Diagnosis and Treatment of Nontuberculous Mycobacterial Lung Disease
- Affiliations
-
- 1Department of Internal Medicine, Chonnam National University Hospital, Gwangju, Korea.
- 2Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. wjkoh@skku.edu
- KMID: 2373660
- DOI: http://doi.org/10.3346/jkms.2016.31.5.649
Abstract
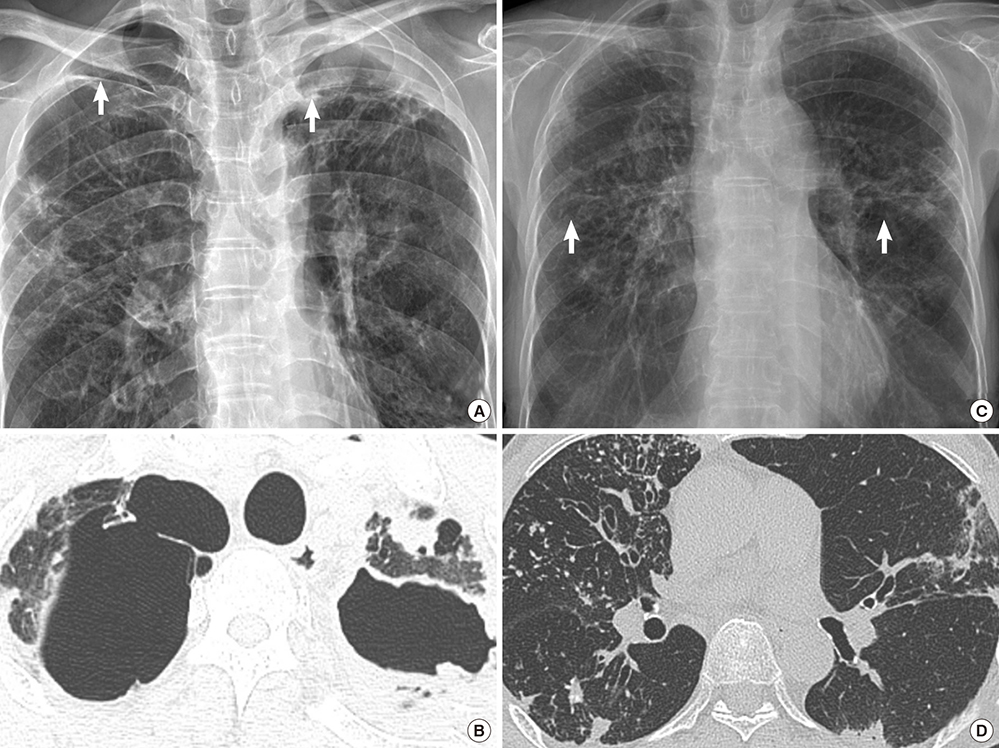
- Nontuberculous mycobacteria (NTM) are ubiquitous organisms; their isolation from clinical specimens does not always indicate clinical disease. The incidence of NTM lung diseases has been increasing worldwide. Although the geographic diversity of NTM species is well known, Mycobacterium avium complex (MAC), M. abscessus complex (MABC), and M. kansasii are the most commonly encountered and important etiologic organisms. Two distinct types of NTM lung diseases have been reported, namely fibrocavitary and nodular bronchiectatic forms. For laboratory diagnosis of NTM lung diseases, both liquid and solid media cultures and species-level identification are strongly recommended to enhance growth detection and determine the clinical relevance of isolates. Treatment for NTM lung diseases consists of a multidrug regimen and a long course of therapy, lasting more than 12 months after negative sputum conversion. For MAC lung disease, several new macrolide-based regimens are now recommended. For nodular bronchiectatic forms of MAC lung diseases, an intermittent three-time-weekly regimen produces outcomes similar to those of daily therapy. Treatment of MABC lung disease is very difficult, requiring long-term use of parenteral agents in combination with new macrolides. Treatment outcomes are much better for M. massiliense lung disease than for M. abscessus lung disease. Thus, precise identification of species in MABC infection is needed for the prediction of antibiotic response. Likewise, increased efforts to improve treatment outcomes and develop new agents for NTM lung disease are needed.
