Endocrinol Metab.
2018 Sep;33(3):355-363. 10.3803/EnM.2018.33.3.355.
Factors Associated with Resolution of Hypertension after Adrenalectomy in Patients with Primary Aldosteronism
- Affiliations
-
- 1Department of Endocrinology, Changi General Hospital, SingHealth, Singapore. wann_jia_loh@cgh.com.sg
- 2Department of Endocrinology, Singapore General Hospital, SingHealth, Singapore.
- KMID: 2447025
- DOI: http://doi.org/10.3803/EnM.2018.33.3.355
Abstract
- BACKGROUND
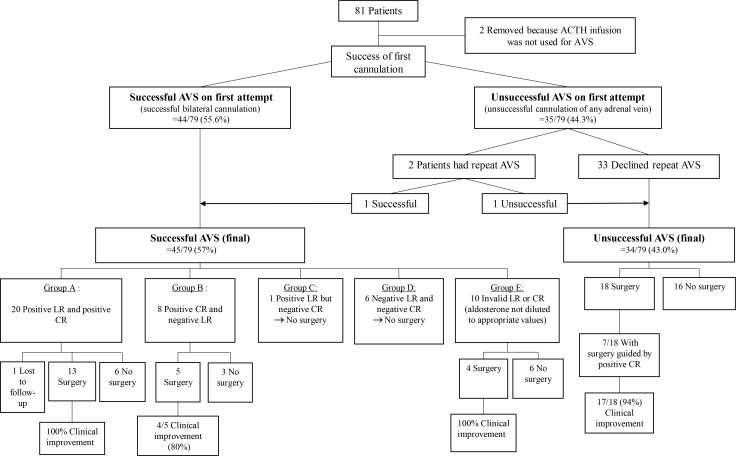
The aim of this study was to investigate the factors associated with resolution of hypertension after adrenalectomy in patients with primary aldosteronism. A secondary aim was to describe our use of the contralateral ratio in adrenal venous sampling (AVS) in the setting of suboptimal successful cannulation rates.
METHODS
A retrospective review of patients who underwent AVS followed by unilateral adrenalectomy for primary aldosteronism was performed.
RESULTS
Complete resolution of hypertension and hypokalemia was seen in 17 of 40 patients (42.5%), while a clinical improvement in hypertension was seen in 38 of 40 (95%). Shorter duration of hypertension, mean aldosteronoma resolution score (ARS), and a high ARS of 3 to 5 were associated with resolution of hypertension after adrenalectomy (P=0.02, P=0.02, and P=0.004, respectively). Of the individual components of ARS, only a duration of hypertension of ≤6 years was associated with resolution of hypertension after adrenalectomy (P=0.03).
CONCLUSION
A shorter duration of hypertension was significantly associated with resolution of hypertension after adrenalectomy in patients with primary aldosteronism.
MeSH Terms
Figure
Cited by 1 articles
-
Update on the Aldosterone Resolution Score and Lateralization in Patients with Primary Aldosteronism
Eun-Hee Cho
Endocrinol Metab. 2018;33(3):352-354. doi: 10.3803/EnM.2018.33.3.352.
Reference
-
1. Rossi GP, Bernini G, Caliumi C, Desideri G, Fabris B, Ferri C, et al. A prospective study of the prevalence of primary aldosteronism in 1,125 hypertensive patients. J Am Coll Cardiol. 2006; 48:2293–2300. PMID: 17161262.
Article2. Lim PO, Rodgers P, Cardale K, Watson AD, MacDonald TM. Potentially high prevalence of primary aldosteronism in a primary-care population. Lancet. 1999; 353:40.
Article3. Kumar A, Lall SB, Ammini A, Peshin SS, Karmarkar MG, Talwar KK, et al. Screening of a population of young hypertensives for primary hyperaldosteronism. J Hum Hypertens. 1994; 8:731–732. PMID: 7807506.4. Gordon RD, Stowasser M, Tunny TJ, Klemm SA, Rutherford JC. High incidence of primary aldosteronism in 199 patients referred with hypertension. Clin Exp Pharmacol Physiol. 1994; 21:315–318. PMID: 7923898.
