J Korean Ophthalmol Soc.
2017 Mar;58(3):352-357. 10.3341/jkos.2017.58.3.352.
Central Retinal Vein Occlusion in Young Healthy Patients and the Role of Thrombophilia in Pathogenesis
- Affiliations
-
- 1Department of Ophthalmology, Dankook University Hospital, Dankook University College of Medicine, Cheonan, Korea. persica79@naver.com
- KMID: 2371919
- DOI: http://doi.org/10.3341/jkos.2017.58.3.352
Abstract
- PURPOSE
We report two young patients who developed central retinal vein occlusion (CRVO) without any systemic disease, and various thrombophilia tests were performed to determine the etiology.
CASE SUMMARY
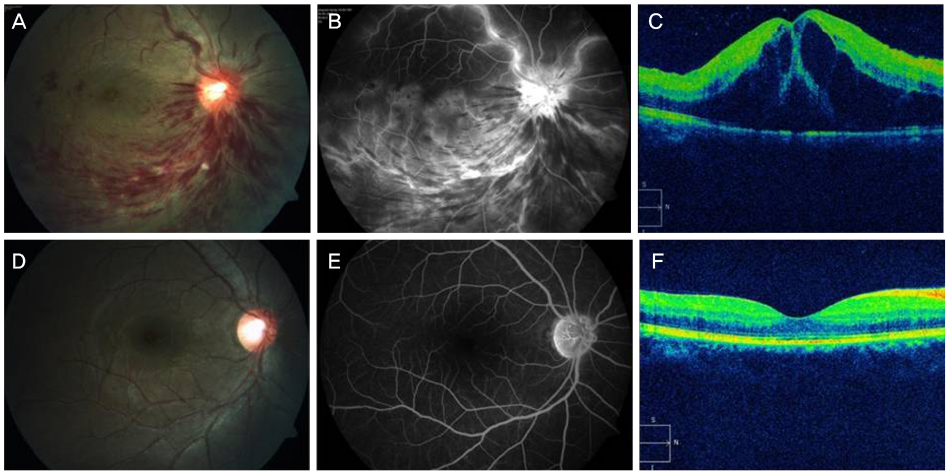
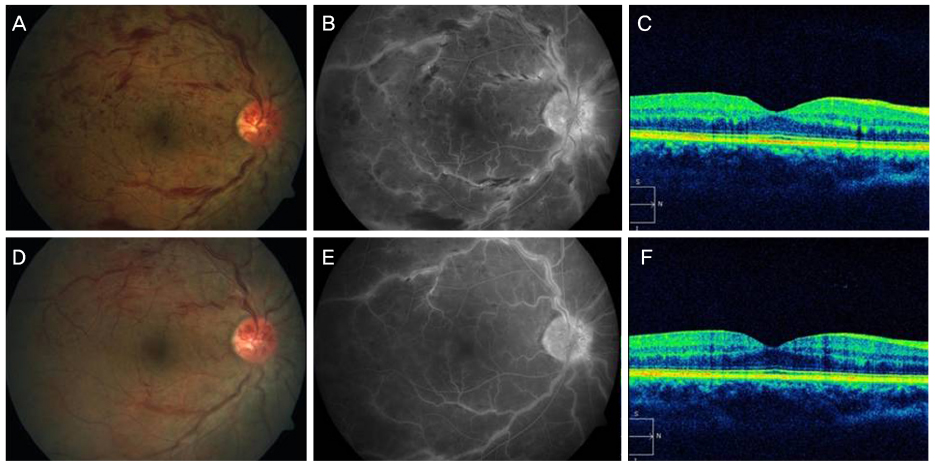
Two young patients, a 22-year-old female and a 23-year-old male, who had acute vision loss were diagnosed with nonischemic CRVO via fluorescein angiography. They had no other disease and no common risk factors for CRVO. We performed various tests to determine the thrombophilic risk factors and discovered a transient decrease in protein S antigen and protein C antigen in the female and male patients, respectively.
CONCLUSIONS
CRVO in young patients without systemic disorders may have different mechanisms in the pathology and thus additional laboratory tests to determine thrombophilic disorders are necessary.
Keyword
MeSH Terms
Figure
Reference
-
1. Green WR, Chan CC, Hutchins GM, Terry JM. Central retinal vein occlusion: a prospective histopathologic study of 29 eyes in 28 cases. Trans Am Ophthalmol Soc. 1981; 79:371–422.2. Hayreh SS. Prevalent misconceptions about acute retinal vascular occlusive disorders. Prog Retin Eye Res. 2005; 24:493–519.3. The Eye Disease Case-Control Study Group. Risk factors for central retinal vein occlusion. Arch Ophthalmol. 1996; 114:545–554.4. Mitchell P, Smith W, Chang A. Prevalence and associations of retinal vein occlusion in Australia. The Blue Mountains Eye Study. Arch Ophthalmol. 1996; 114:1243–1247.5. Rehak M, Krcova V, Slavik L, et al. The role of thrombophilia in patients with retinal vein occlusion and no systemic risk factors. Can J Ophthalmol. 2010; 45:171–175.6. Arsène S, Delahousse B, Regina S, et al. Increased prevalence of factor V Leiden in patients with retinal vein occlusion and under 60 years of age. Thromb Haemost. 2005; 94:101–106.7. Moon SH, Hwang BS, Chang WH. Clinical course of young adults with central retinal vein occlusion. J Korean Ophthalmol Soc. 2008; 49:1948–1953.8. Vrabec JP, Levin LA. Type II protein C deficiency in a 16-year-old girl with central retinal vein occlusion. Am J Ophthalmol. 2007; 143:341–342.9. Kuhli C, Hattenbach LO, Scharrer I, et al. High prevalence of resistance to APC in young patients with retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol. 2002; 240:163–168.10. D'Angelo A, Vigano-D'Angelo S, Esmon CT, Comp PC. Acquired deficiencies of protein S. Protein S activity during oral anticoagulation, in liver disease, and in disseminated intravascular coagulation. J Clin Invest. 1988; 81:1445–1454.11. Kovacs MJ, Kovacs J, Anderson J, et al. Protein C and protein S levels can be accurately determined within 24 hours of diagnosis of acute venous thromboembolism. Clin Lab Haematol. 2006; 28:9–13.12. Moisseiev E, Sagiv O, Lazar M. Intense exercise causing central retinal vein occlusion in a young patient: case report and review of the literature. Case Rep Ophthalmol. 2014; 5:116–120.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Central Retinal Vein Occlusion by Protein C Deficiency
- Hematologic Risk Factors in Young-Aged Retinal Vein Occlusion
- A Case of Cilioretinal Artery Occlusion Associated with Central Retinal Vein Occlusion
- A Case of Papillophlebitis in 21-year-old Healthy Male Adult
- Clinical Analysis of the Hemispheric Retinal Vein Occlusion