Keyword
MeSH Terms
Figure
Cited by 8 articles
-
Changing Epidemiology of Nontuberculous Mycobacterial Lung Diseases in a Tertiary Referral Hospital in Korea between 2001 and 2015
Ryoung-Eun Ko, Seong Mi Moon, Soohyun Ahn, Byung Woo Jhun, Kyeongman Jeon, O Jung Kwon, Hee Jae Huh, Chang-Seok Ki, Nam Yong Lee, Won-Jung Koh
J Korean Med Sci. 2018;33(8):. doi: 10.3346/jkms.2018.33.e65.Prevalence and Species Spectrum of Pulmonary Nontuberculous Mycobacteria Isolates at a Tertiary Care Center
Young Sun Joo, Na Eun Kwak, Gun Han Kim, Eun-Jeong Yoon, Seok Hoon Jeong
Ann Clin Microbiol. 2019;22(3):71-76. doi: 10.5145/ACM.2019.22.3.71.Diagnosis of pulmonary tuberculosis
Byung Woo Jhun, Hee Jae Huh, Won-Jung Koh
J Korean Med Assoc. 2019;62(1):18-24. doi: 10.5124/jkma.2019.62.1.18.Treatment of
Mycobacterium avium Complex Pulmonary Disease
Yong-Soo Kwon, Won-Jung Koh, Charles L. Daley
Tuberc Respir Dis. 2019;82(1):15-26. doi: 10.4046/trd.2018.0060.Infection Source and Epidemiology of Nontuberculous Mycobacterial Lung Disease
Doosoo Jeon
Tuberc Respir Dis. 2019;82(2):94-101. doi: 10.4046/trd.2018.0026.Treatment Outcomes after Discontinuation of Ethambutol due to Adverse Events in
Mycobacterium avium Complex Lung Disease
Yong Shik Kwon, Byoung Soo Kwon, Ock-hwa Kim, Yea Eun Park, Tae Sun Shim, Yong Pil Chong, Kyung-Wook Jo
J Korean Med Sci. 2020;35(9):. doi: 10.3346/jkms.2020.35.e59.Evaluation of EZplex MTBC/NTM Real-Time PCR kit: diagnostic accuracy and efficacy in vaccination
Suengmok Lee, Kyung-A Hwang, Ji-Hoon Ahn, Jae-Hwan Nam
Clin Exp Vaccine Res. 2018;7(2):111-118. doi: 10.7774/cevr.2018.7.2.111.Neutrophil-Lymphocyte Ratio and Monocyte-Lymphocyte Ratio According to the Radiologic Severity of
Mycobacterium avium Complex Pulmonary Disease
Mi-Ae Kim, Yea Eun Park, Yong Pil Chong, Tae Sun Shim, Kyung-Wook Jo
J Korean Med Sci. 2022;37(40):e292. doi: 10.3346/jkms.2022.37.e292.
Reference
-
1. Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, Holland SM, Horsburgh R, Huitt G, Iademarco MF, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007; 175:367–416.2. Falkinham JO 3rd. Environmental sources of nontuberculous mycobacteria. Clin Chest Med. 2015; 36:35–41.3. Szymanski EP, Leung JM, Fowler CJ, Haney C, Hsu AP, Chen F, Duggal P, Oler AJ, McCormack R, Podack E, et al. Pulmonary nontuberculous mycobacterial infection. A multisystem, multigenic disease. Am J Respir Crit Care Med. 2015; 192:618–628.4. Adjemian J, Olivier KN, Seitz AE, Falkinham JO 3rd, Holland SM, Prevots DR. Spatial clusters of nontuberculous mycobacterial lung disease in the United States. Am J Respir Crit Care Med. 2012; 186:553–558.5. Prevots DR, Marras TK. Epidemiology of human pulmonary infection with nontuberculous mycobacteria: a review. Clin Chest Med. 2015; 36:13–34.6. Kim SJ, Hong YP, Kim SC, Bai GH, Jin BW, Park CD. A case of pulmonary disease due to Mycobacterium avium-intracellulare complex. Tuberc Respir Dis (Seoul). 1981; 28:121–124.7. Koh WJ, Kwon OJ, Lee KS. Diagnosis and treatment of nontuberculous mycobacterial pulmonary diseases: a Korean perspective. J Korean Med Sci. 2005; 20:913–925.8. Adjemian J, Olivier KN, Seitz AE, Holland SM, Prevots DR. Prevalence of nontuberculous mycobacterial lung disease in U.S. Medicare beneficiaries. Am J Respir Crit Care Med. 2012; 185:881–886.9. Marras TK, Mendelson D, Marchand-Austin A, May K, Jamieson FB. Pulmonary nontuberculous mycobacterial disease, Ontario, Canada, 1998-2010. Emerg Infect Dis. 2013; 19:1889–1891.10. Moore JE, Kruijshaar ME, Ormerod LP, Drobniewski F, Abubakar I. Increasing reports of non-tuberculous mycobacteria in England, Wales and Northern Ireland, 1995-2006. BMC Public Health. 