Yonsei Med J.
2016 May;57(3):606-613. 10.3349/ymj.2016.57.3.606.
Serial Morphological Changes of Side-Branch Ostium after Paclitaxel-Coated Balloon Treatment of De Novo Coronary Lesions of Main Vessels
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Kangwon National University School of Medicine, Chuncheon, Korea.
- 2Department of Cardiology, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea. sesim1989@gmail.com
- 3Division of Cardiology, Department of Medicine and Clinical Science, Yamaguchi University Graduate School of Medicine, Ube, Japan.
- 4East Lancashire Hospitals NHS Trust, Blackburn, Lancashire, UK.
- 5Department of Internal Medicine, Cardiovascular Center, Seoul National University Hospital, Seoul, Korea.
- KMID: 2374078
- DOI: http://doi.org/10.3349/ymj.2016.57.3.606
Abstract
- PURPOSE
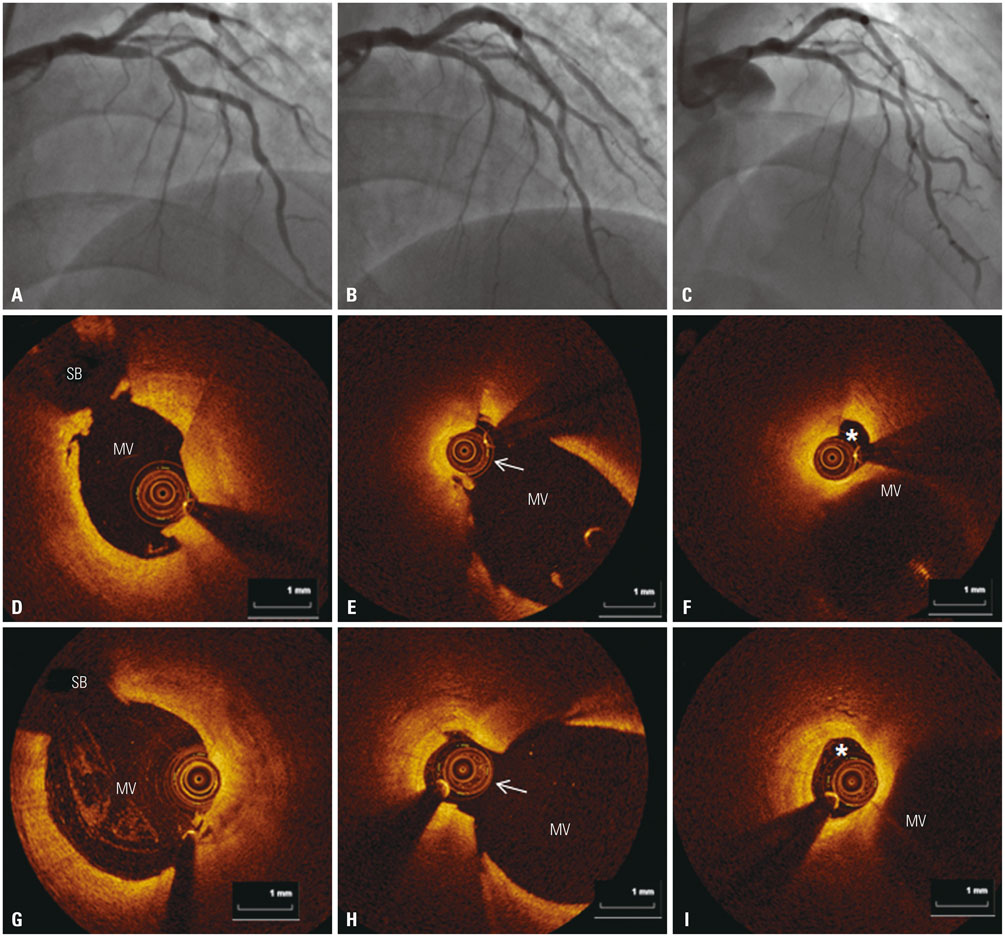
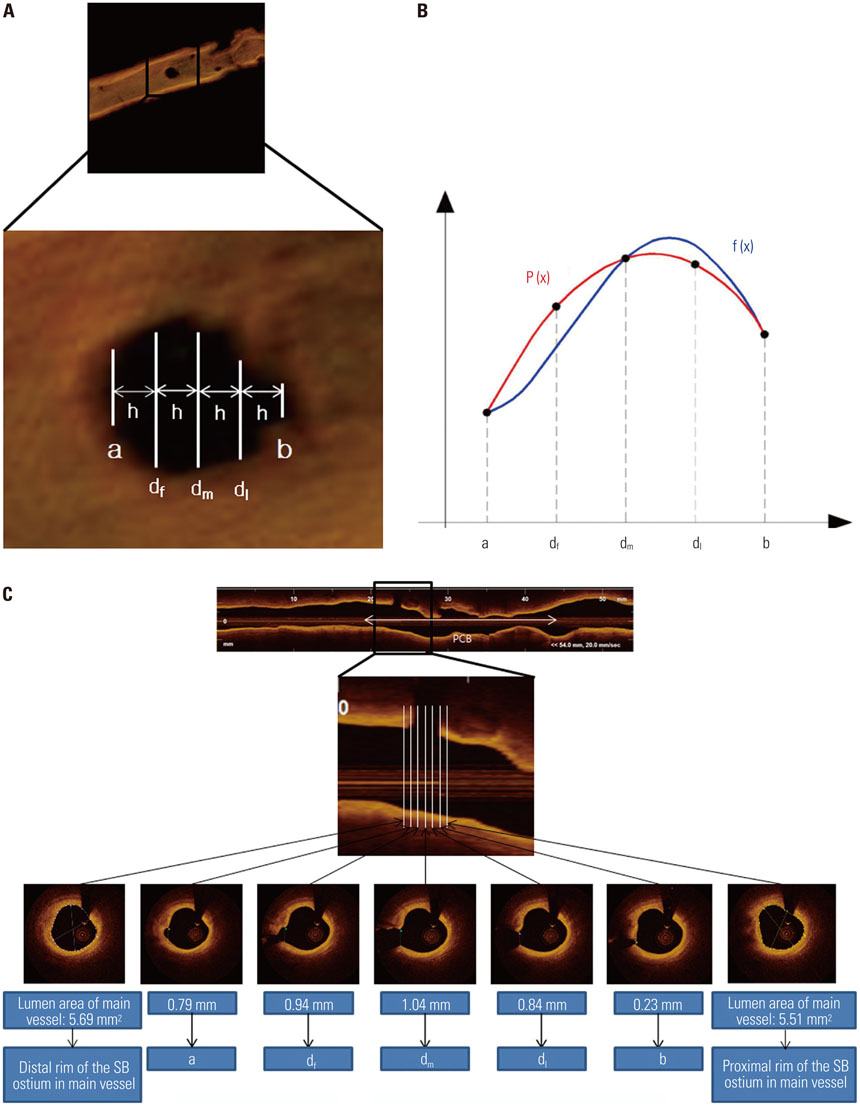
The effects on the side-branch (SB) ostium, following paclitaxel-coated balloon (PCB) treatment of de novo coronary lesions of main vessels have not been previously investigated. This study was aimed at evaluating the serial morphological changes of the SB ostium after PCB treatment of de novo coronary lesions of main vessels using optical coherence tomography (OCT).
