Yonsei Med J.
2016 Sep;57(5):1271-1275. 10.3349/ymj.2016.57.5.1271.
Prevalence and Antibiotic Susceptibility of Mycoplasma hominis and Ureaplasma urealyticum in Pregnant Women
- Affiliations
-
- 1Department of Laboratory Medicine, Kyung Hee University School of Medicine, Kyung Hee University Hospital at Gangdong, Seoul, Korea. meikim96@hanmail.net
- KMID: 2374175
- DOI: http://doi.org/10.3349/ymj.2016.57.5.1271
Abstract
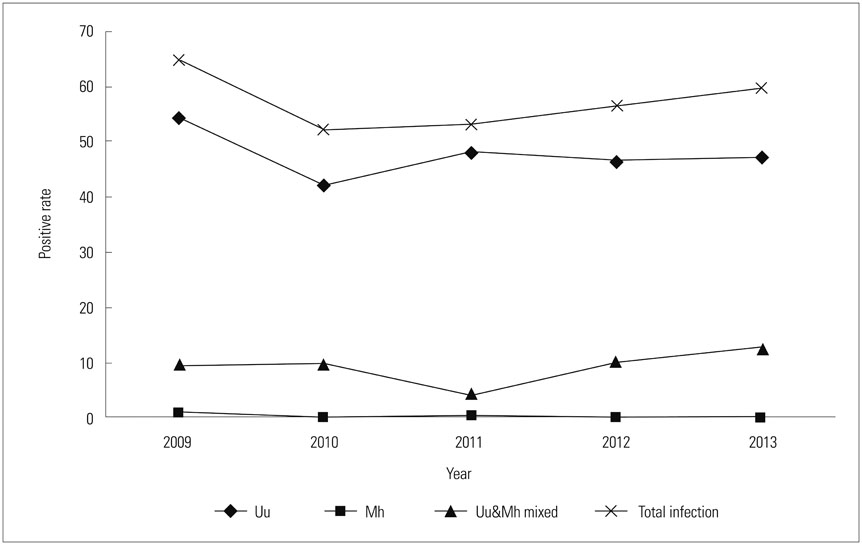
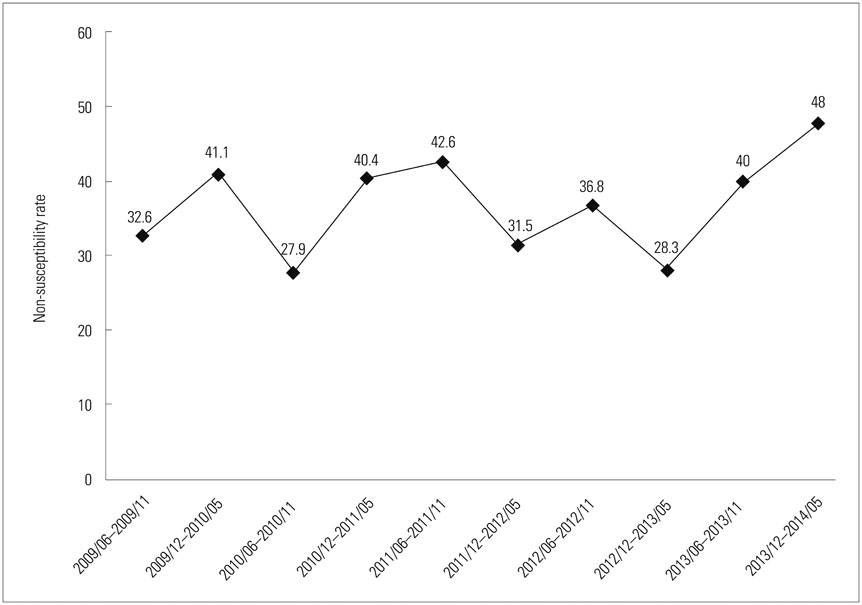
- Mycoplasma hominis (M. hominis) and Ureaplasma urealyticum (U. urealyticum) are important opportunistic pathogens that cause urogenital infections and complicate pregnancy. The aim of this study was to investigate the prevalence, effects on pregnancy outcomes, and antimicrobial susceptibilities of M. hominis and U. urealyticum. We tested vaginal swabs obtained from 1035 pregnant women for the presence of genital mycoplasmas between June 2009 and May 2014. The laboratory and clinical aspects of genital mycoplasmas infection were reviewed retrospectively, and the identification and antimicrobial susceptibility of genital mycoplasmas were determined using the Mycoplasma IST-2 kit. A total of 571 instances of M. hominis and/or U. urealyticum were detected. Of them, M. hominis was detected in two specimens, whereas U. urealyticum was detected in 472 specimens. The remaining 97 specimens were positive for both M. hominis and U. urealyticum. Preterm deliveries were frequently observed in cases of mixed infection of M. hominis and U. urealyticum, and instances of preterm premature rupture of membrane were often found in cases of U. urealyticum. The rates of non-susceptible isolates to erythromycin, empirical agents for pregnant women, showed increasing trends. In conclusion, the prevalence of M. hominis and/or U. urealyticum infections in pregnant women is high, and the resistance rate of antimicrobial agents tends to increase. Therefore, to maintain a safe pregnancy, it is important to identify the isolates and use appropriate empirical antibiotics immediately.
