and prevailed among Beijing isolates (p<0.001). No SMR-related mutation in was found rrs. The combination of rpsL and gidB mutations provided 76.1% sensitivity for detecting SMR in M. tuberculosis Thai isolates. whiB7 was not responsible for SMR in SM resistant isolates lacking rpsL and rrs mutations. The significance of the three gidB mutations, 276A>C, 615A>G, and 330G>T, as lineage signatures for Beijing and EAI were underscored. This study identified 423G>A gidB as a novel sub-lineage marker for EAI6-BGD1.
CONCLUSION
Our study suggested that the majority of SMR in M. tuberculosis Thai isolates were responsible by rpsL and gidB polymorphisms constantly providing the novel lineage specific makers.
Keyword
MeSH Terms
Figure
Reference
-
1. World Health Organization. Treatment of tuberculosis guidelines. 4th ed. WHO/HTM [Internet]. Geneva: World Health Organization;2010. cited 2015 Oct 12. Available from: http://www.who.int/tb/publications/2010/9789241547833/en/.2. Carter AP, Clemons WM, Brodersen DE, Morgan-Warren RJ, Wimberly BT, Ramakrishnan V. Functional insights from the structure of the 30S ribosomal subunit and its interactions with antibiotics. Nature. 2000; 407:340–348.3. Meier A, Sander P, Schaper KJ, Scholz M, Bottger EC. Correlation of molecular resistance mechanisms and phenotypic resistance levels in streptomycin-resistant Mycobacterium tuberculosis. Antimicrob Agents Chemother. 1996; 40:2452–2454.4. Zhang Y, Yew WW. Mechanisms of drug resistance in Mycobacterium tuberculosis. Int J Tuberc Lung Dis. 2009; 13:1320–1330.5. Okamoto S, Tamaru A, Nakajima C, Nishimura K, Tanaka Y, Tokuyama S, et al. Loss of a conserved 7-methylguanosine modification in 16S rRNA confers low-level streptomycin resistance in bacteria. Mol Microbiol. 2007; 63:1096–1106.6. Spies FS, Ribeiro AW, Ramos DF, Ribeiro MO, Martin A, Palomino JC, et al. Streptomycin resistance and lineage-specific polymorphisms in Mycobacterium tuberculosis gidB gene. J Clin Microbiol. 2011; 49:2625–2630.7. Zhao LL, Liu HC, Sun Q, Xiao TY, Zhao XQ, Li GL, et al. Identification of mutations conferring streptomycin resistance in multidrug-resistant tuberculosis of China. Diagn Microbiol Infect Dis. 2015; 83:150–153.8. Smittipat N, Juthayothin T, Billamas P, Jaitrong S, Rukseree K, Dokladda K, et al. Mutations in rrs, rpsL and gidB in streptomycin-resistant Mycobacterium tuberculosis isolates from Thailand. J Glob Antimicrob Resist. 2016; 4:5–10.9. Morris RP, Nguyen L, Gatfield J, Visconti K, Nguyen K, Schnappinger D, et al. Ancestral antibiotic resistance in Mycobacterium tuberculosis. Proc Natl Acad Sci U S A. 2005; 102:12200–12205.10. Reeves AZ, Campbell PJ, Sultana R, Malik S, Murray M, Plikaytis BB, et al. Aminoglycoside cross-resistance in Mycobacterium tuberculosis due to mutations in the 5’ untranslated region of whiB7. Antimicrob Agents Chemother. 2013; 57:1857–1865.11. Villellas C, Aristimuno L, Vitoria MA, Prat C, Blanco S, Garcia de Viedma D, et al. Analysis of mutations in streptomycin-resistant strains reveals a simple and reliable genetic marker for identification of the Mycobacterium tuberculosis Beijing genotype. J Clin Microbiol. 2013; 51:2124–2130.12. World Health Organization. Global tuberculosis report 2015. WHO/HTM/TB/2015.22 [Internet]. Geneva: World Health Organization;2015. cited 2015 Nov 20. Available from: http://www.who.int/tb/publications/global_report/en/.13. World Health Organization. Companion handbook to the WHO guidelines for the programmatic management of drug-resistant tuberculosis. WHO/HTM/TB/2014.11 [Internet]. Geneva: World Health Organization;2014. cited 2014 Oct 12. Available from: http://www.who.int/tb/publications/pmdt_companionhandbook/en/.14. Kamerbeek J, Schouls L, Kolk A, van Agterveld M, van Soolingen D, Kuijper S, et al. Simultaneous detection and strain differentiation of Mycobacterium tuberculosis for diagnosis and epidemiology. J Clin Microbiol. 1997; 35:907–914.15. TB-Insight. About TB-Lineage [Internet]. TB Insight;2015. cited 2015 Nov 28. Available from: http://tbinsight.cs.rpi.edu/about_tb_lineage.html.16. van Soolingen D, Hermans PW, de Haas PE, Soll DR, van Embden JD. Occurrence and stability of insertion sequences in Mycobacterium tuberculosis complex strains: evaluation of an insertion sequence-dependent DNA polymorphism as a tool in the epidemiology of tuberculosis. J Clin Microbiol. 1991; 29:2578–2586.17. Meier A, Kirschner P, Bange FC, Vogel U, Bottger EC. Genetic alterations in streptomycin-resistant Mycobacterium tuberculosis: mapping of mutations conferring resistance. Antimicrob Agents Chemother. 1994; 38:228–233.18. Springer B, Stockman L, Teschner K, Roberts GD, Bottger EC. Two-laboratory collaborative study on identification of mycobacteria: molecular versus phenotypic methods. J Clin Microbiol. 