2010; 10:612.11. Ide S, Nakamura S, Yamamoto Y, Kohno Y, Fukuda Y, Ikeda H, Sasaki E, Yanagihara K, Higashiyama Y, Hashiguchi K, et al. Epidemiology and clinical features of pulmonary nontuberculous mycobacteriosis in Nagasaki, Japan. PLoS One. 2015; 10:e0128304.12. Chien JY, Lai CC, Sheng WH, Yu CJ, Hsueh PR. Pulmonary infection and colonization with nontuberculous mycobacteria, Taiwan, 2000-2012. Emerg Infect Dis. 2014; 20:1382–1385.13. Park YS, Lee CH, Lee SM, Yang SC, Yoo CG, Kim YW, Han SK, Shim YS, Yim JJ. Rapid increase of non-tuberculous mycobacterial lung diseases at a tertiary referral hospital in South Korea. Int J Tuberc Lung Dis. 2010; 14:1069–1071.14. Lee SK, Lee EJ, Kim SK, Chang J, Jeong SH, Kang YA. Changing epidemiology of nontuberculous mycobacterial lung disease in South Korea. Scand J Infect Dis. 2012; 44:733–738.15. Yoo JW, Jo KW, Kim MN, Lee SD, Kim WS, Kim DS, Shim TS. Increasing trend of isolation of non-tuberculous mycobacteria in a tertiary university hospital in South Korea. Tuberc Respir Dis (Seoul). 2012; 72:409–415.16. Koh WJ, Chang B, Jeong BH, Jeon K, Kim SY, Lee NY, Ki CS, Kwon OJ. Increasing recovery of nontuberculous mycobacteria from respiratory specimens over a 10-year period in a tertiary referral hospital in South Korea. Tuberc Respir Dis (Seoul). 2013; 75:199–204.17. Kim JK, Rheem I. Identification and distribution of nontuberculous mycobacteria from 2005 to 2011 in Cheonan, Korea. Tuberc Respir Dis (Seoul). 2013; 74:215–221.18. Hoefsloot W, van Ingen J, Andrejak C, Angeby K, Bauriaud R, Bemer P, Beylis N, Boeree MJ, Cacho J, Chihota V, et al. The geographic diversity of nontuberculous mycobacteria isolated from pulmonary samples: an NTM-NET collaborative study. Eur Respir J. 2013; 42:1604–1613.19. Koh WJ, Kwon OJ, Jeon K, Kim TS, Lee KS, Park YK, Bai GH. Clinical significance of nontuberculous mycobacteria isolated from respiratory specimens in Korea. Chest. 2006; 129:341–348.20. Jang MA, Koh WJ, Huh HJ, Kim SY, Jeon K, Ki CS, Lee NY. Distribution of nontuberculous mycobacteria by multigene sequence-based typing and clinical significance of isolated strains. J Clin Microbiol. 2014; 52:1207–1212.21. Koh WJ, Jeong BH, Jeon K, Lee NY, Lee KS, Woo SY, Shin SJ, Kwon OJ. Clinical significance of the differentiation between Mycobacterium avium and Mycobacterium intracellulare in M avium complex lung disease. Chest. 2012; 142:1482–1488.22. Boyle DP, Zembower TR, Reddy S, Qi C. Comparison of clinical features, virulence, and relapse among Mycobacterium avium complex species. Am J Respir Crit Care Med. 2015; 191:1310–1317.23. Kim HY, Kook Y, Yun YJ, Park CG, Lee NY, Shim TS, Kim BJ, Kook YH. Proportions of Mycobacterium massiliense and Mycobacterium bolletii strains among Korean Mycobacterium chelonae-Mycobacterium abscessus group isolates. J Clin Microbiol. 