Korean J Endocr Surg.
2011 Dec;11(4):276-282. 10.0000/kjes.2011.11.4.276.
Postoperative Outcomes in Patients Undergoing Adrenalectomy for Primary Aldosteronism
- Affiliations
-
- 1Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. jhkim15@skku.edu
- 2Department of Surgery, Konkuk University School of Medicine, Seoul, Korea.
- KMID: 2375390
- DOI: http://doi.org/10.0000/kjes.2011.11.4.276
Abstract
- PURPOSE
Primary aldosteronism (PA) is characterized by hypertension (HTN), hypokalemia, suppressed plasma renin activity, and inappropriate aldosterone secretion. The purpose of this study was to analyze postoperative results on blood pressure (BP), and to determine the factors associated with resolution of HTN after adrenalectomy for PA.
METHODS
One hundred eight patients (66 females and 42 males) with a mean age of 46 years underwent adrenalectomy for PA between January 1, 1996 and September 30, 2009. Their clinical characteristics and biochemical parameters were reviewed retrospectively.
RESULTS
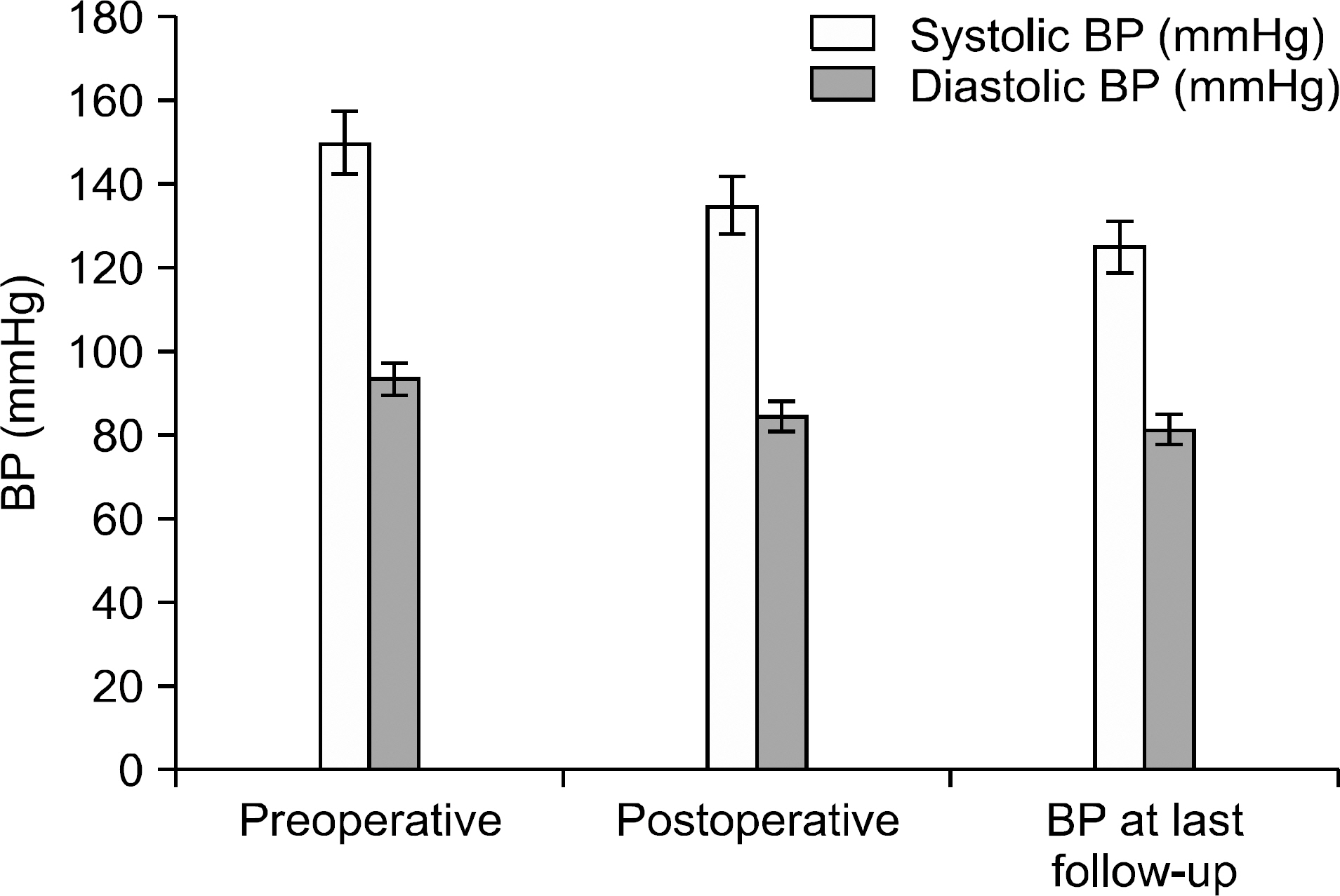
All patients had HTN preoperatively and 20 patients (18.1%) had uncontrolled HTN. Hypokalemia was evident in 89.1% of patients, cardiovascular events in 4.5% and cerebrovascular events in 8.2%. There was a significant decrease in both systolic BP and diastolic BP postoperatively, as compared with that before operation. Median systolic BP decreased from 150 mmHg to 125 mmHg at the last follow-up (P<0.01), and median diastolic BP decreased from 93.5 mmHg to 81.5 mmHg (P<0.01). Sixty two (57.4%) patients were cured of HTN and did not require any hypertensive agent, and 38 (35.1%) patients had an improvement in BP control, whereas 9 (8.3%) patients had no change in BP. Univariate analysis showed that duration of HTN and more than two HTN treatment agents were independent factors predicting sustained hypertension after surgery.
CONCLUSION
The duration of HTN and the severity of HTN are factors influencing persistence of HTN after operation for a PA.
