Yonsei Med J.
2016 Jul;57(4):840-845. 10.3349/ymj.2016.57.4.840.
Prognostic Evaluation of Nasopharyngeal Carcinoma with Bone-Only Metastasis after Therapy
- Affiliations
-
- 1Provincial Clinical College, Fujian Medical University, Fuzhou, Fujian, China. panjianji@126.com
- 2Department of Radiation Oncology, Fujian Provincial Cancer Hospital, Fuzhou, Fujian, China.
- 3Fujian Provincial Key Laboratory of Translational Cancer Medicine, Fuzhou, Fujian, China.
- KMID: 2374113
- DOI: http://doi.org/10.3349/ymj.2016.57.4.840
Abstract
- PURPOSE
To evaluate the prognosis of nasopharyngeal carcinoma (NPC) patients who developed bone-only metastasis after primary treatment and the stratification of these patients into different risk groups based on independent prognostic factors.
MATERIALS AND METHODS
Eighty NPC patients who developed bone-only metastasis after definitive radiotherapy from October 2005 to December 2010 were enrolled. All these patients received palliative treatment for bone metastasis, including chemotherapy and/or radiotherapy. Clinical features, treatment modality, and laboratory parameters were examined with univariate and multivariate analyses.
RESULTS
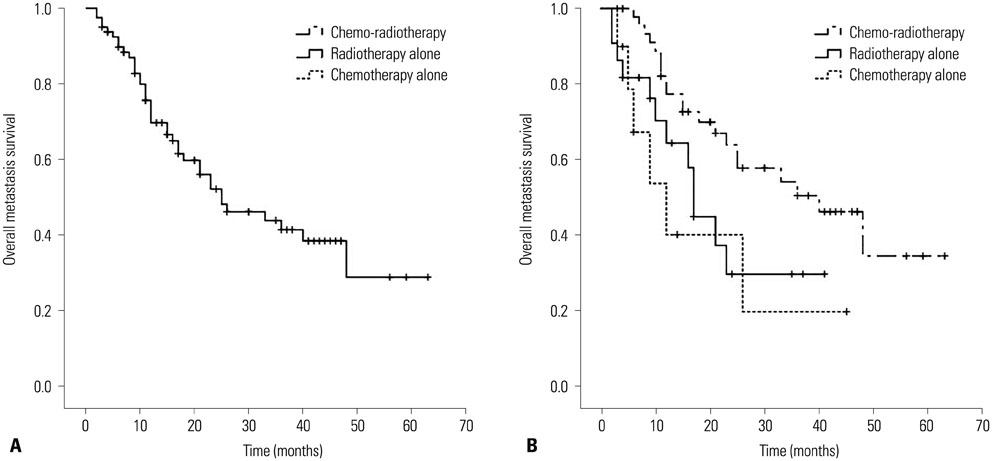
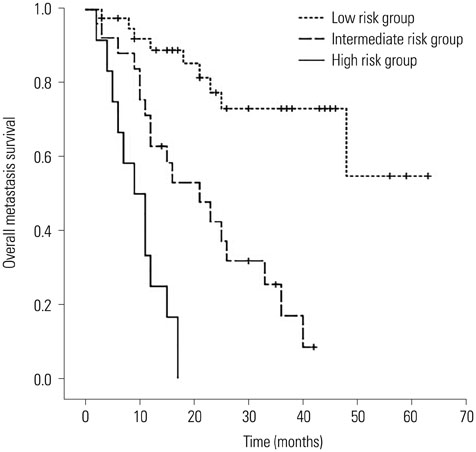
The median follow-up time was 15.5 months (range, 2-67 months) for the whole cohort. The median overall metastatic survival (OMS) time and the 2-year estimate OMS rate were 26.5 months and 52%, respectively. Multivariate analysis indicated that patients with short metastases-free interval, multiple bone metastases sites, high serum lactic dehydrogenase levels, and treated with radiotherapy or chemotherapy alone had significantly worse outcomes. Patients were stratified into three different risk groups based on the number of adverse factors present. The OMS curves of the three groups were all significantly different (p<0.001).
CONCLUSION
Severl prognostic factors were found to be associated with worse outcomes. According to the number of adverse factors present, bone-only metastasis patients can be stratified into three risk groups with significantly different prognoses. Such grouping may help in improving the design of clinical trials and in guiding individualized treatment for NPC patients with bone-only metastasis.
MeSH Terms
Figure
Reference
-
1. Wei WI, Sham JS. Nasopharyngeal carcinoma. Lancet. 2005; 365:2041–2054.
Article2. Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011; 61:69–90.
Article3. Lai SZ, Li WF, Chen L, Luo W, Chen YY, Liu LZ, et al. How does intensity-modulated radiotherapy versus conventional two-dimensional radiotherapy influence the treatment results in nasopharyngeal carcinoma patients? Int J Radiat Oncol Biol Phys. 2011; 80:661–668.
Article4. Peng G, Wang T, Yang KY, Zhang S, Zhang T, Li Q, et al. A prospective, randomized study comparing outcomes and toxicities of intensity-modulated radiotherapy vs. conventional two-dimensional radiotherapy for the treatment of nasopharyngeal carcinoma. Radiother Oncol. 2012; 104:286–293.
Article5. Lin S, Pan J, Han L, Guo Q, Hu C, Zong J, et al. Update report of nasopharyngeal carcinoma treated with reduced-volume intensitymodulated radiation therapy and hypothesis of the optimal margin. Radiother Oncol. 2014; 110:385–389.
Article6. Wang TJ, Riaz N, Cheng S, Lu JJ, Lee NY. Intensity-modulated radiation therapy for nasopharyngeal carcinoma: a review. J Radiat Oncol. 2012; 1:129–146.