2008; 46:3384–3390.24. Koh WJ, Jeon K, Lee NY, Kim BJ, Kook YH, Lee SH, Park YK, Kim CK, Shin SJ, Huitt GA, et al. Clinical significance of differentiation of Mycobacterium massiliense from Mycobacterium abscessus . Am J Respir Crit Care Med. 2011; 183:405–410.25. Lee SH, Yoo HK, Kim SH, Koh WJ, Kim CK, Park YK, Kim HJ. The drug resistance profile of Mycobacterium abscessus group strains from Korea. Ann Lab Med. 2014; 34:31–37.26. Kim SY, Kim CK, Bae IK, Jeong SH, Yim JJ, Jung JY, Park MS, Kim YS, Kim SK, Chang J, et al. The drug susceptibility profile and inducible resistance to macrolides of Mycobacterium abscessus and Mycobacterium massiliense in Korea. Diagn Microbiol Infect Dis. 2015; 81:107–111.27. Yim JJ, Park YK, Lew WJ, Bai GH, Han SK, Shim YS. Mycobacterium kansasii pulmonary diseases in Korea. J Korean Med Sci. 2005; 20:957–960.28. Park HK, Koh WJ, Shim TS, Kwon OJ. Clinical characteristics and treatment outcomes of Mycobacterium kansasii lung disease in Korea. Yonsei Med J. 2010; 51:552–556.29. Moon SM, Park HY, Jeon K, Kim SY, Chung MJ, Huh HJ, Ki CS, Lee NY, Shin SJ, Koh WJ. Clinical significance of Mycobacterium kansasii isolates from respiratory specimens. PLoS One. 2015; 10:e0139621.30. Feazel LM, Baumgartner LK, Peterson KL, Frank DN, Harris JK, Pace NR. Opportunistic pathogens enriched in showerhead biofilms. Proc Natl Acad Sci USA. 2009; 106:16393–16399.31. Adjemian J, Olivier KN, Prevots DR. Nontuberculous mycobacteria among patients with cystic fibrosis in the United States: screening practices and environmental risk. Am J Respir Crit Care Med. 2014; 190:581–586.32. Henkle E, Winthrop KL. Nontuberculous mycobacteria infections in immunosuppressed hosts. Clin Chest Med. 2015; 36:91–99.33. Park SW, Song JW, Shim TS, Park MS, Lee HL, Uh ST, Park CS, Kim DS. Mycobacterial pulmonary infections in patients with idiopathic pulmonary fibrosis. J Korean Med Sci. 2012; 27:896–900.34. Winthrop KL, Baxter R, Liu L, Varley CD, Curtis JR, Baddley JW, McFarland B, Austin D, Radcliffe L, Suhler E, et al. Mycobacterial diseases and antitumour necrosis factor therapy in USA. Ann Rheum Dis. 2013; 72:37–42.35. Brode SK, Jamieson FB, Ng R, Campitelli MA, Kwong JC, Paterson JM, Li P, Marchand-Austin A, Bombardier C, Marras TK. Increased risk of mycobacterial infections associated with anti-rheumatic medications. Thorax. 2015; 70:677–682.36. Lee SK, Kim SY, Kim EY, Jung JY, Park MS, Kim YS, Kim SK, Chang J, Kang YA. Mycobacterial infections in patients treated with tumor necrosis factor antagonists in South Korea. Lung. 2013; 191:565–571.37. Yoo JW, Jo KW, Kang BH, Kim MY, Yoo B, Lee CK, Kim YG, Yang SK, Byeon JS, Kim KJ, et al. Mycobacterial diseases developed during anti-tumour necrosis factor-alpha therapy. Eur Respir J. 2014; 44:1289–1295.38. Park YK, Park YS, Na KI, Cho EH, Shin SS, Kim HJ. Increased tuberculosis burden due to demographic transition in Korea from 2001 to 2010. Tuberc Respir Dis (Seoul). 2013; 74:104–110.39. Kwon YS, Kim YH, Song JU, Jeon K, Song J, Ryu YJ, Choi JC, Kim HC, Koh WJ. Risk factors for death during pulmonary tuberculosis treatment in Korea: a multicenter retrospective cohort study. J Korean Med Sci. 2014; 29:1226–1231.40. Kim JH, Yim JJ. Achievements in and challenges of tuberculosis control in South Korea. Emerg Infect Dis. 2015; 21:1913–1920.41. Kwon YS, Koh WJ. Diagnosis of pulmonary tuberculosis and nontuberculous mycobacterial lung disease in Korea. Tuberc Respir Dis (Seoul). 