Yonsei Med J.
2016 Mar;57(2):342-349. 10.3349/ymj.2016.57.2.342.
Early Experience of Novel Oral Anticoagulants in Catheter Ablation for Atrial Fibrillation: Efficacy and Safety Comparison to Warfarin
- Affiliations
-
- 1Department of Cardiology, Yonsei University Health System, Seoul, Korea. hnpak@yuhs.ac
- KMID: 2374038
- DOI: http://doi.org/10.3349/ymj.2016.57.2.342
Abstract
- PURPOSE
Compared with warfarin, novel oral anticoagulants (NOACs) are convenient to use, although they require a blanking period immediately before radiofrequency catheter ablation for atrial fibrillation (AF). We compared NOACs and uninterrupted warfarin in the peri-procedural period of AF ablation.
MATERIALS AND METHODS
We compared 141 patients treated with peri-procedural NOACs (72% men; 58+/-11 years old; 71% with paroxysmal AF) and 281 age-, sex-, AF type-, and history of stroke-matched patients treated with uninterrupted warfarin. NOACs were stopped 24 hours before the procedure and restarted on the same procedure day after hemostasis was achieved.
RESULTS
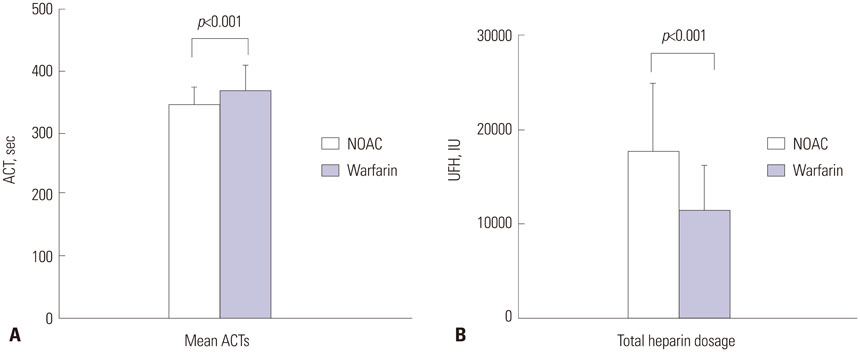
We found no difference in the CHA2DS2-VASc (p=0.376) and HAS-BLED scores (p=0.175) between the groups. The preprocedural anticoagulation duration was significantly shorter in the NOAC group (76.3+/-110.7 days) than in the warfarin group (274.7+/-582.7 days, p<0.001). The intra-procedural total heparin requirement was higher (p<0.001), although mean activated clotting time was shorter (350.0+/-25.0 s vs. 367.4+/-42.9 s, p<0.001), in the NOAC group than in the warfarin group. There was no significant difference in thromboembolic events (1.4% vs. 0%, p=0.111) or major bleeding (1.4% vs. 3.9%, p=0.235) between the NOAC and warfarin groups. Minor stroke occurred in two cases within 10 hours of the procedure (underlying CHA2DS2-VASc scores 0 and 1) in the NOAC group.
CONCLUSION
Pre-procedural anticoagulation duration was shorter and intra-procedural heparin requirement was higher with NOAC than with uninterrupted warfarin during AF ablation. Although the peri-procedural thromboembolism and bleeding incidences did not differ, minor stroke occurred in two cases in the NOAC group.
MeSH Terms
-
Aged
Anticoagulants/*therapeutic use
Atrial Fibrillation/complications/*drug therapy/*surgery
Catheter Ablation/*methods
Female
Follow-Up Studies
Hemorrhage/epidemiology
Heparin
Humans
Incidence
Male
Middle Aged
Postoperative Complications/epidemiology
Stroke/epidemiology
Thromboembolism/epidemiology
Treatment Outcome
Warfarin/administration & dosage/*therapeutic use
Anticoagulants
Heparin
Warfarin
Figure
Cited by 1 articles
-
Unilateral versus Bilateral Groin Puncture for Atrial Fibrillation Ablation: Multi-Center Prospective Randomized Study
Hee Tae Yu, Dong Geum Shin, Jaemin Shim, Gi-Byoung Nam, Won Woo Yoo, Ji Hyun Lee, Tae-Hoon Kim, Jae-Sun Uhm, Boyoung Joung, Moon-Hyoung Lee, Young-Hoon Kim, Hui-Nam Pak
Yonsei Med J. 2019;60(4):360-367. doi: 10.3349/ymj.2019.60.4.360.
Reference
-
1. Haïssaguerre M, Jaïs P, Shah DC, Takahashi A, Hocini M, Quiniou G, et al. Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. N Engl J Med. 1998; 339:659–666.