Article7. Cao CN, Luo JW, Gao L, Yi JL, Huang XD, Wang K, et al. Update report of T4 classification nasopharyngeal carcinoma after intensitymodulated radiotherapy: an analysis of survival and treatment toxicities. Oral Oncol. 2015; 51:190–194.
Article8. Teo PM, Kwan WH, Lee WY, Leung SF, Johnson PJ. Prognosticators determining survival subsequent to distant metastasis from nasopharyngeal carcinoma. Cancer. 1996; 77:2423–2431.
Article9. Hui EP, Leung SF, Au JS, Zee B, Tung S, Chua D, et al. Lung metastasis alone in nasopharyngeal carcinoma: a relatively favorable prognostic group. A study by the Hong Kong Nasopharyngeal Carcinoma Study Group. Cancer. 2004; 101:300–306.
Article10. Lee N, Xia P, Quivey JM, Sultanem K, Poon I, Akazawa C, et al. Intensity-modulated radiotherapy in the treatment of nasopharyngeal carcinoma: an update of the UCSF experience. Int J Radiat Oncol Biol Phys. 2002; 53:12–22.
Article11. Jin Y, An X, Cai YC, Cao Y, Cai XY, Xia Q, et al. Zoledronic acid combined with chemotherapy bring survival benefits to patients with bone metastases from nasopharyngeal carcinoma. J Cancer Res Clin Oncol. 2011; 137:1545–1551.
Article12. Zhao CL, Qian GQ, Chen XY, Chen C. Retrograde analysis of clinical characteristics of bone metastasis in 1,031 cases of preliminarily diagnosed nasopharyngeal carcinoma. Asian Pac J Cancer Prev. 2014; 15:3785–3788.
Article13. Li AC, Xiao WW, Wang L, Shen GZ, Xu AA, Cao YQ, et al. Risk factors and prediction-score model for distant metastasis in nasopharyngeal carcinoma treated with intensity-modulated radiotherapy. Tumour Biol. 2015; 36:8349–8357.
Article14. Provisional recommendations on IFCC methods for the measurement of catalytic concentrations of enzymes. Part 2. IFCC method for aspartate aminotransferase. J Clin Chem Clin Biochem. 1977; 15:39–51.15. Groopman JE, Itri LM. Chemotherapy-induced anemia in adults: incidence and treatment. J Natl Cancer Inst. 1999; 91:1616–1634.
Article16. Cao X, Han Y, He L, Xiang J, Wen Z. Risk subset of the survival for nasopharyngeal carcinoma patients with bone metastases: who will benefit from combined treatment? Oral Oncol. 2011; 47:747–752.
Article17. Hartsell WF, Scott CB, Bruner DW, Scarantino CW, Ivker RA, Roach M 3rd, et al. Randomized trial of short- versus long-course radiotherapy for palliation of painful bone metastases. J Natl Cancer Inst. 2005; 97:798–804.
Article18. Howell DD, James JL, Hartsell WF, Suntharalingam M, Machtay M, Suh JH, et al. Single-fraction radiotherapy versus multifraction radiotherapy for palliation of painful vertebral bone metastasesequivalent efficacy, less toxicity, more convenient: a subset analysis of Radiation Therapy Oncology Group trial 97-14. Cancer. 2013; 119:888–896.
Article19. Capietto AH, Faccio R. Immune regulation of bone metastasis. Bonekey Rep. 2014; 3:600.
Article20. Zhang K, Kim S, Cremasco V, Hirbe AC, Collins L, Piwnica-Worms D, et al. CD8+ T cells regulate bone tumor burden independent of osteoclast resorption. Cancer Res. 2011; 71:4799–4808.
Article21. Koizumi M, Yoshimoto M, Kasumi F, Ogata E. Comparison between solitary and multiple skeletal metastatic lesions of breast cancer patients. Ann Oncol. 2003; 14:1234–1240.
Article22. Ahn SG, Lee HM, Cho SH, Lee SA, Hwang SH, Jeong J, et al. Prognostic factors for patients with bone-only metastasis in breast cancer. Yonsei Med J. 2013; 54:1168–1177.
Article23. Schwartz MK. Lactic dehydrogenase. An old enzyme reborn as a cancer marker? Am J Clin Pathol. 1991; 96:441–443.24. Turen S, Ozyar E, Altundag K, Gullu I, Atahan IL. Serum lactate dehydrogenase level is a prognostic factor in patients with locoregionally advanced nasopharyngeal carcinoma treated with chemoradiotherapy. Cancer Invest. 2007; 25:315–321.
Article25. Jin Y, Ye X, Shao L, Lin BC, He CX, Zhang BB, et al. Serum lactic dehydrogenase strongly predicts survival in metastatic nasopharyngeal carcinoma treated with palliative chemotherapy. Eur J Cancer. 2013; 49:1619–1626.
Article26. Toh CK, Heng D, Ong YK, Leong SS, Wee J, Tan EH. Validation of a new prognostic index score for disseminated nasopharyngeal carcinoma. Br J Cancer. 2005; 92:1382–1387.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Cutaneous Metastasis of Nasopharyngeal Carcinoma on the Face
- Radiation Therapy of Nasopharyngeal Carcinoma
- Treatment Outcomes and Prognostic Factors of Nasopharyngeal Carcinoma
- A Case of Newly Found Lymphoepithelial Carcinoma in Retropharynx of the Patient Who Had Been in the NED State of Nasopharyngeal Carcinoma: Controversy about the Recurrence of Undiffentiated Nasopharyngeal Carcinoma
- An Analysis of Prognostic Factors Affecting the Outcome of Radiation Therapy for Nasopharyngeal Carcinoma