2014; 77:1–5.42. Koh WJ, Yu CM, Suh GY, Chung MP, Kim H, Kwon OJ, Lee NY, Chung MJ, Lee KS. Pulmonary TB and NTM lung disease: comparison of characteristics in patients with AFB smear-positive sputum. Int J Tuberc Lung Dis. 2006; 10:1001–1007.43. Kim YK, Hahn S, Uh Y, Im DJ, Lim YL, Choi HK, Kim HY. Comparable characteristics of tuberculous and non-tuberculous mycobacterial cavitary lung diseases. Int J Tuberc Lung Dis. 2014; 18:725–729.44. Jeong YJ, Lee KS, Koh WJ, Han J, Kim TS, Kwon OJ. Nontuberculous mycobacterial pulmonary infection in immunocompetent patients: comparison of thin-section CT and histopathologic findings. Radiology. 2004; 231:880–886.45. Chung MJ, Lee KS, Koh WJ, Lee JH, Kim TS, Kwon OJ, Kim S. Thin-section CT findings of nontuberculous mycobacterial pulmonary diseases: comparison between Mycobacterium avium-intracellulare complex and Mycobacterium abscessus infection. J Korean Med Sci. 2005; 20:777–783.46. Lee G, Lee KS, Moon JW, Koh WJ, Jeong BH, Jeong YJ, Kim HJ, Woo S. Nodular bronchiectatic Mycobacterium avium complex pulmonary disease. Natural course on serial computed tomographic scans. Ann Am Thorac Soc. 2013; 10:299–306.47. Lee G, Kim HS, Lee KS, Koh WJ, Jeon K, Jeong BH, Ahn J. Serial CT findings of nodular bronchiectatic Mycobacterium avium complex pulmonary disease with antibiotic treatment. AJR Am J Roentgenol. 2013; 201:764–772.48. Koh WJ, Lee KS, Kwon OJ, Jeong YJ, Kwak SH, Kim TS. Bilateral bronchiectasis and bronchiolitis at thin-section CT: diagnostic implications in nontuberculous mycobacterial pulmonary infection. Radiology. 2005; 235:282–288.49. Park HY, Suh GY, Chung MP, Kim H, Kwon OJ, Chung MJ, Kim TS, Lee KS, Koh WJ. Comparison of clinical and radiographic characteristics between nodular bronchiectatic form of nontuberculous mycobacterial lung disease and diffuse panbronchiolitis. J Korean Med Sci. 2009; 24:427–432.50. Kim RD, Greenberg DE, Ehrmantraut ME, Guide SV, Ding L, Shea Y, Brown MR, Chernick M, Steagall WK, Glasgow CG, et al. Pulmonary nontuberculous mycobacterial disease: prospective study of a distinct preexisting syndrome. Am J Respir Crit Care Med. 2008; 178:1066–1074.51. Kartalija M, Ovrutsky AR, Bryan CL, Pott GB, Fantuzzi G, Thomas J, Strand MJ, Bai X, Ramamoorthy P, Rothman MS, et al. Patients with nontuberculous mycobacterial lung disease exhibit unique body and immune phenotypes. Am J Respir Crit Care Med. 2013; 187:197–205.52. Lee AR, Lee J, Choi SM, Seong MW, Kim SA, Kim M, Chae KO, Lee JS, Yim JJ. Phenotypic, immunologic, and clinical characteristics of patients with nontuberculous mycobacterial lung disease in Korea. BMC Infect Dis. 2013; 13:558.53. Marras TK, Wallace RJ Jr, Koth LL, Stulbarg MS, Cowl CT, Daley CL. Hypersensitivity pneumonitis reaction to Mycobacterium avium in household water. Chest. 2005; 127:664–671.54. Hanak V, Kalra S, Aksamit TR, Hartman TE, Tazelaar HD, Ryu JH. Hot tub lung: presenting features and clinical course of 21 patients. Respir Med. 2006; 100:610–615.55. Hahm CR, Park HY, Jeon K, Um SW, Suh GY, Chung MP, Kim H, Kwon OJ, Koh WJ. Solitary pulmonary nodules caused by Mycobacterium tuberculosis and Mycobacterium avium complex. Lung. 2010; 188:25–31.56. Lim J, Lyu J, Choi CM, Oh YM, Lee SD, Kim WS, Kim DS, Lee H, Shim TS. Non-tuberculous mycobacterial diseases presenting as solitary pulmonary nodules. Int J Tuberc Lung Dis. 2010; 14:1635–1640.57. Jeon K, Koh WJ, Kwon OJ, Suh GY, Chung MP, Kim H, Lee NY, Park YK, Bai GH. Recovery rate of NTM from AFB smear-positive sputum specimens at a medical centre in South Korea. Int J Tuberc Lung Dis. 2005; 9:1046–1051.58. Kim JH, Kim YJ, Ki CS, Kim JY, Lee NY. Evaluation of Cobas TaqMan MTB PCR for detection of Mycobacterium tuberculosis . J Clin Microbiol. 