J Dent Rehabil Appl Sci.
2016 Dec;32(4):280-292. 10.14368/jdras.2016.32.4.280.
Factors associated with the survival and marginal bone loss of dental implants: a 5-year retrospective study
- Affiliations
-
- 1Department of Periodontology, Research Institute for Oral Sciences, College of Dentistry, Gangneung-Wonju National University, Gangneung, Republic of Korea. dentist@gwnu.ac.kr
- KMID: 2369068
- DOI: http://doi.org/10.14368/jdras.2016.32.4.280
Abstract
- PURPOSE
The purpose of this study was to compare the long-term survival rate and peri-implant marginal bone loss related to multiple risk factors including the clinician's experience.
MATERIALS AND METHODS
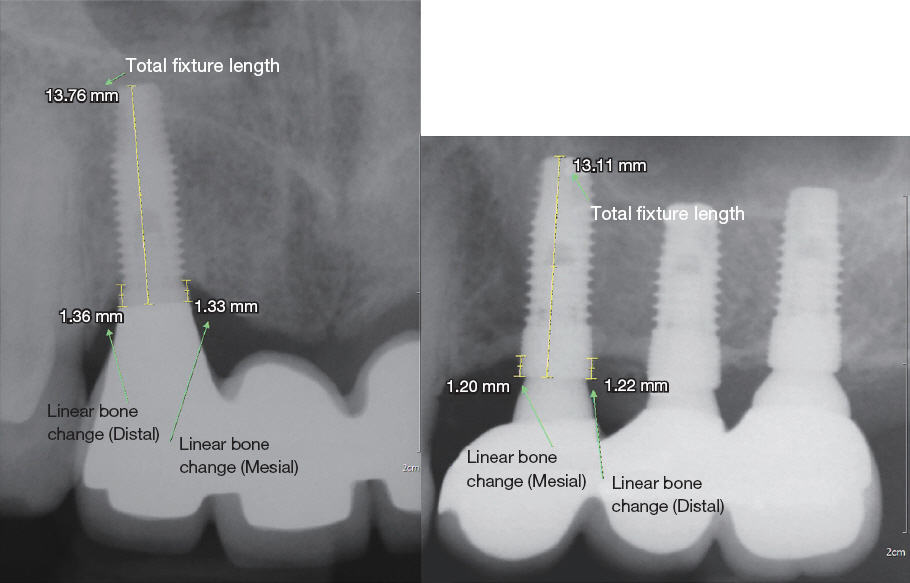
Four hundred twenty implants in 146 patients, who had involved a supportive periodontal therapy program every 3 to 6 months and had follow up data for at least 5 years, were selected as the study group. Peri-implant marginal bone loss, data of demographic, implant and surgical characteristics were collected from peri-apical radiographs and chart review. Implant survival was regarded as the remaining with radiographic marginal bone level in excess of 50% of the fixture length for any reason.
RESULTS
The cumulative survival rate after 5 years of loading was 94.9%. In binary logistic regression analysis, smoking status (P = 0.033) and presence of spontaneous cover screw exposure (P < 0.001) were significantly related to 5-year survival of implants. In stepwise multiple regression analysis, smoking status (P < 0.001), type of abutment connection (P < 0.001) and implant surface (P = 0.033) were significantly related to peri-implant marginal bone level. And the year of resident was not statistically related to 5-year implant survival in simple logistic regression analysis (P = 0.171).
CONCLUSION
Smoking status, spontaneous cover screw exposure, type of abutment connection and implant surface might influence the implant success. There was no significant correlation between the year of resident and implant failure.
MeSH Terms
Figure
Reference
-
References
1. Pjetursson BE, Zwahlen M, Lang NP. Quality of reporting of clinical studies to assess and compare performance of implant-supported restorations. J Clin Periodontol. 2012; 39:139–59. DOI: 10.1111/j.1600-051X.2011.01828.x. PMID: 22533954.2. Pjetursson BE, Tan K, Lang NP, Brägger U, Egger M, Zwahlen M. A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. Clin Oral Implants Res. 2004; 15:667–76. DOI: 10.1111/j.1600-0501.2004.01120.x.3. Vandeweghe S, De Bruyn H. The effect of smoking on early bone remodeling on surface modified Southern Implants®. Clin Implant Dent Relat Res. 2011; 13:206–14. DOI: 10.1111/j.1708-8208.2009.00198.x. PMID: 19744200.4. Rosen P, Clem D, Cochran D, Froum S, McAllister B, Renvert S, Wang HL. Peri-implant mucositis and peri-implantitis: a current understanding of their diagnoses and clinical implications. J Periodontol. 2013; 84:436–43. DOI: 10.1902/jop.2013.134001. PMID: 23537178.5. Costa FO, Takenaka-Martinez S, Cota LO, Ferreira SD, Silva GL, Costa JE. Peri-implant disease in subjects with and without preventive maintenance: a 5-year follow-up. J Clin Periodontol. 2012; 39:173–81. DOI: 10.1111/j.1600-051X.2011.01819.x. PMID: 22111654.6. Pjetursson BE, Helbling C, Weber HP, Matuliene G, Salvi GE, Brägger U, Schmidlin K, Zwahlen M, Lang NP. Peri-implantitis susceptibility as it relates to periodontal therapy and supportive care. Clin Oral Implants Res. 2012; 23:888–94. DOI: 10.1111/j.1600-0501.2012.02474.x. PMID: 22530771.7. Bain CA. Implant installation in the smoking patient. Periodontol 2000. 2003; 33:185–93. DOI: 10.1046/j.0906-6713.2003.03315.x. PMID: 12950851.8. Hinode D, Tanabe S, Yokoyama M, Fujisawa K, Yamauchi E, Miyamoto Y. Influence of smoking on osseointegrated implant failure: a meta-analysis. Clin Oral Implants Res. 2006; 17:473–8. DOI: 10.1111/j.1600-0501.2005.01244.x. PMID: 16907781.9. Klokkevold PR, Han TJ. How do smoking, diabetes, and periodontitis affect outcomes of implant treatment? Int J Oral Maxillofac Implants. 2007; 22(Suppl):173–202. PMID: 18437796.10. Strietzel FP, Reichart PA, Kale A, Kulkarni M, Wegner B, Küchler I. Smoking interferes with the prognosis of dental implant treatment: a systematic review and meta-analysis. J Clin Periodontol. 2007; 34:523–44. DOI: 10.1111/j.1600-051X.2007.01083.x. PMID: 17509093.11. Lambert PM, Morris HF, Ochi S. The influence of smoking on 3-year clinical success of osseointegrated dental implants. Ann Periodontol. 2000; 5:7989. DOI: 10.1902/annals.2000.5.1.79. PMID: 11885185.12. Kumar A, