Ann Hepatobiliary Pancreat Surg.
2017 Feb;21(1):17-20. 10.14701/ahbps.2017.21.1.17.
Importance of critical view of safety in laparoscopic cholecystectomy: a survey of 120 serial patients, with no incidence of complications
- Affiliations
-
- 1Department of General Surgery, Fatih Sultan Mehmet Training and Research Hospital, Istanbul, Turkey. drbkaya@yahoo.com
- KMID: 2371563
- DOI: http://doi.org/10.14701/ahbps.2017.21.1.17
Abstract
- BACKGROUNDS/AIMS
To determine the importance of critical view of safety techniques in laparoscopic cholecystectomy.
METHODS
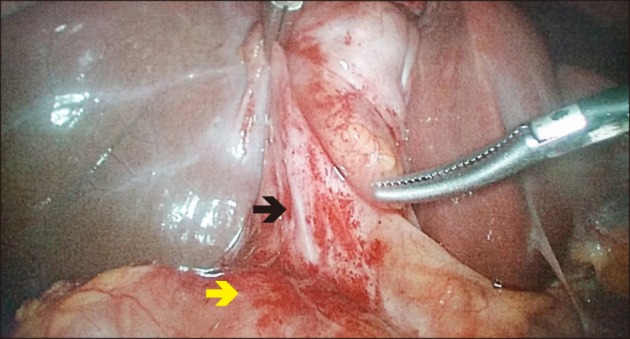
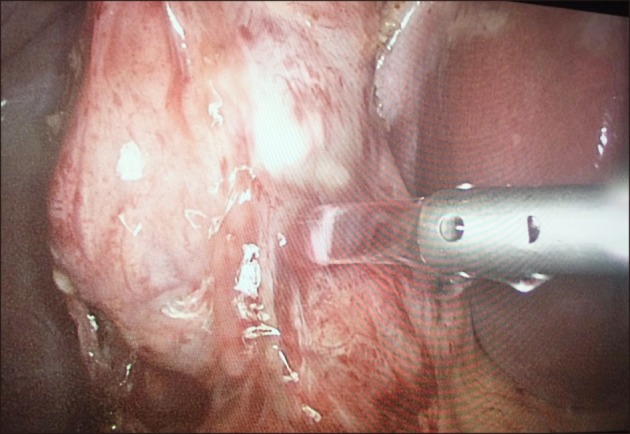
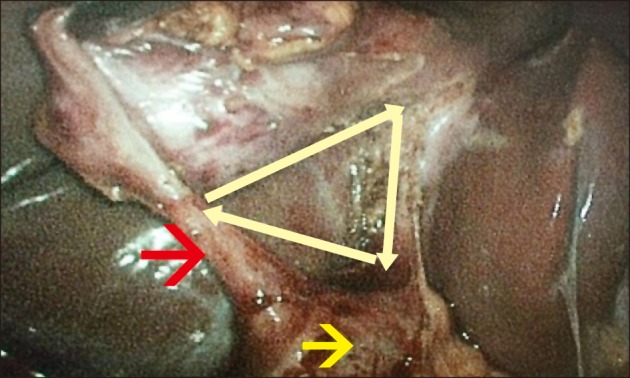
A total of 120 patients were included in the study, between January 2015 to March 2016. Hydrodissection was performed for cases presenting with severe adhesions or cholecystitis. A critical view of safety was performed for all patients undergoing the procedure for isolation of cystic duct and cystic artery with cystic plate dissection. Demographic characteristics of the patients, as well as intraoperative and postoperative minor or major complications were recorded.
RESULTS
A total of 81 (67.5%) female and 39 (32.5%) male patients succesfully underwent surgeries following the critical view of safety and hydrodissection technique. Acute/chronic cholecystitis, or severe adhesions in the surgical field, were detected in 34 (28.3%) patients. There were no intraoperative or postoperative biliary complications. Wound infection was detected in 5 (4.1%) patients. All patients were discharged on either the first, second or third postoperative day.
