Yonsei Med J.
2016 Jul;57(4):893-899. 10.3349/ymj.2016.57.4.893.
Cyclooxygenase-2 Inhibitor Reduces Hepatic Stiffness in Pediatric Chronic Liver Disease Patients Following Kasai Portoenterostomy
- Affiliations
-
- 1Department of Pediatric Surgery, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 2Department of Pediatric Surgery, Severance Children's Hospital, Department of Surgery, Yonsei University College of Medicine, Seoul, Korea. sjhan@yuhs.ac
- KMID: 2374120
- DOI: http://doi.org/10.3349/ymj.2016.57.4.893
Abstract
- PURPOSE
The purpose of this study was to define the role of cyclooxygenase-2 inhibitors (COX-2i) in reducing hepatic fibrosis in pediatric patients with chronic liver disease.
MATERIALS AND METHODS
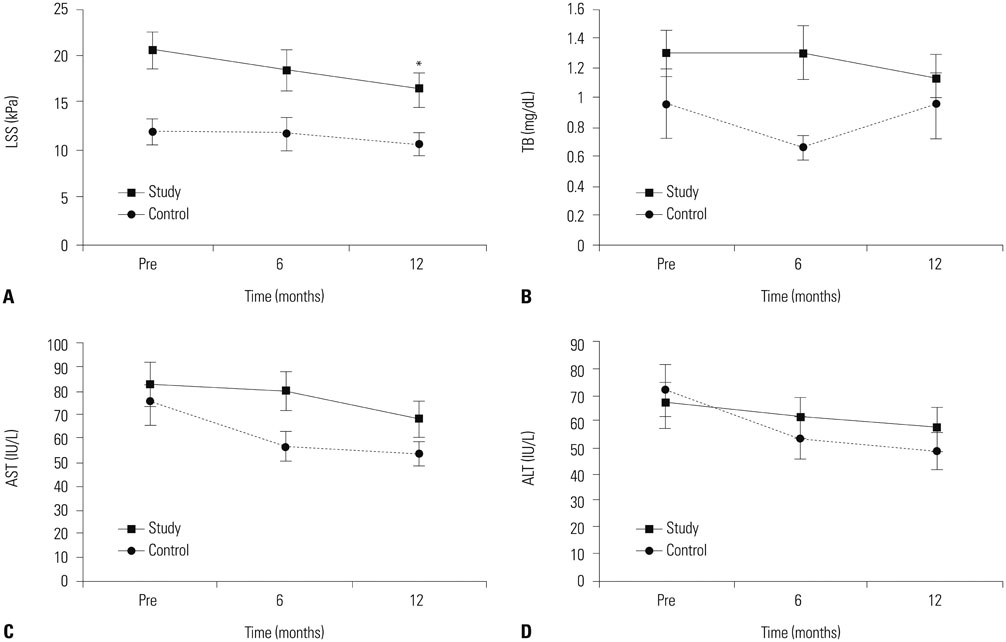
From September 2009 to September 2010, patients over 2 years old who visited our outpatient clinic for follow-up to manage their chronic liver disease after Kasai portoenterostomy for biliary atresia, were included in this study. Volunteers were assigned to the study or control groups, according to their preference. A COX-2i was given to only the study group after obtaining consent. The degree of hepatic fibrosis (liver stiffness score, LSS) was prospectively measured using FibroScan, and liver function was examined using serum analysis before and after treatment. After 1 year, changes in LSSs and liver function were compared between the two groups.
RESULTS
Twenty-five patients (18 females and 7 males) were enrolled in the study group. The control group included 44 patients (26 females and 18 males). After 1 year, the least square mean values for the LSSs were significantly decreased by 3.91±0.98 kPa (p=0.004) only in the study group. Serum total bilirubin did not decrease significantly in either group.
CONCLUSION
COX-2i treatment improved the LSS in patients with chronic liver disease after Kasai portoenterostomy for biliary atresia.
Keyword
MeSH Terms
-
Biliary Atresia/complications/enzymology/*surgery
Child
Child, Preschool
Chronic Disease
Cyclooxygenase 2 Inhibitors/*therapeutic use
Female
Humans
Liver Cirrhosis/etiology/pathology/*prevention & control
Male
*Portoenterostomy, Hepatic
Thiazines/*therapeutic use
Thiazoles/*therapeutic use
Cyclooxygenase 2 Inhibitors
Thiazines
Thiazoles
Figure
Reference
-
1. Hadzić N, Davenport M, Tizzard S, Singer J, Howard ER, Mieli-Vergani G. Long-term survival following Kasai portoenterostomy: is chronic liver disease inevitable? J Pediatr Gastroenterol Nutr. 2003; 37:430–433.
