Yonsei Med J.
2016 Mar;57(2):358-364. 10.3349/ymj.2016.57.2.358.
Clinical Prognostic Factors in 86 Chinese Patients with Primary Myelodysplastic Syndromes and Trisomy 8: A Single Institution Experience
- Affiliations
-
- 1Department of Medical Oncology, ShaanXi Provincial People's Hospital, Xi'an, Shaanxi, P.R. China.
- 2Department of Hematology, Union Hospital, Tongji Medical College of Huazhong University of Science and Technology, Wuhan, Hubei, P.R. China. lxy_wuhanxh@sina.com
- KMID: 2374040
- DOI: http://doi.org/10.3349/ymj.2016.57.2.358
Abstract
- PURPOSE
The objective was to determine the characteristics and prognostic factors of 86 Chinese patients with trisomy 8 aberrations and compare the prognostic value of International Prognostic System (IPSS) and Revised IPSS (IPSS-R) in this cohort.
MATERIALS AND METHODS
A total of 86 cases diagnosed with primary myelodysplastic syndromes (MDS) with isolated tr8 or with tr8 and other additional cytogenetic aberrations diagnosed and treated at the Union Hospital, Tongji Medical College of Huazhong University of Science and Technology between July 2002 and March 2013 were reviewed.
RESULTS
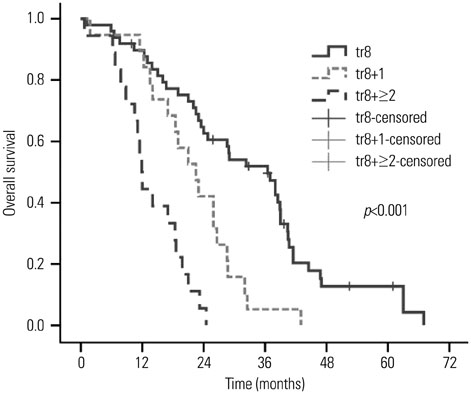
The median survival of the entire group was 23.0 months, and acute myeloid leukemia (AML) developed in 43% (37/86) patients within the follow up time. The univariate analysis revealed that overall survival (OS) was correlated with age, thrombocytopenia, absolute neutrophil count, marrow blasts, cytogenetic status and red blood cell transfusion at diagnosis, and the multivariate analysis revealed that age, marrow blasts, cytogenetic status and transfusion dependence were independent parameters for the OS. The cytogenetic complexity and marrow blasts had the strongest impact on the AML transformation by multivariate analysis. Comparing the two prognostic systems, both two systems could successfully discriminate risk groups for survival. IPSS-R was more refined than IPSS for predicting OS, but had no advantage in predicting the risk of AML development.
CONCLUSION
This study confirmed the influence of clinical factors on the prognosis of 86 Chinese MDS patients with trisomy 8. In addition, IPSS-R can further refine prognostic discrimination in the IPSS risk categories.
MeSH Terms
Figure
Reference
-
1. Greenberg PL, Young NS, Gattermann N. Myelodysplastic syndromes. Hematology Am Soc Hematol Educ Program. 2002; 136–161.
Article2. Nimer SD. Myelodysplastic syndromes. Blood. 2008; 111:4841–4851.
Article3. Nolte F, Hofmann WK. Myelodysplastic syndromes: molecular pathogenesis and genomic changes. Ann Hematol. 2008; 87:777–795.
Article4. Mufti GJ, Bennett JM, Goasguen J, Bain BJ, Baumann I, Brunning R, et al. Diagnosis and classification of myelodysplastic syndrome: International Working Group on Morphology of myelodysplastic syndrome (IWGM-MDS) consensus proposals for the definition and enumeration of myeloblasts and ring sideroblasts. Haematologica. 2008; 93:1712–1717.
Article5. Solé F, Luño E, Sanzo C, Espinet B, Sanz GF, Cervera J, et al. Identification of novel cytogenetic markers with prognostic significance in a series of 968 patients with primary myelodysplastic syndromes. Haematologica. 2005; 90:1168–1178.6. Bernasconi P, Klersy C, Boni M, Cavigliano PM, Calatroni S, Giardini I, et al. World Health Organization classification in combination with cytogenetic markers improves the prognostic stratification of patients with de novo primary myelodysplastic syndromes. Br J Haematol. 2007; 137:193–205.