CONCLUSIONS
Biliary duct injury during laparoscopic cholecystectomy is an important complication. In this study, we show that the critical view of safety and hydrodissection techniquesminimizes the bile duct injury during laparoscopic cholecystectomy, including in difficult cases.
MeSH Terms
Figure
Reference
-
1. Yegiyants S, Collins JC. Operative strategy can reduce the incidence of major bile duct injury in laparoscopic cholecystectomy. Am Surg. 2008; 74:985–987. PMID: 18942628.
Article2. Archer SB, Brown DW, Smith CD, Branum GD, Hunter JG. Bile duct injury during laparoscopic cholecystectomy: results of a national survey. Ann Surg. 2001; 234:549–558. discussion 558-559. PMID: 11573048.3. Avgerinos C, Kelgiorgi D, Touloumis Z, Baltatzi L, Dervenis C. One thousand laparoscopic cholecystectomies in a single surgical unit using the “critical view of safety” technique. J Gastrointest Surg. 2009; 13:498–503. PMID: 19009323.
Article4. Sanjay P, Fulke JL, Exon DJ. ‘Critical view of safety’ as an alternative to routine intraoperative cholangiography during laparoscopic cholecystectomy for acute biliary pathology. J Gastrointest Surg. 2010; 14:1280–1284. PMID: 20535578.
Article5. Russell JC, Walsh SJ, Mattie AS, Lynch JT. Bile duct injuries, 1989-1993. A statewide experience. Connecticut Laparoscopic Cholecystectomy Registry. Arch Surg. 1996; 131:382–388. PMID: 8615723.6. Ooi LL, Goh YC, Chew SP, Tay KH, Foo E, Low CH, et al. Bile duct injuries during laparoscopic cholecystectomy: a collective experience of four teaching hospitals and results of repair. Aust N Z J Surg. 1999; 69:844–846. PMID: 10613280.
Article7. Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995; 180:101–125. PMID: 8000648.8. Vettoretto N, Saronni C, Harbi A, Balestra L, Taglietti L, Giovanetti M. Critical view of safety during laparoscopic cholecystectomy. JSLS. 2011; 15:322–325. PMID: 21985717.
Article9. Honda G, Iwanaga T, Kurata M, Watanabe F, Satoh H, Iwasaki K. The critical view of safety in laparoscopic cholecystectomy is optimized by exposing the inner layer of the subserosal layer. J Hepatobiliary Pancreat Surg. 2009; 16:445–449. PMID: 19259610.
Article10. Eikermann M, Siegel R, Broeders I, Dziri C, Fingerhut A, Gutt C, et al. Prevention and treatment of bile duct injuries during laparoscopic cholecystectomy: the clinical practice guidelines of the European Association for Endoscopic Surgery (EAES). Surg Endosc. 2012; 26:3003–3039. PMID: 23052493.
Article11. O'Kelly JA, De Marchi JA, Joyce WP. The critical view of safety in laparoscopic cholecystectomy: towards a national consensus. Ir Med J. 2015; 108:26. PMID: 25702354.12. Naude GP, Morris E, Bongard FS. Laparoscopic cholecystectomy facilitated by hydrodissection. J Laparoendosc Adv Surg Tech A. 1998; 8:215–218. PMID: 9755913.
Article13. Lubna H, Masoom MR. Hydro-dissection - A simple solution in difficult laparoscopic cholecystectomy. Mymensingh Med J. 2015; 24:592–595. PMID: 26329960.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- How to achieve the critical view of safety for safe laparoscopic cholecystectomy: Technical aspects
- Laparoscopic Cholecystectomy in the Second Trimester of Pregnancy
- Rouviere’s Sulcus: A Guide to Safe Laparoscopic Cholecystectomy
- A Clinical Analysis of 300 Case of Laparoscopic Cholecystectomy
- Comparison of Laparoscopic Cholecystectomy and Minilaparotomy Cholecystectomy