Korean J Gastroenterol.
2015 Nov;66(5):282-285. 10.4166/kjg.2015.66.5.282.
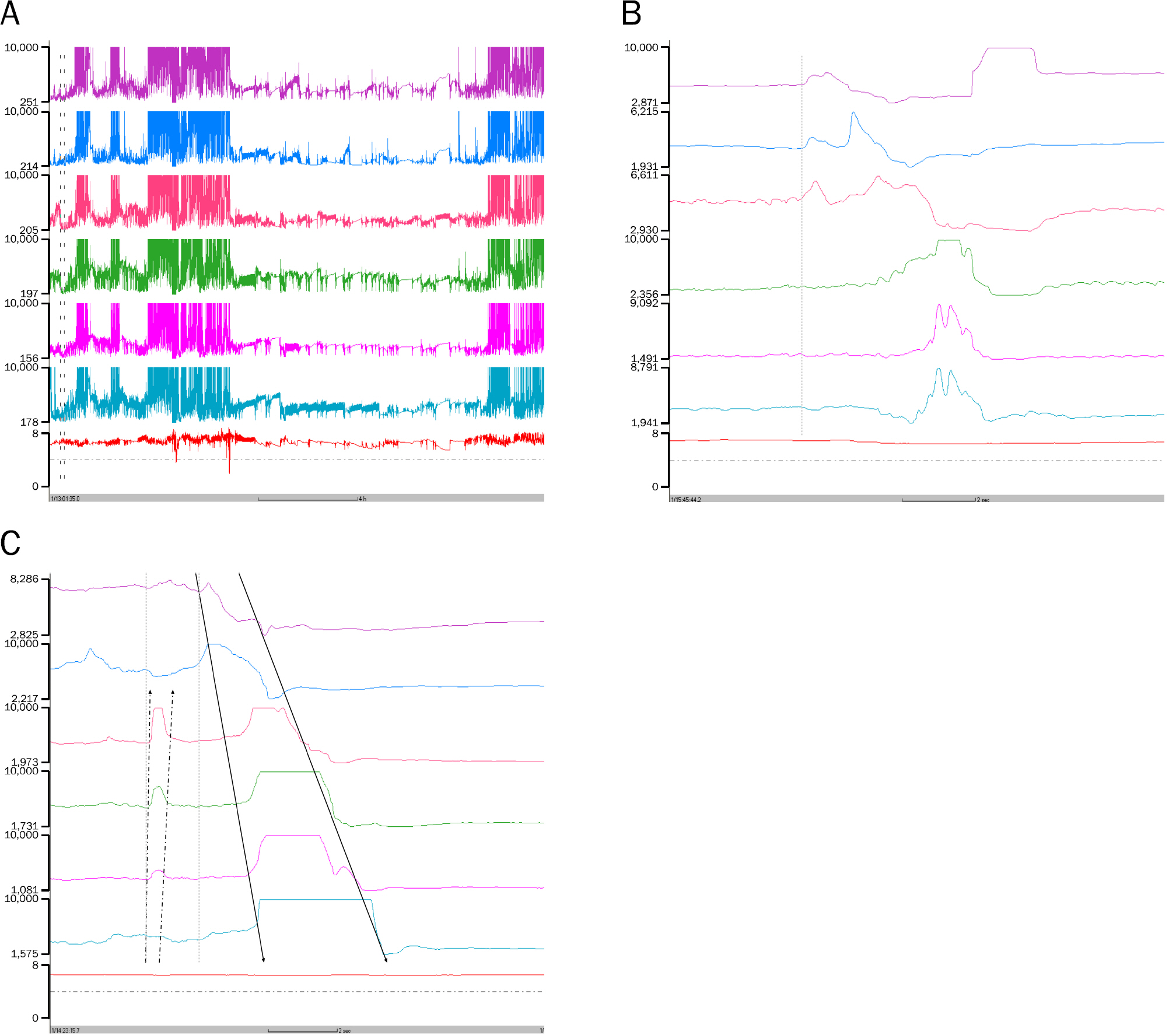
A Case of Aerophagia Diagnosed by Multichannel Intraluminal Impedance Monitoring
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Digestive Disease Research Institute, Wonkwang University College of Medicine, Iksan, Korea. hanseung@wonkwang.ac.kr
- KMID: 2373358
- DOI: http://doi.org/10.4166/kjg.2015.66.5.282
Abstract
- Aerophagia is a disorder caused by abnormal accumulation of air in the gastrointestinal tract as a result of repetitive and frequent inflow of air through the mouth. For the diagnosis of this condition, it is difficult to objectively measure the air swallowing. However, multichannel intraluminal impedance monitoring facilitates the differential diagnosis between normal air swallowing and pathologic aerophagia, and can aid in the determination of the frequency and amount of air swallowed. In this report, in addition to a literature review, we describe a case of 36-year-old man with abdominal distension who was diagnosed with aerophagia using esophageal impedance monitoring and was treated with clonazepam.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Hemmink GJ, Weusten BL, Bredenoord AJ, Timmer R, Smout AJ. Aerophagia: excessive air swallowing demonstrated by esophageal impedance monitoring. Clin Gastroenterol Hepatol. 2009; 7:1127–1129.