Article2. Hartley JL, Davenport M, Kelly DA. Biliary atresia. Lancet. 2009; 374:1704–1713.
Article3. Davenport M. Biliary atresia: clinical aspects. Semin Pediatr Surg. 2012; 21:175–184.
Article4. Hadžić N, Quaglia A, Portmann B, Paramalingam S, Heaton ND, Rela M, et al. Hepatocellular carcinoma in biliary atresia: King's College Hospital experience. J Pediatr. 2011; 159:617–622.e1.
Article5. Hol L, van den Bos IC, Hussain SM, Zondervan PE, de Man RA. Hepatocellular carcinoma complicating biliary atresia after Kasai portoenterostomy. Eur J Gastroenterol Hepatol. 2008; 20:227–231.
Article6. Honsawek S, Klaikeaw N, Vejchapipat P, Chongsrisawat V, Ruangvejvorachai P, Poovorawan Y. Cyclooxygenase-2 overexpression is associated with clinical outcome in biliary atresia. Eur J Pediatr Surg. 2010; 20:164–168.
Article7. Mohammed NA, Abd El-Aleem SA, El-Hafiz HA, McMahon RF. Distribution of constitutive (COX-1) and inducible (COX-2) cyclooxygenase in postviral human liver cirrhosis: a possible role for COX-2 in the pathogenesis of liver cirrhosis. J Clin Pathol. 2004; 57:350–354.
Article8. Morinaga S, Tarao K, Yamamoto Y, Nakamura Y, Rino Y, Miyakawa K, et al. Overexpressed cyclo-oxygenase-2 in the background liver is associated with the clinical course of hepatitis C virus-related cirrhosis patients after curative surgery for hepatocellular carcinoma. J Gastroenterol Hepatol. 2007; 22:1249–1255.
Article9. Pazirandeh S, Khettry U, Gordon FD, Resnick RH, Murray JE, Sheth SG. Cyclooxygenase-2 expression in hepatocellular carcinoma, cirrhosis and chronic hepatitis in the United States. Dig Dis Sci. 2007; 52:220–227.
Article10. Yamamoto H, Kondo M, Nakamori S, Nagano H, Wakasa K, Sugita Y, et al. JTE-522, a cyclooxygenase-2 inhibitor, is an effective chemopreventive agent against rat experimental liver fibrosis. Gastroenterology. 2003; 125:556–571.
Article11. Tu CT, Guo JS, Wang M, Wang JY. Antifibrotic activity of rofecoxib in vivo is associated with reduced portal hypertension in rats with carbon tetrachloride-induced liver injury. J Gastroenterol Hepatol. 2007; 22:877–884.
Article12. Chávez E, Segovia J, Shibayama M, Tsutsumi V, Vergara P, Castro-Sánchez L, et al. Antifibrotic and fibrolytic properties of celecoxib in liver damage induced by carbon tetrachloride in the rat. Liver Int. 2010; 30:969–978.
Article13. Horrillo R, Planagumà A, González-Périz A, Ferré N, Titos E, Miquel R, et al. Comparative protection against liver inflammation and fibrosis by a selective cyclooxygenase-2 inhibitor and a nonredox-type 5-lipoxygenase inhibitor. J Pharmacol Exp Ther. 2007; 323:778–786.
Article14. Kim SM, Park KC, Kim HG, Han SJ. Effect of selective cyclooxygenase-2 inhibitor meloxicam on liver fibrosis in rats with ligated common bile ducts. Hepatol Res. 2008; 38:800–809.
Article15. Tolba RH, Fet N, Yonezawa K, Taura K, Nakajima A, Hata K, et al. Role of preferential cyclooxygenase-2 inhibition by meloxicam in ischemia/reperfusion injury of the rat liver. Eur Surg Res. 2014; 53:11–24.
Article16. Edfawy M, Hassan MH, Mansour A, Hamed AA, Amin HA. Meloxicam modulates oxidative stress status, inhibits prostaglandin E2, and abrogates apoptosis in carbon tetrachloride-induced rat hepatic injury. Int J Toxicol. 2012; 31:276–286.
Article17. Gao JH, Wen SL, Yang WJ, Lu YY, Tong H, Huang ZY, et al. Celecoxib ameliorates portal hypertension of the cirrhotic rats through the dual inhibitory effects on the intrahepatic fibrosis and angiogenesis. PLoS One. 2013; 8:e69309.
