J Korean Neurosurg Soc.
2017 Feb;60(2):205-210. 10.3340/jkns.2016.0405.007.
Impact of Position on Efficacy of Caudal Epidural Injection for Low Back Pain and Radicular Leg Pain Due to Central Spinal Stenosis and Lumbar Disc Hernia
- Affiliations
-
- 1Department of Neurosurgery, Kahramanmaras Sutcu Imam University Medical Faculty, Kahramanmaras, Turkey. idrisaltun46@hotmail.com
- KMID: 2374882
- DOI: http://doi.org/10.3340/jkns.2016.0405.007
Abstract
OBJECTIVE
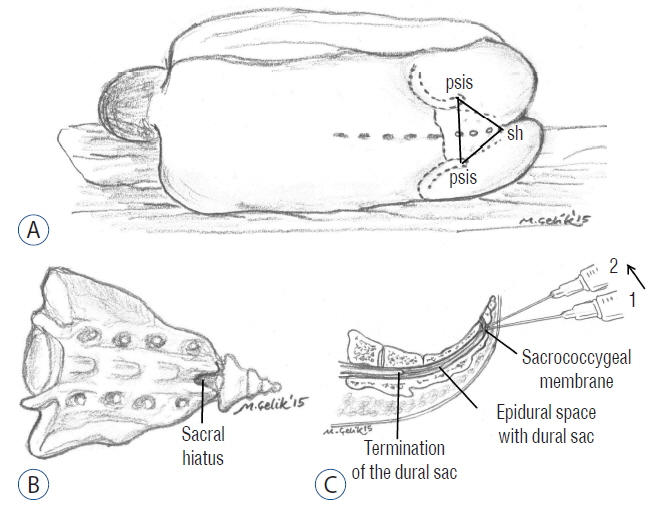
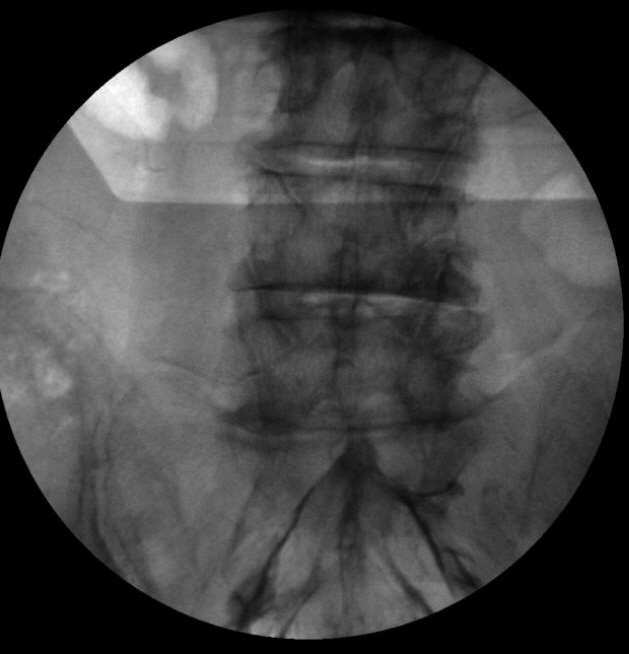
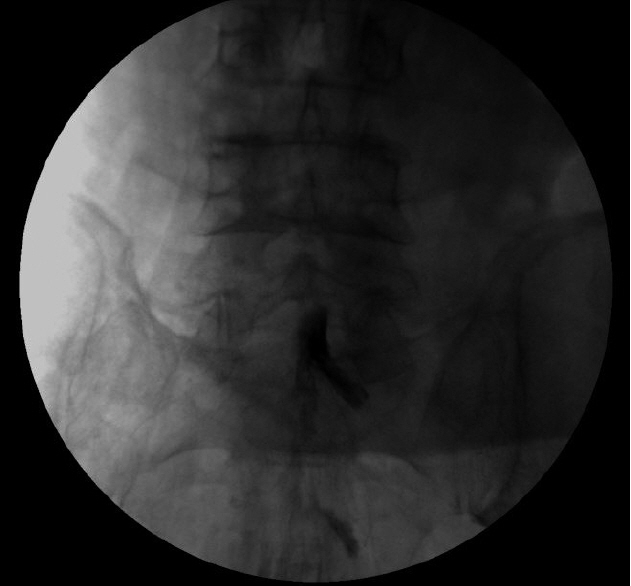
This study was performed to evaluate and compare the efficacies of caudal epidural injections performed at prone and lateral decubitus positions.
METHODS
A total of 120 patients suffering from low back pain and radicular leg pain were included and patients were randomly distributed into 2 groups according to the position during injection. In Group 1 (n=60; 32 women, 28 men), caudal epidural injection was performed at prone position, whereas it was implemented at lateral decubitus position in Group 2 (n=60; 33 women, 27 men). Visual analogue scale, Oswestry Disability Index (ODI), walking tolerance (WT) and standing tolerance (ST) were compared in 2 groups before and after injection.