Article7. Malcovati L, Germing U, Kuendgen A, Della Porta MG, Pascutto C, Invernizzi R, et al. Time-dependent prognostic scoring system for predicting survival and leukemic evolution in myelodysplastic syndromes. J Clin Oncol. 2007; 25:3503–3510.
Article8. Greenberg PL, Tuechler H, Schanz J, Sanz G, Garcia-Manero G, Solé F, et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood. 2012; 120:2454–2465.
Article9. Germing U, Kündgen A. Prognostic scoring systems in MDS. Leuk Res. 2012; 36:1463–1469.
Article10. Greenberg P, Cox C, LeBeau MM, Fenaux P, Morel P, Sanz G, et al. International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood. 1997; 89:2079–2088.
Article11. Paulsson K, Johansson B. Trisomy 8 as the sole chromosomal aberration in acute myeloid leukemia and myelodysplastic syndromes. Pathol Biol (Paris). 2007; 55:37–48.
Article12. Irons RD, Wang X, Gross SA, Bao L, Ryder J, Chen Y, et al. Prevalence of MDS subtypes in Shanghai, China: a comparison of the World Health Organization and French American British classifications. Leuk Res. 2006; 30:769–775.
Article13. Qu S, Xu Z, Zhang Y, Qin T, Zhang T, Cui R, et al. Impacts of cytogenetic categories in the Revised International Prognostic Scoring System on the prognosis of primary myelodysplastic syndromes: results of a single-center study. Leuk Lymphoma. 2012; 53:940–946.
Article14. Xiao Y, Wei J, Chen Y, Zhang K, Zhou J, Zhang Y. Trisomy 8 is the most frequent cytogenetic abnormality in de novo myelodysplastic syndrome in China. Onkologie. 2012; 35:100–106.
Article15. Ma Y, Wang X, Xu X, Lin G. Prognostic value of trisomy 8 in primary myelodysplastic syndrome. Intern Med J. 2010; 40:697–703.
Article16. Cazzola M, Della Porta MG, Travaglino E, Malcovati L. Classification and prognostic evaluation of myelodysplastic syndromes. Semin Oncol. 2011; 38:627–634.
Article17. Sloand EM, Mainwaring L, Fuhrer M, Ramkissoon S, Risitano AM, Keyvanafar K, et al. Preferential suppression of trisomy 8 compared with normal hematopoietic cell growth by autologous lymphocytes in patients with trisomy 8 myelodysplastic syndrome. Blood. 2005; 106:841–851.
Article18. Olnes MJ, Shenoy A, Weinstein B, Pfannes L, Loeliger K, Tucker Z, et al. Directed therapy for patients with myelodysplastic syndromes (MDS) by suppression of cyclin D1 with ON 01910.Na. Leuk Res. 2012; 36:982–989.
Article19. Malcovati L, Della Porta MG, Strupp C, Ambaglio I, Kuendgen A, Nachtkamp K, et al. Impact of the degree of anemia on the outcome of patients with myelodysplastic syndrome and its integration into the WHO classification-based Prognostic Scoring System (WPSS). Haematologica. 2011; 96:1433–1440.
Article20. Gonzalez Garcia JR, Meza-Espinoza JP. Use of the International System for Human Cytogenetic Nomenclature (ISCN). Blood. 2006; 108:3952–3953.
Article21. Chun K, Hagemeijer A, Iqbal A, Slovak ML. Implementation of standardized international karyotype scoring practices is needed to provide uniform and systematic evaluation for patients with myelodysplastic syndrome using IPSS criteria: An International Working Group on MDS Cytogenetics Study. Leuk Res. 2010; 34:160–165.
Article22. Vardiman JW, Thiele J, Arber DA, Brunning RD, Borowitz MJ, Porwit A, et al. The 2008 revision of the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia: rationale and important changes. Blood. 2009; 114:937–951.