MeSH Terms
Figure
Reference
-
1.Conn JW., Louis LH. Primary aldosteronism, a new clinical entity. Ann Intern Med. 1956. 44:1–15.
Article2.Giacchetti G., Ronconi V., Lucarelli G., Boscaro M., Mantero F. Analysis of screening and confirmatory tests in the diagnosis of primary aldosteronism: need for a standardized protocol. J Hypertens. 2006. 24:737–45.
Article3.Plouin PF., Amar L., Chatellier G. Trends in the prevalence of primary aldosteronism, aldosterone-producing adenomas, and surgically correctable aldosterone-dependent hypertension. Nephrol Dial Transplant. 2004. 19:774–7.
Article4.Mulatero P., Stowasser M., Loh KC., Fardella CE., Gordon RD., Mosso L, et al. Increased diagnosis of primary aldosteronism, including surgically correctable forms, in centers from five continents. J Clin Endocrinol Metab. 2004. 89:1045–50.
Article5.Campagnacci R., Crosta F., De Sanctis A., Baldarelli M., Giacchetti G., Paganini AM, et al. Long-term results of laparoscopic adrenalectomy for primary aldosteronism. J Endocrinol Invest. 2009. 32:57–62.
Article6.Fowler DL. Laparoscopic adrenalectomy: there can be no doubt. Ann Surg Oncol. 2003. 10:997–8.
Article7.Gockel I., Heintz A., Polta M., Junginger T. Long-term results of endoscopic adrenalectomy for Conn's syndrome. Am Surg. 2007. 73:174–80.
Article8.Goh BK., Tan YH., Yip SK., Eng PH., Cheng CW. Outcome of patients undergoing laparoscopic adrenalectomy for primary hyperaldosteronism. JSLS. 2004. 8:320–5.9.Gordon RD. Mineralocorticoid hypertension. Lancet. 1994. 344:240–3.
Article10.Rizzoni D., Porteri E., Castellano M., Bettoni G., Muiesan ML., Muiesan P, et al. Vascular hypertrophy and remodeling in secondary hypertension. Hypertension. 1996. 28:785–90.
Article11.Strauch B., Petrák O., Zelinka T., Wichterle D., Holaj R., Kasalický M, et al. Adrenalectomy improves arterial stiffness in primary aldosteronism. Am J Hypertens. 2008. 21:1086–92.
