Yonsei Med J.
2016 May;57(3):741-747. 10.3349/ymj.2016.57.3.741.
Point-Connecting Measurements of the Hallux Valgus Deformity: A New Measurement and Its Clinical Application
- Affiliations
-
- 1Department of Orthopaedic Surgery, Dong-A University Medical Center, College of Medicine, Dong-A University, Busan, Korea.
- 2Department of Orthopaedic Surgery, Uijeongbu St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Uijeongbu, Korea. ilmon@hanmail.net
- 3Department of Orthopaedic & Traumatology, Foot and Ankle, Musculoskeletal Clinic, Fatmawati General Hospital, Jakarta, Indonesia.
- KMID: 2374096
- DOI: http://doi.org/10.3349/ymj.2016.57.3.741
Abstract
- PURPOSE
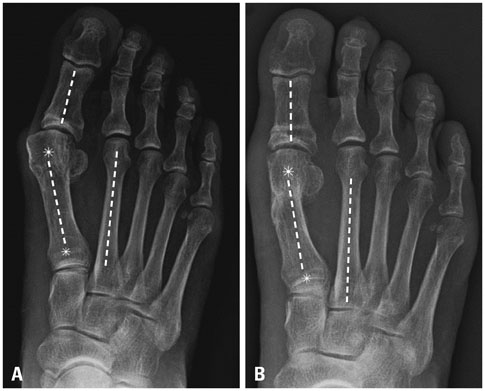
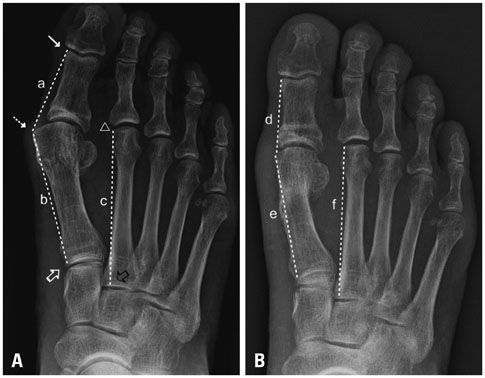
The aim of this study was to investigate new point-connecting measurements for the hallux valgus angle (HVA) and the first intermetatarsal angle (IMA), which can reflect the degree of subluxation of the first metatarsophalangeal joint (MTPJ). Also, this study attempted to compare the validity of midline measurements and the new point-connecting measurements for the determination of HVA and IMA values.
MATERIALS AND METHODS
Sixty feet of hallux valgus patients who underwent surgery between 2007 and 2011 were classified in terms of the severity of HVA, congruency of the first MTPJ, and type of chevron metatarsal osteotomy. On weight-bearing dorsal-plantar radiographs, HVA and IMA values were measured and compared preoperatively and postoperatively using both the conventional and new methods.
RESULTS
Compared with midline measurements, point-connecting measurements showed higher inter- and intra-observer reliability for preoperative HVA/IMA and similar or higher inter- and intra-observer reliability for postoperative HVA/IMA. Patients who underwent distal chevron metatarsal osteotomy (DCMO) had higher intraclass correlation coefficient for inter- and intra-observer reliability for pre- and post-operative HVA and IMA measured by the point-connecting method compared with the midline method. All differences in the preoperative HVAs and IMAs determined by both the midline method and point-connecting methods were significant between the deviated group and subluxated groups (p=0.001).
CONCLUSION
The point-connecting method for measuring HVA and IMA in the subluxated first MTPJ may better reflect the severity of a HV deformity with higher reliability than the midline method, and is more useful in patients with DCMO than in patients with proximal chevron metatarsal osteotomy.
MeSH Terms
Figure
Reference
-
1. Van Vo H, Safiedine AM, Short T, Merrill T. A comparison of 4 common methods of hand-measured techniques with a computerized technique to measure the first intermetatarsal angle. J Foot Ankle Surg. 2004; 43:395–399.
Article2. Elliot RR, Saxby TS. A new method for measuring deformity distal to the hallux metatarsophalangeal joint. Foot Ankle Int. 2010; 31:609–611.
Article3. Deenik AR, de Visser E, Louwerens JW, de Waal Malefijt M, Draijer FF, de Bie RA. Hallux valgus angle as main predictor for correction of hallux valgus. BMC Musculoskelet Disord. 2008; 9:70.
Article4. Coughlin MJ, Jones CP. Hallux valgus: demographics, etiology, and radiographic assessment. Foot Ankle Int. 2007; 28:759–777.
Article5. Schneider W, Csepan R, Kasparek M, Pinggera O, Knahr K. Intra- and interobserver repeatability of radiographic measurements in hallux surgery: improvement and validation of a method. Acta Orthop Scand. 2002; 73:670–673.
Article6. Srivastava S, Chockalingam N, El Fakhri T. Radiographic measurements of hallux angles: a review of current techniques. Foot (Edinb). 2010; 20:27–31.
Article7. Lee KM, Ahn S, Chung CY, Sung KH, Park MS. Reliability and relationship of radiographic measurements in hallux valgus. Clin Orthop Relat Res. 2012; 470:2613–2621.
Article8. Bhutta MA, Chauhan D, Zubairy AI, Barrie J. Second metatarsophalangeal joint instability and second metatarsal length association depends on the method of measurement. Foot Ankle Int. 2010; 31:486–491.
Article9. Shima H, Okuda R, Yasuda T, Jotoku T, Kitano N, Kinoshita M. Radiographic measurements in patients with hallux valgus before and after proximal crescentic osteotomy. J Bone Joint Surg Am. 2009; 91:1369–1376.
