Yonsei Med J.
2016 Mar;57(2):490-495. 10.3349/ymj.2016.57.2.490.
Comparison between Steroid Injection and Stretching Exercise on the Scalene of Patients with Upper Extremity Paresthesia: Randomized Cross-Over Study
- Affiliations
-
- 1Department of Rehabilitation Medicine and Research Institute, Yonsei University College of Medicine, Seoul, Korea. bettertomo@yuhs.ac
- 2Department of Physical Medicine & Rehabilitation, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea.
- 3Department of Physical and Rehabilitation Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2374058
- DOI: http://doi.org/10.3349/ymj.2016.57.2.490
Abstract
- PURPOSE
To compare the therapeutic effects on upper extremity paresthesia of intra-muscular steroid injections into the scalene muscle with those of stretching exercise only.
MATERIALS AND METHODS
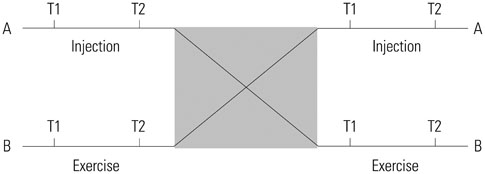
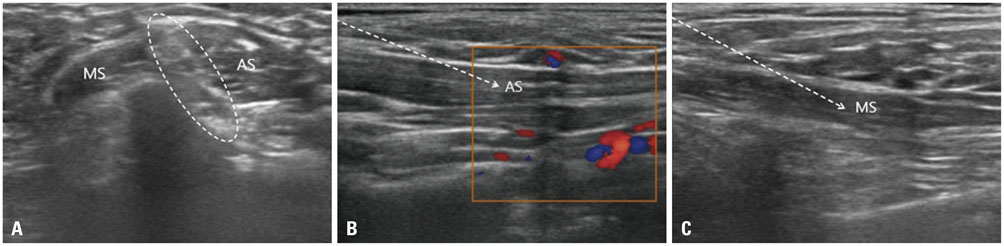
Twenty patients with upper extremity paresthesia who met the criteria were recruited to participate in this single-blind, crossover study. Fourteen of 20 patients were female. The average age was 45.0+/-10.5 years and duration of symptom was 12.2+/-8.7 months. Each participant completed one injection and daily exercise program for 2 weeks. After randomization, half of all patients received ultrasound-guided injection of scalene muscles before exercise, while the other was invested for the other patients.
RESULTS
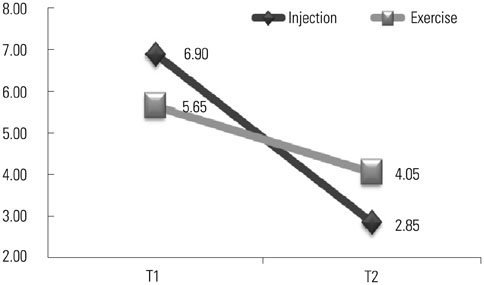
After two weeks, there was a significant decrease of the visual analog scale score of treatment effect compared with baseline in both groups (6.90 to 2.85 after injection and 5.65 to 4.05 after stretching exercise, p<0.01). However, injection resulted in greater improvements than stretching exercise (p<0.01). The number of patients with successful treatment, defined as >50% reduction in post-treatment visual analog scale, was 18 of 20 (90.0%) after injection, compared to 5 of 20 (25.0%) after stretching exercise. There were no cases of unintended brachial plexus block after injection.
CONCLUSION
Ultrasound-guided steroid injection or stretching exercise of scalene muscles led to reduced upper extremity paresthesia in patients who present with localized tenderness in the scalene muscle without electrodiagnostic test abnormalities, although injection treatment resulted in more improvements. The results suggest that symptoms relief might result from injection into the muscle alone not related to blockade of the brachial plexus.
MeSH Terms
-
Adult
Brachial Plexus/*drug effects
Cross-Over Studies
*Exercise Therapy
Female
Humans
*Injections, Intramuscular
Male
Middle Aged
Neck Muscles/drug effects
Pain/drug therapy
Pain Measurement
Paresthesia/*drug therapy/rehabilitation
Single-Blind Method
Thoracic Outlet Syndrome/diagnosis/*drug therapy
Treatment Outcome
Figure
Reference
-
1. Sanders RJ, Hammond SL, Rao NM. Thoracic outlet syndrome: a review. Neurologist. 2008; 14:365–373.2. Demondion X, Herbinet P, Van Sint Jan S, Boutry N, Chantelot C, Cotten A. Imaging assessment of thoracic outlet syndrome. Radiographics. 2006; 26:1735–1750.
Article3. Machleder HI, Moll F, Verity MA. The anterior scalene muscle in thoracic outlet compression syndrome. Histochemical and morphometric studies. Arch Surg. 1986; 121:1141–1144.