MATERIALS AND METHODS
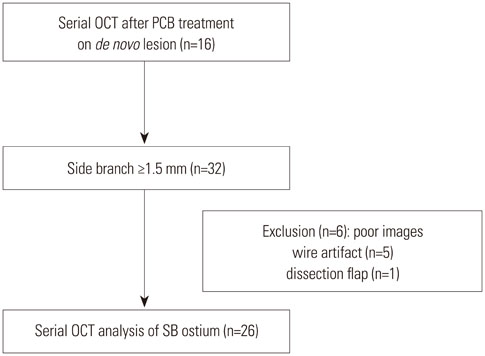
This prospective, single-center observational study enrolled patients with de novo lesions, which were traversed by at least one SB (≥1.5 mm) and were treated with PCB. The SB ostium was evaluated with serial angiographic and OCT assessments pre- and post-procedure, and at 9-months follow-up.
RESULTS
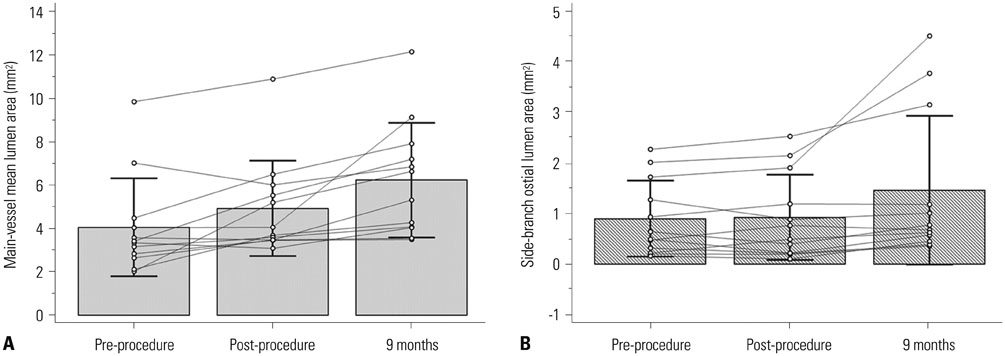
Sixteen main vessel lesions were successfully treated with PCB, and 26 SBs were included for analysis. Mean SB ostial lumen area increased at 9-months follow-up (0.92±0.68 mm2 pre-procedure, 1.03±0.77 mm2 post-procedure and 1.42±1.18 mm2 at 9-months). The SB ostial lumen area gain was 0.02±0.24 mm2 between pre- and post-procedure, 0.37±0.64 mm2 between post-procedure and 9-months, and 0.60±0.93 mm2 between pre-procedure and 9-months. The ostial lumen area increased by 3.9% [interquartile range (IQR) of -33.3 to 10.4%] between pre- and post-procedure, 52.1% (IQR of -0.7 to 77.3%) between post-procedure and 9-months and 76.1% (IQR of 18.2 to 86.6%) between pre-procedure and 9-months.