Article18. Chang HK, Park YJ, Koh H, Kim SM, Chung KS, Oh JT, et al. Hepatic fibrosis scan for liver stiffness score measurement: a useful preendoscopic screening test for the detection of varices in postoperative patients with biliary atresia. J Pediatr Gastroenterol Nutr. 2009; 49:323–328.
Article19. Shinkai M, Ohhama Y, Take H, Kitagawa N, Kudo H, Mochizuki K, et al. Long-term outcome of children with biliary atresia who were not transplanted after the Kasai operation: >20-year experience at a children's hospital. J Pediatr Gastroenterol Nutr. 2009; 48:443–450.
Article20. Chardot C, Buet C, Serinet MO, Golmard JL, Lachaux A, Roquelaure B, et al. Improving outcomes of biliary atresia: French national series 1986-2009. J Hepatol. 2013; 58:1209–1217.
Article21. Kumagi T, Drenth JP, Guttman O, Ng V, Lilly L, Therapondos G, et al. Biliary atresia and survival into adulthood without transplantation: a collaborative multicentre clinic review. Liver Int. 2012; 32:510–518.
Article22. Ng VL, Haber BH, Magee JC, Miethke A, Murray KF, Michail S, et al. Medical status of 219 children with biliary atresia surviving long-term with their native livers: results from a North American multicenter consortium. J Pediatr. 2014; 165:539–546.e2.23. Jeong SW, Jang JY, Lee SH, Kim SG, Cheon YK, Kim YS, et al. Increased expression of cyclooxygenase-2 is associated with the progression to cirrhosis. Korean J Intern Med. 2010; 25:364–371.
Article24. He YF, Jin J, Wei W, Chang Y, Hu B, Ji CS, et al. Overexpression of cyclooxygenase-2 in noncancerous liver tissue increases the postoperative recurrence of hepatocellular carcinoma in patients with hepatitis B virus-related cirrhosis. Can J Gastroenterol. 2010; 24:435–440.
Article25. Wang BH, Bertucci MC, Ma JY, Adrahtas A, Cheung RY, Krum H. Celecoxib, but not rofecoxib or naproxen, attenuates cardiac hypertrophy and fibrosis induced in vitro by angiotensin and aldosterone. Clin Exp Pharmacol Physiol. 2010; 37:912–918.
Article26. Arafa HM, Abdel-Wahab MH, El-Shafeey MF, Badary OA, Hamada FM. Anti-fibrotic effect of meloxicam in a murine lung fibrosis model. Eur J Pharmacol. 2007; 564:181–189.
Article27. Harding P. Do COX-2 inhibitors reduce renal fibrosis? J Hypertens. 2004; 22:43–45.
Article28. Kucuk HF, Bingul SM, Kurt N, Kaptanoglu L, Akyol H, Torlak OA, et al. Effect of a selective cyclooxygenase-2 inhibitor on renal scarring. Eur Surg Res. 2006; 38:451–457.
Article29. Fabbrini P, Schilte MN, Zareie M, ter Wee PM, Keuning ED, Beelen RH, et al. Celecoxib treatment reduces peritoneal fibrosis and angiogenesis and prevents ultrafiltration failure in experimental peritoneal dialysis. Nephrol Dial Transplant. 2009; 24:3669–3676.
Article30. Drugs.com. Meloxicam. accessed on 2008 November 16. Available at: http://www.drugs.com/meloxicam.html.31. Millonig G, Reimann FM, Friedrich S, Fonouni H, Mehrabi A, Büchler MW, et al. Extrahepatic cholestasis increases liver stiffness (FibroScan) irrespective of fibrosis. Hepatology. 2008; 48:1718–1723.
Article32. Fraquelli M, Rigamonti C, Casazza G, Conte D, Donato MF, Ronchi G, et al. Reproducibility of transient elastography in the evaluation of liver fibrosis in patients with chronic liver disease. Gut. 2007; 56:968–973.
Article33. Coco B, Oliveri F, Maina AM, Ciccorossi P, Sacco R, Colombatto P, et al. Transient elastography: a new surrogate marker of liver fibrosis influenced by major changes of transaminases. J Viral Hepat. 2007; 14:360–369.
Article34. Sagir A, Erhardt A, Schmitt M, Häussinger D. Transient elastography is unreliable for detection of cirrhosis in patients with acute liver damage. Hepatology. 2008; 47:592–595.
Article35. Arena U, Vizzutti F, Corti G, Ambu S, Stasi C, Bresci S, et al. Acute viral hepatitis increases liver stiffness values measured by transient elastography. Hepatology. 2008; 47:380–384.
Article36. Yoshioka K, Kawabe N, Hashimoto S. Transient elastography: applications and limitations. Hepatol Res. 2008; 38:1063–1068.
Article