Article23. Wellner JA. On an exponential bound for the Kaplan-Meier estimator. Lifetime Data Anal. 2007; 13:481–496.
Article24. Gill RD. Multistate life-tables and regression models. Math Popul Stud. 1992; 3:259–276.
Article25. Pozdnyakova O, Miron PM, Tang G, Walter O, Raza A, Woda B, et al. Cytogenetic abnormalities in a series of 1,029 patients with primary myelodysplastic syndromes: a report from the US with a focus on some undefined single chromosomal abnormalities. Cancer. 2008; 113:3331–3340.
Article26. Matsuda A, Germing U, Jinnai I, Misumi M, Kuendgen A, Knipp S, et al. Difference in clinical features between Japanese and German patients with refractory anemia in myelodysplastic syndromes. Blood. 2005; 106:2633–2640.
Article27. Lee JJ, Kim HJ, Chung IJ, Kim JS, Sohn SK, Kim BS, et al. Comparisons of prognostic scoring systems for myelodysplastic syndromes: a Korean multicenter study. Leuk Res. 1999; 23:425–432.
Article28. Kuendgen A, Matsuda A, Germing U. Differences in epidemiology of MDS between Western and Eastern countries: ethnic differences or environmental influence? Leuk Res. 2007; 31:103–104.
Article29. Chen B, Zhao WL, Jin J, Xue YQ, Cheng X, Chen XT, et al. Clinical and cytogenetic features of 508 Chinese patients with myelodysplastic syndrome and comparison with those in Western countries. Leukemia. 2005; 19:767–775.
Article30. Li L, Liu XP, Nie L, Yu MH, Zhang Y, Qin TJ, et al. Unique cytogenetic features of primary myelodysplastic syndromes in Chinese patients. Leuk Res. 2009; 33:1194–1198.
Article31. Al Ameri A, Jabbour E, Garcia-Manero G, O'Brien S, Faderl S, Ravandi F, et al. Significance of thrombocytopenia in myelodysplastic syndromes: associations and prognostic implications. Clin Lymphoma Myeloma Leuk. 2011; 11:237–241.
Article32. Lee JH, Lee JH, Shin YR, Lee JS, Kim WK, Chi HS, et al. Application of different prognostic scoring systems and comparison of the FAB and WHO classifications in Korean patients with myelodysplastic syndrome. Leukemia. 2003; 17:305–313.
Article33. Pereira A, Nomdedeu M, Aguilar JL, Belkaid M, Carrió A, Cobo F, et al. Transfusion intensity, not the cumulative red blood cell transfusion burden, determines the prognosis of patients with myelodysplastic syndrome on chronic transfusion support. Am J Hematol. 2011; 86:245–250.
Article34. Saumell S, Florensa L, Luño E, Sanzo C, Cañizo C, Hernández JM, et al. Prognostic value of trisomy 8 as a single anomaly and the influence of additional cytogenetic aberrations in primary myelodysplastic syndromes. Br J Haematol. 2012; 159:311–321.
Article35. Haase D, Germing U, Schanz J, Pfeilstöcker M, Nösslinger T, Hildebrandt B, et al. New insights into the prognostic impact of the karyotype in MDS and correlation with subtypes: evidence from a core dataset of 2124 patients. Blood. 2007; 110:4385–4395.
Article36. Schanz J, Steidl C, Fonatsch C, Pfeilstöcker M, Nösslinger T, Tuechler H, et al. Coalesced multicentric analysis of 2,351 patients with myelodysplastic syndromes indicates an underestimation of poor-risk cytogenetics of myelodysplastic syndromes in the international prognostic scoring system. J Clin Oncol. 2011; 29:1963–1970.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anesthetic experience for laparoscopic cholecystectomy in a patient with myelodysplastic syndrome with trisomy 8 mosaicism syndrome
- Classifications and prognostic scoring systems in myelodysplastic syndrome
- Myelodysplastic syndromes and overlap syndromes
- Trisomy 9, As a Sole Chromosomal Aberration in Refractory Anemia with Excess Blasts-II
- A Case of Behcet's Disease Associated with Schizophrenia and Myelodysplastic Syndrome with Trisomy 8 and 9