2011; 49:173–176.59. Park KS, Kim JY, Lee JW, Hwang YY, Jeon K, Koh WJ, Ki CS, Lee NY. Comparison of the Xpert MTB/RIF and Cobas TaqMan MTB assays for detection of Mycobacterium tuberculosis in respiratory specimens. J Clin Microbiol. 2013; 51:3225–3227.60. Huh HJ, Koh WJ, Song DJ, Ki CS, Lee NY. Evaluation of the Cobas TaqMan MTB test for the detection of Mycobacterium tuberculosis complex according to acid-fast-bacillus smear grades in respiratory specimens. J Clin Microbiol. 2015; 53:696–698.61. Wang HY, Bang H, Kim S, Koh WJ, Lee H. Identification of Mycobacterium species in direct respiratory specimens using reverse blot hybridisation assay. Int J Tuberc Lung Dis. 2014; 18:1114–1120.62. Huh HJ, Kwon HJ, Ki CS, Lee NY. Comparison of the genedia MTB detection kit and the cobas TaqMan MTB assay for detection of Mycobacterium tuberculosis in respiratory specimens. J Clin Microbiol. 2015; 53:1012–1014.63. Lee BH, Yoon SH, Yeo HJ, Kim DW, Lee SE, Cho WH, Lee SJ, Kim YS, Jeon D. Impact of implementation of an automated liquid culture system on diagnosis of tuberculous pleurisy. J Korean Med Sci. 2015; 30:871–875.64. van Ingen J. Microbiological diagnosis of nontuberculous mycobacterial pulmonary disease. Clin Chest Med. 2015; 36:43–54.65. Griffith DE, Adjemian J, Brown-Elliott BA, Philley JV, Prevots DR, Gaston C, Olivier KN, Wallace RJ Jr. Semiquantitative culture analysis during therapy for Mycobacterium avium complex lung disease. Am J Respir Crit Care Med. 2015; 192:754–760.66. Koh WJ, Stout JE, Yew WW. Advances in the management of pulmonary disease due to Mycobacterium abscessus complex. Int J Tuberc Lung Dis. 2014; 18:1141–1148.67. Jeon K, Kwon OJ, Lee NY, Kim BJ, Kook YH, Lee SH, Park YK, Kim CK, Koh WJ. Antibiotic treatment of Mycobacterium abscessus lung disease: a retrospective analysis of 65 patients. Am J Respir Crit Care Med. 2009; 180:896–902.68. van Ingen J, Boeree MJ, van Soolingen D, Mouton JW. Resistance mechanisms and drug susceptibility testing of nontuberculous mycobacteria. Drug Resist Updat. 2012; 15:149–161.69. Bastian S, Veziris N, Roux AL, Brossier F, Gaillard JL, Jarlier V, Cambau E. Assessment of clarithromycin susceptibility in strains belonging to the Mycobacterium abscessus group by erm(41) and rrl sequencing. Antimicrob Agents Chemother. 2011; 55:775–781.70. Choi GE, Shin SJ, Won CJ, Min KN, Oh T, Hahn MY, Lee K, Lee SH, Daley CL, Kim S, et al. Macrolide treatment for Mycobacterium abscessus and Mycobacterium massiliense infection and inducible resistance. Am J Respir Crit Care Med. 2012; 186:917–925.71. Brown-Elliott BA, Vasireddy S, Vasireddy R, Iakhiaeva E, Howard ST, Nash K, Parodi N, Strong A, Gee M, Smith T, et al. Utility of sequencing the erm(41) gene in isolates of Mycobacterium abscessus subsp. abscessus with low and intermediate clarithromycin MICs. J Clin Microbiol. 2015; 53:1211–1215.72. Ito Y, Hirai T, Maekawa K, Fujita K, Imai S, Tatsumi S, Handa T, Matsumoto H, Muro S, Niimi A, et al. Predictors of 5-year mortality in pulmonary Mycobacterium avium-intracellulare complex disease. Int J Tuberc Lung Dis. 2012; 16:408–414.73. Hayashi M, Takayanagi N, Kanauchi T, Miyahara Y, Yanagisawa T, Sugita Y. Prognostic factors of 634 HIV-negative patients with Mycobacterium avium complex lung disease. Am J Respir Crit Care Med. 2012; 185:575–583.74. Kikuchi T, Kobashi Y, Hirano T, Tode N, Santoso A, Tamada T, Fujimura S, Mitsuhashi Y, Honda Y, Nukiwa T, et al. Mycobacterium avium genotype is associated with the therapeutic response to lung infection. Clin Microbiol Infect. 2014; 20:256–262.75. Shin SJ, Choi GE, Cho SN, Woo SY, Jeong BH, Jeon K, Koh WJ. Mycobacterial genotypes are associated with clinical manifestation and progression of lung disease caused by Mycobacterium abscessus and Mycobacterium massiliense . Clin Infect Dis. 2013; 57:32–39.76. Wallace RJ Jr, Brown-Elliott BA, McNulty S, Philley JV, Killingley J, Wilson RW, York DS, Shepherd S, Griffith DE. Macrolide/Azalide therapy for nodular/bronchiectatic Mycobacterium avium complex lung disease. Chest. 2014; 146:276–282.77. Jeong BH, Jeon K, Park HY, Kim SY, Lee KS, Huh HJ, Ki CS, Lee NY, Shin SJ, Daley CL, et al. Intermittent antibiotic therapy for nodular bronchiectatic Mycobacterium avium complex lung disease. Am J Respir Crit Care Med. 2015; 191:96–103.78. Field SK, Fisher D, Cowie RL. Mycobacterium avium complex pulmonary disease in patients without HIV infection. Chest. 2004; 126:566–581.79. Xu HB, Jiang RH, Li L. Treatment outcomes for Mycobacterium avium complex: a systematic review and meta-analysis. Eur J Clin Microbiol Infect Dis. 2014; 33:347–358.80. Lee BY, Kim S, Hong Y, Lee SD, Kim WS, Kim DS, Shim TS, Jo KW. Risk factors for recurrence after successful treatment of Mycobacterium avium complex lung disease. Antimicrob Agents Chemother. 2015; 59:2972–2977.81. Min J, Park J, Lee YJ, Kim SJ, Park JS, Cho YJ, Yoon HI, Lee CT, Lee JH. Determinants of recurrence after successful treatment of Mycobacterium avium complex lung disease. Int J Tuberc Lung Dis. 2015; 19:1239–1245.82. van Ingen J, Egelund EF, Levin A, Totten SE, Boeree MJ, Mouton JW, Aarnoutse RE, Heifets LB, Peloquin CA, Daley CL. The pharmacokinetics and pharmacodynamics of pulmonary Mycobacterium avium complex disease treatment. Am J Respir Crit Care Med. 2012; 186:559–565.83. Koh WJ, Jeong BH, Jeon K, Lee SY, Shin SJ. Therapeutic drug monitoring in the treatment of Mycobacterium avium complex lung disease. Am J Respir Crit Care Med. 2012; 186:797–802.84. Adjemian J, Prevots DR, Gallagher J, Heap K, Gupta R, Griffith D. Lack of adherence to evidence-based treatment guidelines for nontuberculous mycobacterial lung disease. Ann Am Thorac Soc. 2014; 11:9–16.85. Griffith DE, Brown-Elliott BA, Langsjoen B, Zhang Y, Pan X, Girard W, Nelson K, Caccitolo J, Alvarez J, Shepherd S, et al. Clinical and molecular analysis of macrolide resistance in Mycobacterium avium complex lung disease. Am J Respir Crit Care Med. 2006; 174:928–934.86. Jo KW, Kim S, Lee JY, Lee SD, Kim WS, Kim DS, Shim TS. Treatment outcomes of refractory MAC pulmonary disease treated with drugs with unclear efficacy. J Infect Chemother. 2014; 20:602–606.87. Jarand J, Davis JP, Cowie RL, Field SK, Fisher DA. Long term follow up of Mycobacterium avium complex lung disease in patients treated with regimens including clofazimine and/or fifampin. Chest. Forthcoming. 