Keyword
MeSH Terms
-
Adolescent
Adult
Anti-Bacterial Agents/*pharmacology/therapeutic use
Female
Humans
Infant, Newborn
Microbial Sensitivity Tests
Middle Aged
Mycoplasma Infections/drug therapy/*epidemiology
Mycoplasma hominis/*drug effects/physiology
Pregnancy
Pregnancy Complications, Infectious/drug therapy/*epidemiology
Pregnancy Outcome
Prevalence
Retrospective Studies
Ureaplasma Infections/drug therapy/*epidemiology
Ureaplasma urealyticum/*drug effects/physiology
Young Adult
Anti-Bacterial Agents
Figure
Cited by 1 articles
-
Letter to the Editor: Breakpoints of the Mycoplasma Hominis and Ureaplasma Urealyticum
Hyun Soo Park
Yonsei Med J. 2017;58(6):1252-1252. doi: 10.3349/ymj.2017.58.6.1252.
Reference
-
1. Redelinghuys MJ, Ehlers MM, Dreyer AW, Lombaard HA, Kock MM. Antimicrobial susceptibility patterns of Ureaplasma species and Mycoplasma hominis in pregnant women. BMC Infect Dis. 2014; 14:171.
Article2. Stellrecht KA, Woron AM, Mishrik NG, Venezia RA. Comparison of multiplex PCR assay with culture for detection of genital mycoplasmas. J Clin Microbiol. 2004; 42:1528–1533.
Article3. Kataoka S, Yamada T, Chou K, Nishida R, Morikawa M, Minami M, et al. Association between preterm birth and vaginal colonization by mycoplasmas in early pregnancy. J Clin Microbiol. 2006; 44:51–55.
Article4. Arai S, Gohara Y, Kuwano K, Kawashima T. Antimycoplasmal activities of new quinolones, tetracyclines, and macrolides against Mycoplasma pneumoniae. Antimicrob Agents Chemother. 1992; 36:1322–1324.
Article5. Hannan PC. Comparative susceptibilities of various AIDS-associated and human urogenital tract mycoplasmas and strains of Mycoplasma pneumoniae to 10 classes of antimicrobial agent in vitro. J Med Microbiol. 1998; 47:1115–1122.
Article6. Kenny GE, Cartwright FD. Susceptibilities of Mycoplasma hominis and Ureaplasma urealyticum to two new quinolones, sparfloxacin and WIN 57273. Antimicrob Agents Chemother. 1991; 35:1515–1516.
Article7. Kenny GE, Cartwright FD. Susceptibilities of Mycoplasma hominis, M. pneumoniae, and Ureaplasma urealyticum to GAR-936, dalfopristin, dirithromycin, evernimicin, gatifloxacin, linezolid, moxifloxacin, quinupristin-dalfopristin, and telithromycin compared to their susceptibilities to reference macrolides, tetracyclines, and quinolones. Antimicrob Agents Chemother. 2001; 45:2604–2608.
Article8. Song T, Ye A, Xie X, Huang J, Ruan Z, Kong Y, et al. Epidemiological investigation and antimicrobial susceptibility analysis of ureaplasma species and Mycoplasma hominis in outpatients with genital manifestations. J Clin Pathol. 2014; 67:817–820.
Article9. Koh E, Kim S, Kim IS, Maeng KY, Lee S. Antimicrobial susceptibilities of Ureaplasma urealyticum and Mycoplasma hominis in pregnant women. Korean J Clin Microbiol. 2009; 12:159–162.
Article10. Wang QY, Li RH, Zheng LQ, Shang XH. Prevalence and antimicrobial susceptibility of Ureaplasma urealyticum and Mycoplasma hominis in female outpatients, 2009-2013. J Microbiol Immunol Infect. 2014; 07. 28. [Epub ahead of print]. DOI: 10.1016/j.jmii.2014.06.007.
Article11. Capoccia R, Greub G, Baud D. Ureaplasma urealyticum, Mycoplasma hominis and adverse pregnancy outcomes. Curr Opin Infect Dis. 2013; 26:231–240.
Article12. Larsen B, Hwang J. Mycoplasma, Ureaplasma, and adverse pregnancy outcomes: a fresh look. Infect Dis Obstet Gynecol. 2010; 2010:DOI: 10.1155/2010/521921.13. Breugelmans M, Vancutsem E, Naessens A, Laubach M, Foulon W. Association of abnormal vaginal flora and Ureaplasma species as risk factors for preterm birth: a cohort study. Acta Obstet Gynecol Scand. 2010; 89:256–260.
Article14. Choi SJ, Park SD, Jang IH, Uh Y, Lee A. The prevalence of vaginal microorganisms in pregnant women with preterm labor and preterm birth. Ann Lab Med. 2012; 32:194–200.
Article15. Taylor-Robinson D. The role of mycoplasmas in pregnancy outcome. Best Pract Res Clin Obstet Gynaecol. 2007; 21:425–438.
Article16. Raynes Greenow CH, Roberts CL, Bell JC, Peat B, Gilbert GL, Parker S. Antibiotics for ureaplasma in the vagina in pregnancy. Cochrane Database Syst Rev. 2011; (9):CD003767.17. Bébéar C, Kempf I. Antimicrobial therapy and antimicrobial resistance. In : Blanchard A, Browning GF, editors. Mycoplasmas: Pathogenesis, Molecular Biology, and Emerging Strategies for Control. Wymondham: Horizon Bioscience;2005. p. 535–568.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antimicrobial Susceptibilities of Ureaplasma urealyticum and Mycoplasma hominis in Pregnant Women
- The detection rate of Ureaplasma urealyticum and Mycoplasma hominis in patients with impending preterm birth and mid-trimester cervical swab
- Detection and Isolation of Genital Mycoplasmas from Public Toilet Bowls
- Positive culture rate and antimicrobial susceptibilities of Mycoplasma hominis and Ureaplasma urealyticum
- The Prevalence of Vaginal Microorganisms in Pregnant Women with Preterm Labor and Preterm Birth