Article2. Smith SW. Aerophagy. Br Med J. 1940; 1:296–297.
Article3. Tack J, Talley NJ, Camilleri M, et al. Functional gastroduodenal disorders. Gastroenterology. 2006; 130:1466–1479.
Article4. Lekkas CN, Lentino W. Symptom-producing interposition of the colon. Clinical syndrome in mentally deficient adults. JAMA. 1978; 240:747–750.
Article5. Bredenoord AJ. Management of belching, hiccups, and aerophagia. Clin Gastroenterol Hepatol. 2013; 11:6–12.
Article6. Chitkara DK, Bredenoord AJ, Rucker MJ, Talley NJ. Aerophagia in adults: a comparison with functional dyspepsia. Aliment Pharmacol Ther. 2005; 22:855–858.
Article7. Weil RS, Cavanna AE, Willoughby JM, Robertson MM. Air swallowing as a tic. J Psychosom Res. 2008; 65:497–500.
Article8. Hwang JB, Choi WJ, Kim JS, et al. Clinical features of pathologic childhood aerophagia: early recognition and essential diagnostic criteria. J Pediatr Gastroenterol Nutr. 2005; 41:612–616.
Article9. Komuro H, Matoba K, Kaneko M. Laparoscopic gastropexy for chronic gastric volvulus complicated by pathologic aerophagia in a boy. Pediatr Int. 2005; 47:701–703.
Article10. Basaran UN, Inan M, Aksu B, Ceylan T. Colon perforation due to pathologic aerophagia in an intellectually disabled child. J Paediatr Child Health. 2007; 43:710–712.
Article11. van der Kolk MB, Bender MH, Goris RJ. Acute abdomen in mentally retarded patients: role of aerophagia. Report of nine cases. Eur J Surg. 1999; 165:507–511.12. Pouderoux P, Ergun GA, Lin S, Kahrilas PJ. Esophageal bolus transit imaged by ultrafast computerized tomography. Gastroenterology. 1996; 110:1422–1428.
Article13. Sifrim D, Silny J, Holloway RH, Janssens JJ. Patterns of gas and liquid reflux during transient lower oesophageal sphincter relaxation: a study using intraluminal electrical impedance. Gut. 1999; 44:47–54.
Article14. Imam H, Shay S, Ali A, Baker M. Bolus transit patterns in healthy subjects: a study using simultaneous impedance monitoring, videoesophagram, and esophageal manometry. Am J Physiol Gastrointest Liver Physiol. 2005; 288:G1000–G1006.
Article15. Blondeau K, Boecxstaens V, Rommel N, et al. Baclofen improves symptoms and reduces postprandial flow events in patients with rumination and supragastric belching. Clin Gastroenterol Hepatol. 2012; 10:379–384.
Article16. Lee GH, Jang HJ, Hwang JB. Clonazepam treatment of pathologic aerophagia in children with mental retardation. Pediatr Gastroenterol Hepatol Nutr. 2014; 17:209–213.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Combined Multichannel Intraluminal Impedance and pH Monitoring for Patients With Suspected Laryngopharyngeal Reflux: Is It Ready to Use?
- Simultaneous Evaluation of Laryngopharyngeal Reflux and Swallowing Function Using Hypopharyngeal Multichannel Intraluminal Impedance Measurements in Neurologically Impaired Patients
- Usefulness of Multichannel Intraluminal Impedance-pH Metry in Children with Suspected Gastroesophageal Reflux Disease
- Esophageal pH and Combined Impedance-pH Monitoring in Children
- Usefulness of Multichannel Intraluminal Impedance-pH metry in Patients with Suspected GERD Presenting with Typical or Atypical Symptoms