Hip Pelvis.
2017 Mar;29(1):68-76. 10.5371/hp.2017.29.1.68.
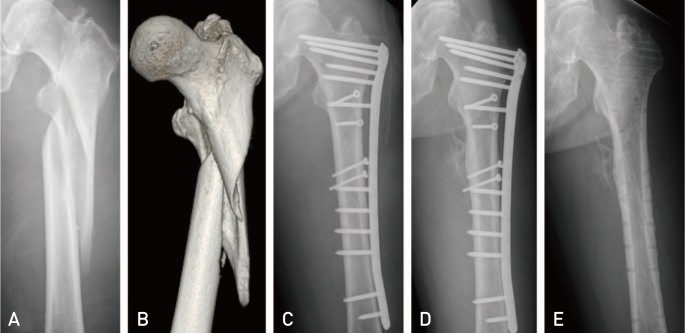
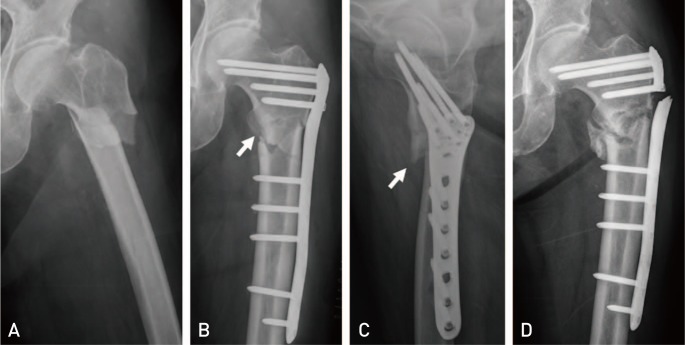
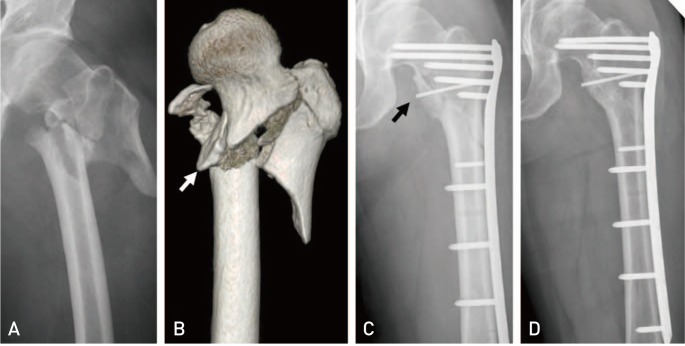
Surgical Outcomes of Biologic Fixation for Subtrochanteric Fracture Using Locking Compression Plates
- Affiliations
-
- 1Department of Orthopaedic Surgery, Biomedical Research Institute, Pusan National University Hospital, Busan, Korea. namhoonmoon@gmail.com
- 2Department of Orthopaedic Surgery, Pusan Korea Hospital, Busan, Korea.
- KMID: 2371770
- DOI: http://doi.org/10.5371/hp.2017.29.1.68
Abstract
- PURPOSE
This study aimed to evaluate the surgical outcomes of biologic plating using locking compression plate-distal femur (LCP-DF) in patients with subtrochanteric fracture of the femur.
MATERIALS AND METHODS
Between January 2010 and December 2013, 28 consecutive patients with subtrochanteric fractures of the femur, treated with biologic fixation using LCP-DF, were enrolled. Preoperative values, including patient age, sex, body mass index, fracture type, type of lung injury, and surgical timing from injury to surgery, were retrospectively evaluated. Radiologic assessments included time to union, coronal alignment, rotational alignment, and complications such as implant breakage and screw breakage. Adverse events, including postoperative fat embolism and adult respiratory distress syndrome, infection during the follow-up period, and walking ability at the last follow-up visit, were assessed.
RESULTS
Union was achieved in 27 patients (96.4%) after a mean duration of 5.4 months (range, 3-14 months). No patients developed fat embolism or adult respiratory distress syndrome during the hospitalization period of this study.
CONCLUSION
Biologic fixation using locking compression plates may represent a safe surgical option which can be utilized in patients with subtrochanteric fracture regardless of injury severity, surgical timing, fracture type, and presence of lung injury.