Article10. Robinson AH, Cullen NP, Chhaya NC, Sri-Ram K, Lynch A. Variation of the distal metatarsal articular angle with axial rotation and inclination of the first metatarsal. Foot Ankle Int. 2006; 27:1036–1040.
Article11. Piggott H. The natural history of hallux valgus in adolescence and early adult life. J Bone Joint Surg Br. 1960; 42:749–760.
Article12. Miller JW. Distal first metatarsal displacement osteotomy. Its place in the schema of bunion surgery. J Bone Joint Surg Am. 1974; 56:923–931.13. Choi WJ, Yoon HK, Yoon HS, Kim BS, Lee JW. Comparison of the proximal chevron and Ludloff osteotomies for the correction of hallux valgus. Foot Ankle Int. 2009; 30:1154–1160.
Article14. O'Donnell T, Hogan N, Solan M, Stephens MM. Correction of severe hallux valgus using a basal chevron osteotomy and distal soft tissue release. Foot Ankle Surg. 2010; 16:126–131.15. Okuda R, Kinoshita M, Yasuda T, Jotoku T, Shima H, Takamura M. Hallux valgus angle as a predictor of recurrence following proximal metatarsal osteotomy. J Orthop Sci. 2011; 16:760–764.
Article16. Allen DM, Nunley JA 2nd. Measurement of the first/second intermetatarsal angle following proximal oblique metatarsal osteotomy. Foot Ankle Int. 2002; 23:64–67.
Article17. Sammarco VJ. Surgical correction of moderate and severe hallux valgus: proximal metatarsal osteotomy with distal soft-tissue correction and arthrodesis of the metatarsophalangeal joint. Instr Course Lect. 2008; 57:415–428.18. Pinney SJ, Song KR, Chou LB. Surgical treatment of severe hallux valgus: the state of practice among academic foot and ankle surgeons. Foot Ankle Int. 2006; 27:1024–1029.
Article19. Han SH, Park EH, Jo J, Koh YG, Lee JW, Choi WJ, et al. First metatarsal proximal opening wedge osteotomy for correction of hallux valgus deformity: comparison of straight versus oblique osteotomy. Yonsei Med J. 2015; 56:744–752.
Article20. Choi GW, Kim HJ, Kim TW, Lee JW, Park SB, Kim JK. Sex-related differences in outcomes after hallux valgus surgery. Yonsei Med J. 2015; 56:466–473.
Article21. Schneider W, Csepan R, Knahr K. Reproducibility of the radiographic metatarsophalangeal angle in hallux surgery. J Bone Joint Surg Am. 2003; 85-A:494–499.
Article22. Taylor N, Campbell J, Metcalfe S. Radiographic measurement of the first metatarsal: a new technique to improve the accuracy of intermetatarsal angle measurement. J Am Podiatr Med Assoc. 2012; 102:105–113.23. Condon F, Kaliszer M, Conhyea D, O Donnell T, Shaju A, Masterson E. The first intermetatarsal angle in hallux valgus: an analysis of measurement reliability and the error involved. Foot Ankle Int. 2002; 23:717–721.
Article24. Perera AM, Mason L, Stephens MM. The pathogenesis of hallux valgus. J Bone Joint Surg Am. 2011; 93:1650–1661.
Article25. Miller F, Arenson D, Weil LS. Incongruity of the first metatarsophalangeal joint. The effect on cartilage contact surface area. J Am Podiatry Assoc. 1977; 67:328–333.
Article26. Bock P, Kristen KH, Kröner A, Engel A. Hallux valgus and cartilage degeneration in the first metatarsophalangeal joint. J Bone Joint Surg Br. 2004; 86:669–673.
Article27. Thordarson D, Ebramzadeh E, Moorthy M, Lee J, Rudicel S. Correlation of hallux valgus surgical outcome with AOFAS forefoot score and radiological parameters. Foot Ankle Int. 2005; 26:122–127.
Article28. Gines-Cespedosa A, Alentorn-Geli E, Sanchez JF, Leal-Blanquet J, Rigol P, Puig L, et al. Influence of common associated forefoot disorders on preoperative quality of life in patients with hallux valgus. Foot Ankle Int. 2013; 34:1634–1637.
Article29. Menz HB, Roddy E, Thomas E, Croft PR. Impact of hallux valgus severity on general and foot-specific health-related quality of life. Arthritis Care Res (Hoboken). 2011; 63:396–404.
Article30. Lazarides SP, Hildreth A, Prassanna V, Talkhani I. Association amongst angular deformities in hallux valgus and impact of the deformity in health related quality of life. Foot Ankle Surg. 2005; 11:193–196.
Article31. Spink MJ, Menz HB, Lord SR. Distribution and correlates of plantar hyperkeratotic lesions in older people. J Foot Ankle Res. 2009; 2:8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Corrective Osteotomies in Hallux Valgus
- Computerized Measurement on Angular Parameters for Hallux Valgus: Comparison of 100% and 150% Magnified Digital Radiography
- Minimally Invasive Surgery with Tenorrhaphy for Postoperative Hallux Varus Deformity Combined with Flexor Hallucis Longus Rupture after Hallux Valgus Correction: A Case Report
- Minimally Invasive Surgery for Hallux Valgus Deformity Using Intramedullary Low Profile Plate Fixation: A Case Report
- Relationship between Foot Width Reduction and Clinical Outcomes after Chevron Osteotomy for Hallux Valgus Deformity