RESULTS
In Group 1, ODI values were higher at 30th minute (p=0.007), 3rd week (p=0.043) and 6th month (p=0.013). In Group 1, ODI, VAS and ST values were improved significantly at all follow-up periods compared to initial values. In Group 1, WT scores were better than initial values at 30th minute, 3rd week and 3rd month. In Group 2, ODI scores at 30th minute, 3rd week, 3rd month and 6th month were improved while VAS and ST scores were improved at all periods after injection. WT scores were better at 30th minute, 3rd week and 3rd month compared to initial WT scores.
CONCLUSION
Our results indicated that application of injection procedure at lateral decubitus position allowing a more concentrated local distribution may provide better relief of pain.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Abdi S, Datta S, Trescot AM, Schultz DM, Adlaka R, Atluri SL, et al. Epidural steroids in the management of chronic spinal pain: a systematic review. Pain Physician. 10:185–212. 2007.2. Alderman N, Shepherd J, Youngson H. Increasing standing tolerance and posture quality following severe brain injury using a behavior modification approach. Physiotherapy. 78:335–343. 1992.
Article3. Botwin K, Brown LA, Fishman M, Rao S. Fluoroscopically guided caudal epidural steroid injections in degenerative lumbar spine stenosis. Pain Physician. 10:547–558. 2007.4. Dincer U, Kiralp MZ, Cakar E, Yasar E, Dursan H. Caudal epidural injection versus non-steroidal anti-inflammatory drugs in the treatment of low back pain accompanied with radicular pain. Joint Bone Spine. 74:467–471. 2007.
Article5. Enk D. Unilateral spinal anaesthesia: gadget or tool? Curr Opin Anaesthesiol. 11:511–515. 1998.
Article6. Fairbank JC, Pynsent PB. The Oswestry disability index. Spine (Phila Pa 1976). 25:2940–2952. discussion 2952. 2000.
Article7. Korhonen AM, Valanne JV, Jokela RM, Ravaska P, Volmanen P, Korttila K. Influence of the injection site (L2/3 or L3/4) and the posture of the vertebral column on selective spinal anesthesia for ambulatory knee arthroscopy. Acta Anaesthesiol Scand. 49:72–77. 2005.
Article8. Makki D, Nawabi DH, Francis R, Hamed AR, Hussein AA. Is the outcome of caudal epidural injections affected by patient positioning? Spine (Phila Pa 1976). 35:E687–E690. 2010.
Article9. Manchikanti L, Singh V, Cash KA, Pampati V, Damron KS, Boswell MV. Preliminary results of a randomized, equivalence trial of fluoroscopic caudal epidural injections in managing chronic low back pain: Part 2--Disc herniation and radiculitis. Pain Physician. 11:801–815. 2008.10. Mannion AF, Balagué F, Pellisé F, Cedraschi C. Pain measurement in patients with low back pain. Nat Clin Pract Rheumatol. 3:610–618. 2007.
Article11. Martin-Salvaj G, Van Gessel E, Forster A, Schweizer A, Iselin-Chaves I, Gamulin Z. Influence of duration of lateral decubitus on the spread of hyperbaric tetracaine during spinal anesthesia: a prospective time-response study. Anesth Analg. 79:1107–1112. 1994.12. Miyakoshi N, Shimada Y, Kasukawa Y, Saito H, Kodama H, Itoi E. Total dorsal ramus block for the treatment of chronic low back pain: a preliminary study. Joint Bone Spine. 74:270–274. 2007.
Article13. Ritti-Dias RM, Wolosker N, de Moraes Forjaz CL, Carvalho CR, Cucato GG, Leão PP, et al. Strength training increases walking tolerance in intermittent claudication patients: randomized trial. J Vasc Surg. 51:89–95. 2010.
Article14. Schizas C, Theumann N, Burn A, Tansey R, Wardlaw D, Smith FW, et al. Qualitative grading of severity of lumbar spinal stenosis based on the morphology of the dural sac on magnetic resonance images. Spine (Phila Pa 1976). 35:1919–1924. 2010.
Article15. Sumi M, Sakura S, Koshizaki M, Saito Y, Kosaka Y. The advantages of the lateral decubitus position after spinal anesthesia with hyperbaric tetracaine. Anesth Analg. 87:879–884. 1998.
Article16. Vaghadia H. Spinal anaesthesia for outpatients: controversies and new techniques. Can J Anaesth. 45(5 Pt 2):R64–R75. 1998.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anterior Epidural Irrigation in a Lumbar Spinal Stenosis Patient
- Arachnoiditis Following Caudal Epidural Injections for the Lumbo-Sacral Radicular Pain
- The Effects of Selective Spinal Nerve Root Steroid Injedtion for Low Back Pain and Radicular Pain in Patients with Interbetebral Disc Herniation or Spinal stenosis
- Persistent Hiccup after Epidural Steroid Injection: Case reports
- Caudal Epidural Injectioin in Treatment of Lumbosacral Radicular Leg Pain