2015.88. Koh WJ, Hong G, Kim SY, Jeong BH, Park HY, Jeon K, Kwon OJ, Lee SH, Kim CK, Shin SJ. Treatment of refractory Mycobacterium avium complex lung disease with a moxifloxacin-containing regimen. Antimicrob Agents Chemother. 2013; 57:2281–2285.89. Lyu J, Jang HJ, Song JW, Choi CM, Oh YM, Lee SD, Kim WS, Kim DS, Shim TS. Outcomes in patients with Mycobacterium abscessus pulmonary disease treated with long-term injectable drugs. Respir Med. 2011; 105:781–787.90. Jarand J, Levin A, Zhang L, Huitt G, Mitchell JD, Daley CL. Clinical and microbiologic outcomes in patients receiving treatment for Mycobacterium abscessus pulmonary disease. Clin Infect Dis. 2011; 52:565–571.91. Lyu J, Kim BJ, Kim BJ, Song JW, Choi CM, Oh YM, Lee SD, Kim WS, Kim DS, Shim TS. A shorter treatment duration may be sufficient for patients with Mycobacterium massiliense lung disease than with Mycobacterium abscessus lung disease. Respir Med. 2014; 108:1706–1712.92. Cho YJ, Yi H, Chun J, Cho SN, Daley CL, Koh WJ, Shin SJ. The genome sequence of ‘Mycobacterium massiliense’ strain CIP 108297 suggests the independent taxonomic status of the Mycobacterium abscessus complex at the subspecies level. PLoS One. 2013; 8:e81560.93. Griffith DE, Brown-Elliott BA, Benwill JL, Wallace RJ Jr. Mycobacterium abscessus. "Pleased to meet you, hope you guess my name... Ann Am Thorac Soc. 2015; 12:436–439.94. Kim HS, Lee KS, Koh WJ, Jeon K, Lee EJ, Kang H, Ahn J. Serial CT findings of Mycobacterium massiliense pulmonary disease compared with Mycobacterium abscessus disease after treatment with antibiotic therapy. Radiology. 2012; 263:260–270.95. Harada T, Akiyama Y, Kurashima A, Nagai H, Tsuyuguchi K, Fujii T, Yano S, Shigeto E, Kuraoka T, Kajiki A, et al. Clinical and microbiological differences between Mycobacterium abscessus and Mycobacterium massiliense lung diseases. J Clin Microbiol. 2012; 50:3556–3561.96. Kang HK, Park HY, Kim D, Jeong BH, Jeon K, Cho JH, Kim HK, Choi YS, Kim J, Koh WJ. Treatment outcomes of adjuvant resectional surgery for nontuberculous mycobacterial lung disease. BMC Infect Dis. 2015; 15:76.97. Olivier KN, Shaw PA, Glaser TS, Bhattacharyya D, Fleshner M, Brewer CC, Zalewski CK, Folio LR, Siegelman JR, Shallom S, et al. Inhaled amikacin for treatment of refractory pulmonary nontuberculous mycobacterial disease. Ann Am Thorac Soc. 2014; 11:30–35.98. Rose SJ, Neville ME, Gupta R, Bermudez LE. Delivery of aerosolized liposomal amikacin as a novel approach for the treatment of nontuberculous mycobacteria in an experimental model of pulmonary infection. PLoS One. 2014; 9:e108703.99. Philley JV, Wallace RJ Jr, Benwill JL, Taskar V, Brown-Elliott BA, Thakkar F, Aksamit TR, Griffith DE. Preliminary results of bedaquiline as salvage therapy for patients with nontuberculous mycobacterial lung disease. Chest. 2015; 148:499–506.100. Philley JV, Griffith DE. Treatment of slowly growing mycobacteria. Clin Chest Med. 2015; 36:79–90.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnosis of Pulmonary Tuberculosis and Nontuberculous Mycobacterial Lung Disease in Korea
- Nontuberculous Mycobacterial Lung Disease
- Respiratory Review of 2009: Nontuberculous Mycobacterium
- Radiologic Diagnosis of Nontuberculous Mycobacterial Pulmonary Disease
- Diagnosis and Treatment of Nontuberculous Mycobacterial Lung Disease: Clinicians' Perspectives