Article2. January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014; 64:e1–e76.3. Spragg DD, Dalal D, Cheema A, Scherr D, Chilukuri K, Cheng A, et al. Complications of catheter ablation for atrial fibrillation: incidence and predictors. J Cardiovasc Electrophysiol. 2008; 19:627–631.
Article4. Cappato R, Calkins H, Chen SA, Davies W, Iesaka Y, Kalman J, et al. Prevalence and causes of fatal outcome in catheter ablation of atrial fibrillation. J Am Coll Cardiol. 2009; 53:1798–1803.
Article5. Page SP, Herring N, Hunter RJ, Withycombe E, Lovell M, Wali G, et al. Periprocedural stroke risk in patients undergoing catheter ablation for atrial fibrillation on uninterrupted warfarin. J Cardiovasc Electrophysiol. 2014; 25:585–590.
Article6. Calkins H, Kuck KH, Cappato R, Brugada J, Camm AJ, Chen SA, et al. 2012 HRS/EHRA/ECAS Expert Consensus Statement on Catheter and Surgical Ablation of Atrial Fibrillation: recommendations for patient selection, procedural techniques, patient management and follow-up, definitions, endpoints, and research trial design. Europace. 2012; 14:528–606.
Article7. Eitel C, Koch J, Sommer P, John S, Kircher S, Bollmann A, et al. Novel oral anticoagulants in a real-world cohort of patients undergoing catheter ablation of atrial fibrillation. Europace. 2013; 15:1587–1593.
Article8. Hohnloser SH, Camm AJ. Safety and efficacy of dabigatran etexilate during catheter ablation of atrial fibrillation: a meta-analysis of the literature. Europace. 2013; 15:1407–1411.
Article9. Providência R, Albenque JP, Combes S, Bouzeman A, Casteigt B, Combes N, et al. Safety and efficacy of dabigatran versus warfarin in patients undergoing catheter ablation of atrial fibrillation: a systematic review and meta-analysis. Heart. 2014; 100:324–335.
Article10. Bin Abdulhak AA, Khan AR, Tleyjeh IM, Spertus JA, Sanders SU, Steigerwalt KE, et al. Safety and efficacy of interrupted dabigatran for peri-procedural anticoagulation in catheter ablation of atrial fibrillation: a systematic review and meta-analysis. Europace. 2013; 15:1412–1420.
Article11. Lakkireddy D, Reddy YM, Di Biase L, Vallakati A, Mansour MC, Santangeli P, et al. Feasibility and safety of uninterrupted rivaroxaban for periprocedural anticoagulation in patients undergoing radiofrequency ablation for atrial fibrillation: results from a multicenter prospective registry. J Am Coll Cardiol. 2014; 63:982–988.
Article12. Dillier R, Ammar S, Hessling G, Kaess B, Pavaci H, Buiatti A, et al. Safety of continuous periprocedural rivaroxaban for patients undergoing left atrial catheter ablation procedures. Circ Arrhythm Electrophysiol. 2014; 7:576–582.
Article13. Kwak JJ, Pak HN, Jang JK, Kim SK, Park JH, Choi JI, et al. Safety and convenience of continuous warfarin strategy during the periprocedural period in patients who underwent catheter ablation of atrial fibrillation. J Cardiovasc Electrophysiol. 2010; 21:620–625.
Article14. Heidbuchel H, Verhamme P, Alings M, Antz M, Hacke W, Oldgren J, et al. European Heart Rhythm Association Practical Guide on the use of new oral anticoagulants in patients with non-valvular atrial fibrillation. Europace. 2013; 15:625–651.
Article15. Kastrati A, Neumann FJ, Mehilli J, Byrne RA, Iijima R, Büttner HJ, et al. Bivalirudin versus unfractionated heparin during percutaneous coronary intervention. N Engl J Med. 2008; 359:688–696.
Article16. Kussmaul WG 3rd, Buchbinder M, Whitlow PL, Aker UT, Heuser RR, King SB, et al. Rapid arterial hemostasis and decreased access site complications after cardiac catheterization and angioplasty: results of a randomized trial of a novel hemostatic device. J Am Coll Cardiol. 1995; 25:1685–1692.
Article17. Park JH, Pak HN, Choi EJ, Jang JK, Kim SK, Choi DH, et al. The relationship between endocardial voltage and regional volume in electroanatomical remodeled left atria in patients with atrial fibrillation: comparison of three-dimensional computed tomographic images and voltage mapping. J Cardiovasc Electrophysiol. 2009; 20:1349–1356.