CONCLUSION
PCB treatment of de novo coronary lesions of main vessels resulted in an increase in the SB ostial lumen area at 9-months.
Keyword
MeSH Terms
-
Aged
Angioplasty, Balloon, Coronary/*methods
Coronary Angiography
Coronary Stenosis/diagnosis/*therapy
Coronary Vessels/*pathology
*Drug-Eluting Stents/adverse effects
Female
Humans
Male
Middle Aged
Paclitaxel/*administration & dosage
Prospective Studies
Tomography, Optical Coherence/*methods
Treatment Outcome
Tubulin Modulators/administration & dosage
Paclitaxel
Tubulin Modulators
Figure
Cited by 1 articles
-
A Comparison of Peri-Procedural Myocardial Infarction between Paclitaxel-Coated Balloon and Drug-Eluting Stent on De Novo Coronary Lesions
Ae-Young Her, Kyoung-Im Cho, Gillian Balbir Singh, Scot Garg, Yong Hoon Kim, Bon-Kwon Koo, Eun-Seok Shin
Yonsei Med J. 2017;58(1):99-104. doi: 10.3349/ymj.2017.58.1.99.
Reference
-
1. Steigen TK, Maeng M, Wiseth R, Erglis A, Kumsars I, Narbute I, et al. Randomized study on simple versus complex stenting of coronary artery bifurcation lesions: the Nordic bifurcation study. Circulation. 2006; 114:1955–1961.
Article2. Koo BK, Kang HJ, Youn TJ, Chae IH, Choi DJ, Kim HS, et al. Physiologic assessment of jailed side branch lesions using fractional flow reserve. J Am Coll Cardiol. 2005; 46:633–637.
Article3. Gil RJ, Vassilev D, Formuszewicz R, Rusicka-Piekarz T, Doganov A. The carina angle-new geometrical parameter associated with periprocedural side branch compromise and the long-term results in coronary bifurcation lesions with main vessel stenting only. J Interv Cardiol. 2009; 22:E1–E10.
Article4. Kleber FX, Rittger H, Bonaventura K, Zeymer U, Wöhrle J, Jeger R, et al. Drug-coated balloons for treatment of coronary artery disease: updated recommendations from a consensus group. Clin Res Cardiol. 2013; 102:785–797.
Article5. Dou K, Zhang D, Xu B, Yang Y, Yin D, Qiao S, et al. An angiographic tool for risk prediction of side branch occlusion in coronary bifurcation intervention: the RESOLVE score system (Risk prEdiction of Side branch OccLusion in coronary bifurcation interVEntion). JACC Cardiovasc Interv. 2015; 8(1 Pt A):39–46.
Article6. Scheller B, Speck U, Abramjuk C, Bernhardt U, Böhm M, Nickenig G. Paclitaxel balloon coating, a novel method for prevention and therapy of restenosis. Circulation. 2004; 110:810–814.
Article7. Sianos G, Morel MA, Kappetein AP, Morice MC, Colombo A, Dawkins K, et al. The SYNTAX Score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention. 2005; 1:219–227.8. Atkinson KE. An introduction to numerical analysis. New York: Wiley & Sons;1989. p. 111–120.9. Aliabadi D, Tilli FV, Bowers TR, Benzuly KH, Safian RD, Goldstein JA, et al. Incidence and angiographic predictors of side branch occlusion following high-pressure intracoronary stenting. Am J Cardiol. 1997; 80:994–997.
Article10. Park DW, Kim YH, Yun SC, Ahn JM, Lee JY, Kim WJ, et al. Frequency, causes, predictors, and clinical significance of peri-procedural myocardial infarction following percutaneous coronary intervention. Eur Heart J. 2013; 34:1662–1669.
Article11. Hahn JY, Chun WJ, Kim JH, Song YB, Oh JH, Koo BK, et al. Predictors and outcomes of side branch occlusion after main vessel stenting in coronary bifurcation lesions: results from the COBIS II Registry (COronary BIfurcation Stenting). J Am Coll Cardiol. 2013; 62:1654–1659.12. Pan M, de Lezo JS, Medina A, Romero M, Segura J, Pavlovic D, et al. Rapamycin-eluting stents for the treatment of bifurcated coronary lesions: a randomized comparison of a simple versus complex strategy. Am Heart J. 2004; 148:857–864.