Article12.Funder JW., Carey RM., Fardella C., Gomez-Sanchez CE., Mantero F., Stowasser M, et al. Case detection, diagnosis, and treatment of patients with primary aldosteronism: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2008. 93:3266–81.
Article13.Nishizaka MK., Pratt-Ubunama M., Zaman MA., Cofield S., Calhoun DA. Validity of plasma aldosterone-to-renin activity ratio in African American and white subjects with resistant hypertension. Am J Hypertens. 2005. 18:805–12.
Article14.Catena C., Colussi G., Nadalini E., Chiuch A., Baroselli S., Lapenna R, et al. Cardiovascular outcomes in patients with primary aldosteronism after treatment. Arch Intern Med. 2008. 168:80–5.15.Milliez P., Girerd X., Plouin PF., Blacher J., Safar ME., Mourad JJ. Evidence for an increased rate of cardiovascular events in patients with primary aldosteronism. J Am Coll Cardiol. 2005. 45:1243–8.
Article16.Rocha R., Stier CT Jr. Pathophysiological effects of aldosterone in cardiovascular tissues. Trends Endocrinol Metab. 2001. 12:308–14.
Article17.Sechi LA., Novello M., Lapenna R., Baroselli S., Nadalini E., Colussi GL, et al. Long-term renal outcomes in patients with primary aldosteronism. JAMA. 2006. 295:2638–45.
Article18.Blumenfeld JD., Sealey JE., Schlussel Y., Vaughan ED Jr., Sos TA., Atlas SA, et al. Diagnosis and treatment of primary hyperaldosteronism. Ann Intern Med. 1994. 121:877–85.
Article19.Obara T., Ito Y., Okamoto T., Kanaji Y., Yamashita T., Aiba M, et al. Risk factors associated with postoperative persistent hypertension in patients with primary aldosteronism. Surgery. 1992. 112:987–93.20.Sawka AM., Young WF., Thompson GB., Grant CS., Farley DR., Leibson C, et al. Primary aldosteronism: factors associated with normalization of blood pressure after surgery. Ann Intern Med. 2001. 135:258–61.
Article21.Giacchetti G., Ronconi V., Rilli S., Guerrieri M., Turchi F., Boscaro M. Small tumor size as favorable prognostic factor after adrenalectomy in Conn's adenoma. Eur J Endocrinol. 2009. 160:639–46.
Article22.Meyer A., Brabant G., Behrend M. Long-term follow-up after adrenalectomy for primary aldosteronism. World J Surg. 2005. 29:155–9.
Article23.Fukudome Y., Fujii K., Arima H., Ohya Y., Tsuchihashi T., Abe I, et al. Discriminating factors for recurrent hypertension in patients with primary aldosteronism after adrenalectomy. Hypertens Res. 2002. 25:11–8.
Article24.TAIPAI Study Group. Wu VC., Chueh SC., Chang HW., Lin LY., Liu KL., Lin YH, et al. Association of kidney function with residual hypertension after treatment of aldosterone -producing adenoma. Am J Kidney Dis. 2009. 54:665–73.25.Young WF., Stanson AW., Thompson GB., Grant CS., Farley DR., van Heerden JA. Role for adrenal venous sampling in primary aldosteronism. Surgery. 2004. 136:1227–35.
Article26.Auchus RJ., Wians FH Jr., Anderson ME., Dolmatch BL., Trimmer CK., Josephs SC, et al. What we still do not know about adrenal vein sampling for primary aldosteronism. Horm Metab Res. 2010. 42:411–5.
Article27.Sukor N., Gordon RD., Ku YK., Jones M., Stowasser M. Role of unilateral adrenalectomy in bilateral primary aldosteronism: a 22-year single center experience. J Clin Endocrinol Metab. 2009. 94:2437–45.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors Associated with Resolution of Hypertension after Adrenalectomy in Patients with Primary Aldosteronism
- Factors Influencing the Outcomes of Operations for Adrenal Hypertention
- Anesthetic Experience of Adrenalectomy with Primary Aldosteronism
- Primary Aldosteronism: An Anesthetic Experience with Adrenalectomy
- Hypertension Controlled by Adrenalectomy: A Case of Primary Aldosteronism