Article5. Loh KC, Koay ES, Khaw MC, Emmanuel SC, Young WF Jr. Prevalence of primary aldosteronism among Asian hypertensive patients in Singapore. J Clin Endocrinol Metab. 2000; 85:2854–2859. PMID: 10946893.
Article6. Rossi GP, Sechi LA, Giacchetti G, Ronconi V, Strazzullo P, Funder JW. Primary aldosteronism: cardiovascular, renal and metabolic implications. Trends Endocrinol Metab. 2008; 19:88–90. PMID: 18314347.
Article7. Milliez P, Girerd X, Plouin PF, Blacher J, Safar ME, Mourad JJ. Evidence for an increased rate of cardiovascular events in patients with primary aldosteronism. J Am Coll Cardiol. 2005; 45:1243–1248. PMID: 15837256.
Article8. Young WF, Stanson AW, Thompson GB, Grant CS, Farley DR, van Heerden JA. Role for adrenal venous sampling in primary aldosteronism. Surgery. 2004; 136:1227–1235. PMID: 15657580.
Article9. Funder JW, Carey RM, Fardella C, Gomez-Sanchez CE, Mantero F, Stowasser M, et al. Case detection, diagnosis, and treatment of patients with primary aldosteronism: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2008; 93:3266–3281. PMID: 18552288.
Article10. Rossi GP, Auchus RJ, Brown M, Lenders JW, Naruse M, Plouin PF, et al. An expert consensus statement on use of adrenal vein sampling for the subtyping of primary aldosteronism. Hypertension. 2014; 63:151–160. PMID: 24218436.
Article11. Oh EM, Lee KE, Yoon K, Kim SY, Kim HC, Youn YK. Value of adrenal venous sampling for lesion localization in primary aldosteronism. World J Surg. 2012; 36:2522–2527. PMID: 22736344.
Article12. Mathur A, Kemp CD, Dutta U, Baid S, Ayala A, Chang RE, et al. Consequences of adrenal venous sampling in primary hyperaldosteronism and predictors of unilateral adrenal disease. J Am Coll Surg. 2010; 211:384–390. PMID: 20800196.
Article13. Kempers MJ, Lenders JW, van Outheusden L, van der Wilt GJ, Schultze Kool LJ, Hermus AR, et al. Systematic review: diagnostic procedures to differentiate unilateral from bilateral adrenal abnormality in primary aldosteronism. Ann Intern Med. 2009; 151:329–337. PMID: 19721021.
Article14. Minami I, Yoshimoto T, Hirono Y, Izumiyama H, Doi M, Hirata Y. Diagnostic accuracy of adrenal venous sampling in comparison with other parameters in primary aldosteronism. Endocr J. 2008; 55:839–846. PMID: 18497447.
Article15. Graham UM, Ellis PK, Hunter SJ, Leslie H, Mullan KR, Atkinson AB. 100 Cases of primary aldosteronism: careful choice of patients for surgery using adrenal venous sampling and CT imaging results in excellent blood pressure and potassium outcomes. Clin Endocrinol (Oxf). 2012; 76:26–32. PMID: 21767289.
Article16. Murashima M, Trerotola SO, Fraker DL, Han D, Townsend RR, Cohen DL. Adrenal venous sampling for primary aldosteronism and clinical outcomes after unilateral adrenalectomy: a single-center experience. J Clin Hypertens (Greenwich). 2009; 11:316–323. PMID: 19527322.
Article17. Vonend O, Ockenfels N, Gao X, Allolio B, Lang K, Mai K, et al. Adrenal venous sampling: evaluation of the German Conn's registry. Hypertension. 2011; 57:990–995. PMID: 21383311.18. Rossi GP, Barisa M, Allolio B, Auchus RJ, Amar L, Cohen D, et al. The Adrenal Vein Sampling International Study (AVIS) for identifying the major subtypes of primary aldosteronism. J Clin Endocrinol Metab. 2012; 97:1606–1614. PMID: 22399502.
Article19. Zarnegar R, Young WF Jr, Lee J, Sweet MP, Kebebew E, Farley DR, et al. The aldosteronoma resolution score: predicting complete resolution of hypertension after adrenalectomy for aldosteronoma. Ann Surg. 2008; 247:511–518. PMID: 18376197.20. Utsumi T, Kawamura K, Imamoto T, Kamiya N, Komiya A, Suzuki S, et al. High predictive accuracy of aldosteronoma resolution score in Japanese patients with aldosterone-producing adenoma. Surgery. 2012; 151:437–443. PMID: 22000827.