1996; 34:296–303.19. Via LE, Cho SN, Hwang S, Bang H, Park SK, Kang HS, et al. Polymorphisms associated with resistance and cross-resistance to aminoglycosides and capreomycin in Mycobacterium tuberculosis isolates from South Korean patients with drug-resistant tuberculosis. J Clin Microbiol. 2010; 48:402–411.20. Sowajassatakul A, Prammananan T, Chaiprasert A, Phunpruch S. Molecular characterization of amikacin, kanamycin and capreomycin resistance in M/XDR-TB strains isolated in Thailand. BMC Microbiol. 2014; 14:165.21. Chen J, Tsolaki AG, Shen X, Jiang X, Mei J, Gao Q. Deletion-targeted multiplex PCR (DTM-PCR) for identification of Beijing/W genotypes of Mycobacterium tuberculosis. Tuberculosis (Edinb). 2007; 87:446–449.22. BLAST. Basic Local Alignment Search Tool [Internet]. Bethesda: National Center for Biotechnology Information;2015. cited 2015 Feb 4. Available from: http://blast.ncbi.nlm.nih.gov/Blast.cgi.23. Lee AS, Ong DC, Wong JC, Siu GK, Yam WC. High-resolution melting analysis for the rapid detection of fluoroquinolone and streptomycin resistance in Mycobacterium tuberculosis. PLoS One. 2012; 7:e31934.24. Morita M, Ohnishi M, Arakawa E, Bhuiyan NA, Nusrin S, Alam M, et al. Development and validation of a mismatch amplification mutation PCR assay to monitor the dissemination of an emerging variant of Vibrio cholerae O1 biotype El Tor. Microbiol Immunol. 2008; 52:314–317.25. Wan X, Qian L, Hou S, Drees KP, Foster JT, Douglas JT. Complete genome sequences of Beijing and Manila family strains of Mycobacterium tuberculosis. Genome Announc. 2014; 2:e01135–e01114.26. Kornder JD. Streptomycin revisited: molecular action in the microbial cell. Med Hypotheses. 2002; 58:34–46.27. Nhu NT, Lan NT, Phuong NT, Chau N, Farrar J, Caws M. Association of streptomycin resistance mutations with level of drug resistance and Mycobacterium tuberculosis genotypes. Int J Tuberc Lung Dis. 2012; 16:527–531.28. Sun YJ, Luo JT, Wong SY, Lee AS. Analysis of rpsL and rrs mutations in Beijing and non-Beijing streptomycin-resistant Mycobacterium tuberculosis isolates from Singapore. Clin Microbiol Infect. 2010; 16:287–289.29. Van Rie A, Warren R, Mshanga I, Jordaan AM, van der Spuy GD, Richardson M, et al. Analysis for a limited number of gene codons can predict drug resistance of Mycobacterium tuberculosis in a high-incidence community. J Clin Microbiol. 2001; 39:636–641.30. Siddiqi N, Shamim M, Hussain S, Choudhary RK, Ahmed N, Prachee , et al. Molecular characterization of multidrug-resistant isolates of Mycobacterium tuberculosis from patients in North India. Antimicrob Agents Chemother. 2002; 46:443–450.31. Feuerriegel S, Oberhauser B, George AG, Dafae F, Richter E, Rusch-Gerdes S, et al. Sequence analysis for detection of first-line drug resistance in Mycobacterium tuberculosis strains from a high-incidence setting. BMC Microbiol. 2012; 12:90.32. Jnawali HN, Hwang SC, Park YK, Kim H, Lee YS, Chung GT, et al. Characterization of mutations in multi- and extensive drug resistance among strains of Mycobacterium tuberculosis clinical isolates in Republic of Korea. Diagn Microbiol Infect Dis. 2013; 76:187–196.33. Tudo G, Rey E, Borrell S, Alcaide F, Codina G, Coll P, et al. Characterization of mutations in streptomycin-resistant Mycobacterium tuberculosis clinical isolates in the area of Barcelona. J Antimicrob Chemother. 2010; 65:2341–2346.34. Ramaswamy SV, Dou SJ, Rendon A, Yang Z, Cave MD, Graviss EA. Genotypic analysis of multidrug-resistant Mycobacterium tuberculosis isolates from Monterrey, Mexico. J Med Microbiol. 2004; 53(Pt 2):107–113.35. Jagielski T, Ignatowska H, Bakula Z, Dziewit L, Napiorkowska A, Augustynowicz-Kopec E, et al. Screening for streptomycin resistance-conferring mutations in Mycobacterium tuberculosis clinical isolates from Poland. PLoS One. 2014; 9:e100078.36. Comas I, Homolka S, Niemann S, Gagneux S. Genotyping of genetically monomorphic bacteria: DNA sequencing in Mycobacterium tuberculosis highlights the limitations of current methodologies. PLoS One. 2009; 4:e7815.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Development of Oligonucleotide Chip for Detection of Drug-Resistant Mycobacterium Tuberculosis
- An Alternative Approach to Tuberculosis Management with Intravenous Streptomycin
- Detection of Antibiotic Resistant Genes in Salmonella enterica Serovar Typhimurium Isolated from Foodborne Patients in Seoul Using Multiplex-PCR
- Rapid Detection of Rifampin Resistant Mycobacterium tuberculosis Using the Line Probe Assay
- Molecular analysis of katG gene mutations in strains of Mycobacterium tuberculosis from Korea