Article13. Hildick-Smith D, de Belder AJ, Cooter N, Curzen NP, Clayton TC, Oldroyd KG, et al. Randomized trial of simple versus complex drug-eluting stenting for bifurcation lesions: the British Bifurcation Coronary Study: old, new, and evolving strategies. Circulation. 2010; 121:1235–1243.
Article14. Sheiban I, Albiero R, Marsico F, Dharmadhikari A, Tzifos V, Pagnotta P, et al. Immediate and long-term results of "T" stenting for bifurcation coronary lesions. Am J Cardiol. 2000; 85:1141–1144.
Article15. Koo BK, Park KW, Kang HJ, Cho YS, Chung WY, Youn TJ, et al. Physiological evaluation of the provisional side-branch intervention strategy for bifurcation lesions using fractional flow reserve. Eur Heart J. 2008; 29:726–732.
Article16. Koo BK, Waseda K, Kang HJ, Kim HS, Nam CW, Hur SH, et al. Anatomic and functional evaluation of bifurcation lesions undergoing percutaneous coronary intervention. Circ Cardiovasc Interv. 2010; 3:113–119.
Article17. Herdeg C, Oberhoff M, Baumbach A, Blattner A, Axel DI, Schröder S, et al. Local paclitaxel delivery for the prevention of restenosis: biological effects and efficacy in vivo. J Am Coll Cardiol. 2000; 35:1969–1976.
Article18. Kleber FX, Schulz A, Waliszewski M, Hauschild T, Böhm M, Dietz U, et al. Local paclitaxel induces late lumen enlargement in coronary arteries after balloon angioplasty. Clin Res Cardiol. 2015; 104:217–225.
Article19. Pires NM, Eefting D, de Vries MR, Quax PH, Jukema JW. Sirolimus and paclitaxel provoke different vascular pathological responses after local delivery in a murine model for restenosis on underlying atherosclerotic arteries. Heart. 2007; 93:922–927.
Article20. Gray WA, Granada JF. Drug-coated balloons for the prevention of vascular restenosis. Circulation. 2010; 121:2672–2680.
Article21. Axel DI, Kunert W, Göggelmann C, Oberhoff M, Herdeg C, Küttner A, et al. Paclitaxel inhibits arterial smooth muscle cell proliferation and migration in vitro and in vivo using local drug delivery. Circulation. 1997; 96:636–645.
Article22. Scheller B, Speck U, Schmitt A, Böhm M, Nickenig G. Addition of paclitaxel to contrast media prevents restenosis after coronary stent implantation. J Am Coll Cardiol. 2003; 42:1415–1420.
Article23. Speck U, Cremers B, Kelsch B, Biedermann M, Clever YP, Schaffner S, et al. Do pharmacokinetics explain persistent restenosis inhibition by a single dose of paclitaxel? Circ Cardiovasc Interv. 2012; 5:392–400.
Article24. Stella PR, Belkacemi A, Dubois C, Nathoe H, Dens J, Naber C, et al. A multicenter randomized comparison of drug-eluting balloon plus bare-metal stent versus bare-metal stent versus drug-eluting stent in bifurcation lesions treated with a single-stenting technique: six-month angiographic and 12-month clinical results of the drug-eluting balloon in bifurcations trial. Catheter Cardiovasc Interv. 2012; 80:1138–1146.
Article25. Mathey DG, Wendig I, Boxberger M, Bonaventura K, Kleber FX. Treatment of bifurcation lesions with a drug-eluting balloon: the PEPCAD V (Paclitaxel Eluting PTCA Balloon in Coronary Artery Disease) trial. EuroIntervention. 2011; 7:Suppl K. K61–K65.
Article26. Xu J, Hahn JY, Song YB, Choi SH, Choi JH, Lu C, et al. Carina shift versus plaque shift for aggravation of side branch ostial stenosis in bifurcation lesions: volumetric intravascular ultrasound analysis of both branches. Circ Cardiovasc Interv. 2012; 5:657–662.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Paclitaxel-Coated Balloon Treatment and Plain Old Balloon Angioplasty for De Novo Coronary Lesions
- Drug-Coated Balloon Treatment for De Novo Coronary Lesions: Current Status and Future Perspectives
- Drug-Coated Balloon Treatment for De Novo Coronary Artery Disease
- Drug-Coated Balloons for De Novo Coronary Artery Lesions: A Meta-Analysis of Randomized Clinical Trials
- A Comparison of Peri-Procedural Myocardial Infarction between Paclitaxel-Coated Balloon and Drug-Eluting Stent on De Novo Coronary Lesions