Article21. Carter Y, Roy M, Sippel RS, Chen H. Persistent hypertension after adrenalectomy for an aldosterone-producing adenoma: weight as a critical prognostic factor for aldosterone's lasting effect on the cardiac and vascular systems. J Surg Res. 2012; 177:241–247. PMID: 22921664.
Article22. Sawka AM, Young WF, Thompson GB, Grant CS, Farley DR, Leibson C, et al. Primary aldosteronism: factors associated with normalization of blood pressure after surgery. Ann Intern Med. 2001; 135:258–261. PMID: 11511140.
Article23. Steichen O, Zinzindohoue F, Plouin PF, Amar L. Outcomes of adrenalectomy in patients with unilateral primary aldosteronism: a review. Horm Metab Res. 2012; 44:221–227. PMID: 22395801.
Article24. Obara T, Ito Y, Okamoto T, Kanaji Y, Yamashita T, Aiba M, et al. Risk factors associated with postoperative persistent hypertension in patients with primary aldosteronism. Surgery. 1992; 112:987–993. PMID: 1455323.25. Pang TC, Bambach C, Monaghan JC, Sidhu SB, Bune A, Delbridge LW, et al. Outcomes of laparoscopic adrenalectomy for hyperaldosteronism. ANZ J Surg. 2007; 77:768–773. PMID: 17685956.26. Kupers EM, Amar L, Raynaud A, Plouin PF, Steichen O. A clinical prediction score to diagnose unilateral primary aldosteronism. J Clin Endocrinol Metab. 2012; 97:3530–3537. PMID: 22918872.27. Zhang X, Zhu Z, Xu T, Shen Z. Factors affecting complete hypertension cure after adrenalectomy for aldosterone-producing adenoma: outcomes in a large series. Urol Int. 2013; 90:430–434. PMID: 23466491.
Article28. Giacchetti G, Ronconi V, Rilli S, Guerrieri M, Turchi F, Boscaro M. Small tumor size as favorable prognostic factor after adrenalectomy in Conn's adenoma. Eur J Endocrinol. 2009; 160:639–646. PMID: 19131503.
Article29. Tresallet C, Salepcioglu H, Godiris-Petit G, Hoang C, Girerd X, Menegaux F. Clinical outcome after laparoscopic adrenalectomy for primary hyperaldosteronism: the role of pathology. Surgery. 2010; 148:129–134. PMID: 20083287.
Article30. Davidson JK, Morley P, Hurley GD, Holford NG. Adrenal venography and ultrasound in the investigation of the adrenal gland: an analysis of 58 cases. Br J Radiol. 1975; 48:435–450. PMID: 1227698.
Article31. Espiner EA, Ross DG, Yandle TG, Richards AM, Hunt PJ. Predicting surgically remedial primary aldosteronism: role of adrenal scanning, posture testing, and adrenal vein sampling. J Clin Endocrinol Metab. 2003; 88:3637–3644. PMID: 12915648.
Article32. Umakoshi H, Tanase-Nakao K, Wada N, Ichijo T, Sone M, Inagaki N, et al. Importance of contralateral aldosterone suppression during adrenal vein sampling in the subtype evaluation of primary aldosteronism. Clin Endocrinol (Oxf). 2015; 83:462–467. PMID: 25727719.
Article33. Strajina V, Al-Hilli Z, Andrews JC, Bancos I, Thompson GB, Farley DR, et al. Primary aldosteronism: making sense of partial data sets from failed adrenal venous samplingsuppression of adrenal aldosterone production can be used in clinical decision making. Surgery. 2018; 163:801–806. PMID: 29174432.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors Influencing the Outcomes of Operations for Adrenal Hypertention
- Anesthetic Experience of Adrenalectomy with Primary Aldosteronism
- Hypertension Controlled by Adrenalectomy: A Case of Primary Aldosteronism
- Predictors of Resolution of Hypertension after Adrenalectomy in Patients with Aldosterone-producing Adenoma
- Anesthetic Experience of Adrenalectomy with Primary Aldosteronism - Report of two cases