Article18. Shim J, Joung B, Park JH, Uhm JS, Lee MH, Pak HN. Long duration of radiofrequency energy delivery is an independent predictor of clinical recurrence after catheter ablation of atrial fibrillation: over 500 cases experience. Int J Cardiol. 2013; 167:2667–2672.
Article19. D'Agostino RB Jr. Propensity scores in cardiovascular research. Circulation. 2007; 115:2340–2343.20. Ruff CT, Giugliano RP, Braunwald E, Hoffman EB, Deenadayalu N, Ezekowitz MD, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014; 383:955–962.
Article21. Kim JS, She F, Jongnarangsin K, Chugh A, Latchamsetty R, Ghanbari H, et al. Dabigatran vs warfarin for radiofrequency catheter ablation of atrial fibrillation. Heart Rhythm. 2013; 10:483–489.
Article22. Bassiouny M, Saliba W, Rickard J, Shao M, Sey A, Diab M, et al. Use of dabigatran for periprocedural anticoagulation in patients undergoing catheter ablation for atrial fibrillation. Circ Arrhythm Electrophysiol. 2013; 6:460–466.
Article23. Kaseno K, Naito S, Nakamura K, Sakamoto T, Sasaki T, Tsukada N, et al. Efficacy and safety of periprocedural dabigatran in patients undergoing catheter ablation of atrial fibrillation. Circ J. 2012; 76:2337–2342.
Article24. Maddox W, Kay GN, Yamada T, Osorio J, Doppalapudi H, Plumb VJ, et al. Dabigatran versus warfarin therapy for uninterrupted oral anticoagulation during atrial fibrillation ablation. J Cardiovasc Electrophysiol. 2013; 24:861–865.
Article25. Yamaji H, Murakami T, Hina K, Higashiya S, Kawamura H, Murakami M, et al. Usefulness of dabigatran etexilate as periprocedural anticoagulation therapy for atrial fibrillation ablation. Clin Drug Investig. 2013; 33:409–418.
Article26. Singer DE, Chang Y, Fang MC, Borowsky LH, Pomernacki NK, Udaltsova N, et al. The net clinical benefit of warfarin anticoagulation in atrial fibrillation. Ann Intern Med. 2009; 151:297–305.
Article27. Uhm JS, Won H, Joung B, Nam GB, Choi KJ, Lee MH, et al. Safety and efficacy of switching anticoagulation to aspirin three months after successful radiofrequency catheter ablation of atrial fibrillation. Yonsei Med J. 2014; 55:1238–1245.
Article28. Hirsh J, Bauer KA, Donati MB, Gould M, Samama MM, Weitz JI. American College of Chest Physicians. Parenteral anticoagulants: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008; 133:6 Suppl. 141S–159S.29. Nin T, Sairaku A, Yoshida Y, Kamiya H, Tatematsu Y, Nanasato M, et al. A randomized controlled trial of dabigatran versus warfarin for periablation anticoagulation in patients undergoing ablation of atrial fibrillation. Pacing Clin Electrophysiol. 2013; 36:172–179.
Article30. Kim YD, Lee KY, Nam HS, Han SW, Lee JY, Cho HJ, et al. Factors associated with ischemic stroke on therapeutic anticoagulation in patients with nonvalvular atrial fibrillation. Yonsei Med J. 2015; 56:410–417.
Article31. Han JH, Shin DH, Lee HJ, Kim YJ, Lee SH, Shim J, et al. Routine preprocedural transesophageal echocardiography might not be necessary for stroke prevention evaluation in AF patients on anticoagulation therapy. Int J Cardiol. 2013; 168:1992–1996.
Article32. Cappato R, Marchlinski FE, Hohnloser SH, Naccarelli GV, Xiang J, Wilber DJ, et al. Uninterrupted rivaroxaban vs. uninterrupted vitamin K antagonists for catheter ablation in non-valvular atrial fibrillation. Eur Heart J. 2015; 36:1805–1811.
Article33. Chang RJ, Doherty TM, Goldberg SL. How does warfarin affect the activated coagulation time? Am Heart J. 1998; 136:477–479.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Early Complications of Oral Anticoagulants after Totally Thoracoscopic Ablation: Warfarin versus Non-vitamin K Antagonist Oral Anticoagulants
- New oral anticoagulants
- Cerebral Infarction After Radiofrequency Catheter Ablation in Patients With Paroxysmal Atrial Fibrillation
- Practical Issues to Prevent Stroke Associated with Non-valvular Atrial Fibrillation
- Use of NOAC in Cardioversion