MeSH Terms
Figure
Cited by 1 articles
-
Characteristics and Surgical Outcomes of Intertrochanteric or Subtrochanteric Fractures Associated with Ipsilateral Femoral Shaft Fractures Treated with Closed Intramedullary Nailing: A Review of 31 Consecutive Cases over Four Years at a Single Institution
Yoon Jae Seong, Jae Hoon Jang, Se Bin Jeon, Nam Hoon Moon
Hip Pelvis. 2019;31(4):190-199. doi: 10.5371/hp.2019.31.4.190.
Reference
-
1. Giannoudis PV, Giannoudi M, Stavlas P. Damage control orthopaedics: lessons learned. Injury. 2009; 40(Suppl 4):S47–S52. PMID: 19895952.
Article2. Roberts CS, Pape HC, Jones AL, Malkani AL, Rodriguez JL, Giannoudis PV. Damage control orthopaedics: evolving concepts in the treatment of patients who have sustained orthopaedic trauma. Instr Course Lect. 2005; 54:447–462. PMID: 15948472.3. Kreder HJ. Principles and evidence: The optimal treatment of pertrochanteric hip fractures: Commentary on an article by Kjell Matre, MD, et al.: “TRIGEN INTERTAN intramedullary nail versus sliding hip screw. A prospective, randomized multicenter study on pain, function, and complications in 684 patients with an intertrochanteric or subtrochanteric fracture and one year of follow-up”. J Bone Joint Surg Am. 2013; 95:e16(1-2). PMID: 23389796.4. Miedel R, Törnkvist H, Ponzer S, Söderqvist A, Tidermark J. Musculoskeletal function and quality of life in elderly patients after a subtrochanteric femoral fracture treated with a cephalomedullary nail. J Orthop Trauma. 2011; 25:208–213. PMID: 21399469.
Article5. Cheng MT, Chiu FY, Chuang TY, Chen CM, Chen TH, Lee PC. Treatment of complex subtrochanteric fracture with the long gamma AP locking nail: a prospective evaluation of 64 cases. J Trauma. 2005; 58:304–311. PMID: 15706192.
Article6. Kregor PJ, Stannard J, Zlowodzki M, Cole PA, Alonso J. Distal femoral fracture fixation utilizing the Less Invasive Stabilization System (LISS): the technique and early results. Injury. 2001; 32(Suppl 3):SC32–SC47. PMID: 11888193.
Article7. Corrales LA, Morshed S, Bhandari M, Miclau T 3rd. Variability in the assessment of fracture-healing in orthopaedic trauma studies. J Bone Joint Surg Am. 2008; 90:1862–1868. PMID: 18762645.
Article8. Waddell JP. Subtrochanteric fractures of the femur: a review of 130 patients. J Trauma. 1979; 19:582–592. PMID: 469971.9. Parker MJ, Dutta BK, Sivaji C, Pryor GA. Subtrochanteric fractures of the femur. Injury. 1997; 28:91–95. PMID: 9205572.
Article10. Fielding JW, Cochran GV, Zickel RE. Biomechanical characteristics and surgical management of subtrochanteric fractures. Orthop Clin North Am. 1974; 5:629–650. PMID: 4600224.
Article11. Seinsheimer F. Subtrochanteric fractures of the femur. J Bone Joint Surg Am. 1978; 60:300–306. PMID: 649632.
Article12. Zickel RE. An intramedullary fixation device for the proximal part of the femur. Nine years' experience. J Bone Joint Surg Am. 1976; 58:866–872. PMID: 956232.
Article13. Johnson KD, Tencer AF, Sherman MC. Biomechanical factors affecting fracture stability and femoral bursting in closed intramedullary nailing of femoral shaft fractures, with illustrative case presentations. J Orthop Trauma. 1987; 1:1–11. PMID: 3506582.
Article14. Kraemer WJ, Hearn TC, Powell JN, Mahomed N. Fixation of segmental subtrochanteric fractures. A biomechanical study. Clin Orthop Relat Res. 1996; (332):71–79.15. Brumback RJ, Toal TR Jr, Murphy-Zane MS, Novak VP, Belkoff SM. Immediate weight-bearing after treatment of a comminuted fracture of the femoral shaft with a statically locked intramedullary nail. J Bone Joint Surg Am. 1999; 81:1538–1544. PMID: 10565645.