Article4. Braun RM, Sahadevan DC, Feinstein J. Confirmatory needle placement technique for scalene muscle block in the diagnosis of thoracic outlet syndrome. Tech Hand Up Extrem Surg. 2006; 10:173–176.
Article5. Novak CB, Mackinnon SE. Thoracic outlet syndrome. Orthop Clin North Am. 1996; 27:747–762.
Article6. Finlayson HC, O'Connor RJ, Brasher PM, Travlos A. Botulinum toxin injection for management of thoracic outlet syndrome: a double-blind, randomized, controlled trial. Pain. 2011; 152:2023–2028.
Article7. Rha DW, Han SH, Kim HJ, Won SY, Lee SC. Ultrasound-guided lateral approach for needle insertion into the subscapularis for treatment of spasticity. Arch Phys Med Rehabil. 2012; 93:1147–1152.
Article8. Shin HJ, Shin JC, Kim WS, Chang WH, Lee SC. Application of ultrasound-guided trigger point injection for myofascial trigger points in the subscapularis and pectoralis muscles to post-mastectomy patients: a pilot study. Yonsei Med J. 2014; 55:792–799.
Article9. Nishida T, Price SJ, Minieka MM. Medial antebrachial cutaneous nerve conduction in true neurogenic thoracic outlet syndrome. Electromyogr Clin Neurophysiol. 1993; 33:285–288.10. Muscolino JE. The Muscle and Bone Palpation Manual with Trigger Points, Referral Patterns and Stretching. St. Louis: Mosby;2008.11. Benzon HT, Rodes ME, Chekka K, Malik K, Pearce WH. Scalene muscle injections for neurogenic thoracic outlet syndrome: case series. Pain Pract. 2012; 12:66–70.
Article12. Machanic BI, Sanders RJ. Medial antebrachial cutaneous nerve measurements to diagnose neurogenic thoracic outlet syndrome. Ann Vasc Surg. 2008; 22:248–254.
Article13. Wilbourn AJ. Thoracic outlet syndromes. Neurol Clin. 1999; 17:477–497. vi
Article14. Jordan SE, Machleder HI. Diagnosis of thoracic outlet syndrome using electrophysiologically guided anterior scalene blocks. Ann Vasc Surg. 1998; 12:260–264.
Article15. Jordan SE, Ahn SS, Freischlag JA, Gelabert HA, Machleder HI. Selective botulinum chemodenervation of the scalene muscles for treatment of neurogenic thoracic outlet syndrome. Ann Vasc Surg. 2000; 14:365–369.
Article16. Christo PJ, Christo DK, Carinci AJ, Freischlag JA. Single CT-guided chemodenervation of the anterior scalene muscle with botulinum toxin for neurogenic thoracic outlet syndrome. Pain Med. 2010; 11:504–511.
Article17. Torriani M, Gupta R, Donahue DM. Botulinum toxin injection in neurogenic thoracic outlet syndrome: results and experience using a ultrasound-guided approach. Skeletal Radiol. 2010; 39:973–980.
Article18. Olinger AB, Homier P. Functional anatomy of human scalene musculature: rotation of the cervical spine. J Manipulative Physiol Ther. 2010; 33:594–602.
Article19. Sanders RJ, Jackson CG, Banchero N, Pearce WH. Scalene muscle abnormalities in traumatic thoracic outlet syndrome. Am J Surg. 1990; 159:231–236.
Article20. Granter R. Treatments used for musculoskeletal conditions: more choices and more evidence. In : Brukner P, Khan K, editors. Brukner & Khan's Clinical Sports Medicine. 4th ed. Sydney: McGraw-Hill Education;2011. p. 164–201.21. Clendenen SR, Candler SA, Osborne MD, Palmer SC, Duench S, Glynn L, et al. Needle placement for piriformis injection using 3-D imaging. Pain Physician. 2013; 16:E301–E310.22. Lento P, Ihm J, Kennedy D, Visco C. Peripheral joint and soft tissue injection techniques. In : Braddom RL, editor. Physical Medicine and Rehabilitation. 4th ed. Philadelphia: Saunders;2010. p. 517–540.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Stretching Exercise on the Head Speed of Golf Club and Driving Distance
- Thoracic Outlet Syndrome Caused by Automobile Accident
- The Efficacy of Scalene Injection in Thoracic Outlet Syndrome
- Eyelid Stretching Exercise Performed in Overcorrection after Levator Resection in Congenital Ptosis
- Upper Limb Pain and Paresthesia in a Post-Stroke Patient Treated with Ultrasound-Guided Electrical Twitch-Obtaining Intramuscular Stimulation (ETOIMS) of Scalene Muscles