Yonsei Med J.
2016 Mar;57(2):426-429. 10.3349/ymj.2016.57.2.426.
Possible Prevention of Neonatal Death: A Regional Population-Based Study in Japan
- Affiliations
-
- 1Department of Community Perinatal Medicine, Shiga University of Medical Science, Otsu, Japan. koshida@belle.shiga-med.ac.jp
- 2Department of Pediatrics, Shiga University of Medical Science, Otsu, Japan.
- 3Department of Obstetrics and Gynecology, Shiga University of Medical Science, Otsu, Japan.
- KMID: 2374049
- DOI: http://doi.org/10.3349/ymj.2016.57.2.426
Abstract
- PURPOSE
The neonatal mortality rate in Japan has currently been at the lowest level in the world. However, it is unclear whether there are still some potentially preventable neonatal deaths. We, therefore, aimed to examine the backgrounds of neonatal death and the possibilities of prevention in a region of Japan.
MATERIALS AND METHODS
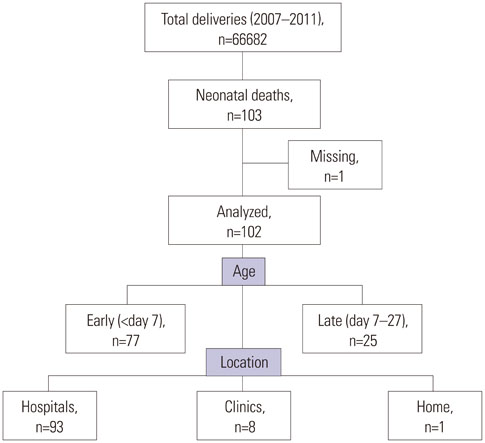
This is a population-based study of neonatal death in Shiga Prefecture of Japan.
RESULTS
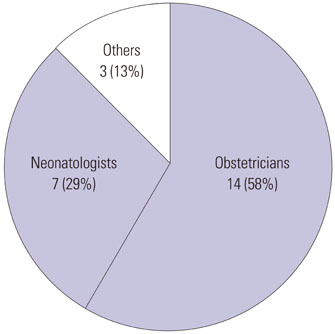
The 103 neonatal deaths in our prefecture between 2007 and 2011 were included. After reviewing by a peer-review team, we classified the backgrounds of these neonatal deaths and analyzed end-of-life care approaches associated with prenatal diagnosis. Furthermore, we evaluated the possibilities of preventable neonatal death, suggesting specific recommendations for its prevention. We analyzed 102 (99%) of the neonatal deaths. Congenital malformations and extreme prematurity were the first and the second most common causes of death, respectively. More than half of the congenital abnormalities (59%) including malformations and chromosome abnormality had been diagnosed before births. We had 22 neonates with non-intensive care including eighteen cases with congenital abnormality and four with extreme prematurity. Twenty three cases were judged to have had some possibility of prevention with one having had a strong possibility of prevention. Among specific recommendations of preventable neonatal death, more than half of them were for obstetricians.
CONCLUSION
There is room to reduce neonatal deaths in Japan. Prevention of neonatal death requires grater prenatal care by obstetricians before birth rather than improved neonatal care by neonatologists after birth.
MeSH Terms
Figure
Reference
-
1. Hamilton BE, Hoyert DL, Martin JA, Strobino DM, Guyer B. Annual summary of vital statistics: 2010-2011. Pediatrics. 2013; 131:548–558.
Article2. Rajaratnam JK, Marcus JR, Flaxman AD, Wang H, Levin-Rector A, Dwyer L, et al. Neonatal, postneonatal, childhood, and under-5 mortality for 187 countries, 1970-2010: a systematic analysis of progress towards Millennium Development Goal 4. Lancet. 2010; 375:1988–2008.
Article3. Ministry of Health, Labour and Welfare. Prompt Vital Statistics Report, October 2012. Tokyo, Japan: Ministry of Health, Labour and Welfare;2012.4. Sameshima H, Ikenoue T. Miyazaki Perinatal Data Group. Risk factors for perinatal deaths in Southern Japan: population-based analysis from 1998 to 2005. Early Hum Dev. 2008; 84:319–323.
Article5. Eventov-Friedman S, Kanevsky H, Bar-Oz B. Neonatal end-of-life care: a single-center NICU experience in Israel over a decade. Pediatrics. 2013; 131:e1889–e1896.
Article6. Berger TM, Hofer A. Causes and circumstances of neonatal deaths in 108 consecutive cases over a 10-year period at the Children's Hospital of Lucerne, Switzerland. Neonatology. 2009; 95:157–163.
Article7. Simpson CD, Ye XY, Hellmann J, Tomlinson C. Trends in cause-specific mortality at a Canadian outborn NICU. Pediatrics. 2010; 126:e1538–e1544.
Article8. Mathews TJ, Miniño AM, Osterman MJ, Strobino DM, Guyer B. Annual summary of vital statistics: 2008. Pediatrics. 2011; 127:146–157.
Article9. Bianchi DW, Parker RL, Wentworth J, Madankumar R, Saffer C, Das AF, et al. DNA sequencing versus standard prenatal aneuploidy screening. N Engl J Med. 2014; 370:799–808.
Article10. Greene MF, Phimister EG. Screening for trisomies in circulating DNA. N Engl J Med. 2014; 370:874–875.
Article11. Tudorache S, Chiuţu LC, Iliescu DG, Georgescu R, Stoica GA, Simionescu CE, et al. Prenatal diagnosis and perinatal outcome in congenital diaphragmatic hernia. Single tertiary center report. Rom J Morphol Embryol. 2014; 55:823–833.12. Anagnostou K, Messenger L, Yates R, Kelsall W. Outcome of infants with prenatally diagnosed congenital heart disease delivered outside specialist paediatric cardiac centres. Arch Dis Child Fetal Neonatal Ed. 2013; 98:F218–F221.
Article13. Oster ME, Kim CH, Kusano AS, Cragan JD, Dressler P, Hales AR, et al. A population-based study of the association of prenatal diagnosis with survival rate for infants with congenital heart defects. Am J Cardiol. 2014; 113:1036–1040.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Neonatal Research Network of Japan and Neonatal Database
- Potential Capacity of Korean Neonatal Transport Team Model Accompanying Doctors: Citizen Security Medical Service Development Project Experience
- Evolution of Asthma Concept and Effect of Current Asthma Management Guidelines
- Long-Term Care System in Japan
- Mortality Analysis of Surgical Neonates : A 20-year Experience by A Single Surgeon