Ann Hepatobiliary Pancreat Surg.
2017 Feb;21(1):57-60. 10.14701/ahbps.2017.21.1.57.
Biliary metastasis in colorectal cancer confers a poor prognosis: case study of 5 consecutive patients
- Affiliations
-
- 1Division of Colorectal Surgery, University Surgical Cluster, National University Health System, Singapore. surtkk@nus.edu.sg
- 2Department of Surgery, Yong Loo Lin School of Medicine, National University of Singapore, Singapore.
- 3Department of Pathology, Yong Loo Lin School of Medicine, National University of Singapore, Singapore.
- KMID: 2371569
- DOI: http://doi.org/10.14701/ahbps.2017.21.1.57
Abstract
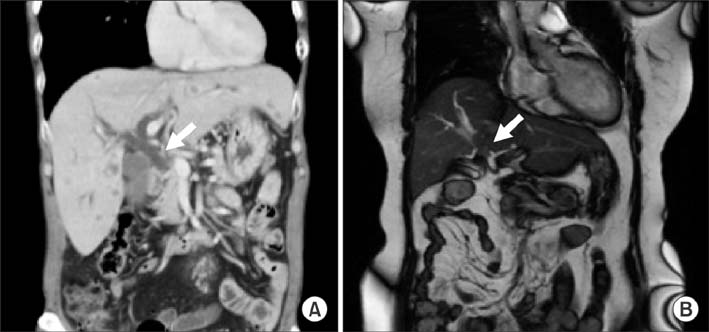
- The biliary duct is an extremely rare site for colon cancer metastasis. It often leads to a diagnostic dilemma, since primary cholangiocarcinoma (potentially treatable with surgery) has a similar presentation. This paper highlights our experience with 5 consecutive patients who had colon malignancy with biliary metastasis, and prognosis of their disease. Five patients, with a history of primary colon cancer since 2010, were identified to have biliary metastasis. Of these, 4 (80.0%) patients were male. The median time to diagnosis of biliary metastasis from diagnosis of colon cancer was 59.2 months (0-70.1 months), and all exhibited symptoms of biliary obstruction or its associated complications. Evaluation of the tumour samples revealed all specimens to be negative for CK7 but positive for CK20, suggestive of a colorectal primary. The median survival of the 5 patients was 23.5 months (1.8-44.5 months) from the diagnosis of biliary metastasis. However, none of their death was related to the direct complication of biliary obstruction. Biliary metastasis is a rare entity for metastatic colon malignancy. Diagnosis may be difficult radiologically, and immunohistochemical staining may help in identification. The overall survival for these patients is dismal.
Keyword
MeSH Terms
Figure
Reference
-
1. Wenzel DJ, Gaede JT, Wenzel LR. Case report. Intrabiliary colonic metastasis mimicking primary biliary neoplasia. AJR Am J Roentgenol. 2003; 180:1029–1032.2. Tirapu de Sagrario MG, Baleato González S, García Figueiras R, Coessens A. Intraductal biliary metastases from colorectal cancer: a report of two cases. Radiologia. 2014; 56:e34–e37.3. Herbut PA, Watson JS. Metastatic cancer of the extrahepatic bile ducts producing jaundice. Am J Clin Pathol. 1946; 16:365–372.4. Kawakatsu S, Kaneoka Y, Maeda A, Takayama Y, Fukami Y, Onoe S. Intrapancreatic bile duct metastasis from colon cancer after resection of liver metastasis with intrabiliary growth: a case report. World J Surg Oncol. 2015; 13:254.5. Sugiura T, Nagino M, Oda K, Ebata T, Nishio H, Arai T, et al. Hepatectomy for colorectal liver metastases with macroscopic intrabiliary tumor growth. World J Surg. 2006; 30:1902–1908.6. Okano K, Yamamoto J, Moriya Y, Akasu T, Kosuge T, Sakamoto M, et al. Macroscopic intrabiliary growth of liver metastases from colorectal cancer. Surgery. 1999; 126:829–834.7. Kubo M, Sakamoto M, Fukushima N, Yachida S, Nakanishi Y, Shimoda T, et al. Less aggressive features of colorectal cancer with liver metastases showing macroscopic intrabiliary extension. Pathol Int. 2002; 52:514–518.8. Seo SI, Lim SB, Yoon YS, Kim CW, Yu CS, Kim TW, et al. Comparison of recurrence patterns between ≤5 years and >5 years after curative operations in colorectal cancer patients. J Surg Oncol. 2013; 108:9–13.9. Estrella JS, Othman ML, Taggart MW, Hamilton SR, Curley SA, Rashid A, et al. Intrabiliary growth of liver metastases: clinicopathologic features, prevalence, and outcome. Am J Surg Pathol. 2013; 37:1571–1579.10. Jennings PE, Rode J, Coral A, Dowsett J, Lees WR. Villous adenoma of the common hepatic duct: the role of ultrasound in management. Gut. 1990; 31:558–560.11. Chu P, Wu E, Weiss LM. Cytokeratin 7 and cytokeratin 20 expression in epithelial neoplasms: a survey of 435 cases. Mod Pathol. 2000; 13:962–972.12. Nanashima A, Tobinaga S, Araki M, Kunizaki M, Abe K, Hayashi H, et al. Intraductal papillary growth of liver metastasis originating from colon carcinoma in the bile duct: report of a case. Surg Today. 2011; 41:276–280.13. Kayashima H, Taketomi A, Yamashita Y, Kuroda Y, Kitagawa D, Harimoto N, et al. Liver metastasis with intraductal invasion originating from rectal cancer: report of a case. Surg Today. 2008; 38:765–768.14. Rullier A, Le Bail B, Fawaz R, Blanc JF, Saric J, Bioulac-Sage P. Cytokeratin 7 and 20 expression in cholangiocarcinomas varies along the biliary tract but still differs from that in colorectal carcinoma metastasis. Am J Surg Pathol. 2000; 24:870–876.15. Povoski SP, Klimstra DS, Brown KT, Schwartz LH, Kurtz RC, Jarnagin WR, et al. Recognition of intrabiliary hepatic metastases from colorectal adenocarcinoma. HPB Surg. 2000; 11:383–390.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Characteristics of Ovarian Metastasis from Colorectal Cancer
- Significance of p53 Overexpression in the Metastasis of Colorectal Cancer
- Cutaneous metastasis: a rare phenomenon of colorectal cancer
- Choroidal Metastasis from Colon Cancer Treated with Palliative Radiotherapy
- Acute Cholecystitis Associated with Gallbladder Metastasis of Gastric Cancer