Article16. Yoon RS, Donegan DJ, Liporace FA. Reducing subtrochanteric femur fractures: tips and tricks, do's and don'ts. J Orthop Trauma. 2015; 29(Suppl 4):S28–S33.17. Bone LB, Giannoudis P. Femoral shaft fracture fixation and chest injury after polytrauma. J Bone Joint Surg Am. 2011; 93:311–317. PMID: 21266645.
Article18. Bosse MJ, MacKenzie EJ, Riemer BL, et al. Adult respiratory distress syndrome, pneumonia, and mortality following thoracic injury and a femoral fracture treated either with intramedullary nailing with reaming or with a plate. A comparative study. J Bone Joint Surg Am. 1997; 79:799–809. PMID: 9199375.
Article19. Stavlas P, Giannoudis PV. Bilateral femoral fractures: does intramedullary nailing increase systemic complications and mortality rates. Injury. 2009; 40:1125–1128. PMID: 19775688.
Article20. Asher MA, Tippett JW, Rockwood CA, Zilber S. Compression fixation of subtrochanteric fractures. Clin Orthop Relat Res. 1976; (117):202–208.
Article21. Yoo MC, Cho YJ, Kim KI, Khairuddin M, Chun YS. Treatment of unstable peritrochanteric femoral fractures using a 95 degrees angled blade plate. J Orthop Trauma. 2005; 19:687–692. PMID: 16314715.22. Celebi L, Can M, Muratli HH, Yagmurlu MF, Yuksel HY, Bicimoğlu A. Indirect reduction and biological internal fixation of comminuted subtrochanteric fractures of the femur. Injury. 2006; 37:740–750. PMID: 16487528.
Article23. Vaidya SV, Dholakia DB, Chatterjee A. The use of a dynamic condylar screw and biological reduction techniques for subtrochanteric femur fracture. Injury. 2003; 34:123–128. PMID: 12565019.
Article24. Dumbre Patil SS, Karkamkar SS, Patil VS, Patil SS, Ranaware AS. Reverse distal femoral locking compression plate a salvage option in nonunion of proximal femoral fractures. Indian J Orthop. 2016; 50:374–378. PMID: 27512218.25. Oh CW, Kim JJ, Byun YS, et al. Minimally invasive plate osteosynthesis of subtrochanteric femur fractures with a locking plate: a prospective series of 20 fractures. Arch Orthop Trauma Surg. 2009; 129:1659–1665. PMID: 19169695.
Article26. Papanna MC, Al-Hadithy N, Ma CH, Tu YK, Yu SW, Yen CY, Yeh JH, Wu CH. Reverse LISS plates for unstable proximal femoral fractures [Injury 2010;41(8):827-33]. Injury. 2012; 43:392.27. Ma CH, Tu YK, Yu SW, Yen CY, Yeh JH, Wu CH. Reverse LISS plates for unstable proximal femoral fractures. Injury. 2010; 41:827–833. PMID: 20471014.
Article28. Acklin YP, Bereiter H, Sommer C. Reversed LISS-DF in selected cases of complex proximal femur fractures. Injury. 2010; 41:427–429. PMID: 19555949.
Article29. Crist BD, Khalafi A, Hazelwood SJ, Lee MA. A biomechanical comparison of locked plate fixation with percutaneous insertion capability versus the angled blade plate in a subtrochanteric fracture gap model. J Orthop Trauma. 2009; 23:622–627. PMID: 19897982.
Article30. Wieser K, Babst R. Fixation failure of the LCP proximal femoral plate 4.5/5.0 in patients with missing posteromedial support in unstable per-, inter-, and subtrochanteric fractures of the proximal femur. Arch Orthop Trauma Surg. 2010; 130:1281–1287. PMID: 20191276.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Subtrochanteric Fracture Treated with Bent Self - Compression Plate
- Surgical Treatment of Subtrochanteric Fracture with Compression Hip Screw
- Treatment of Femur Supracondylar Fracture with Locking Compression Plate
- Orthogonal Locking Compression Plate Fixation for Distal Humeral Intraarticular Fractures
- External Fixation for Distal Radius Fractures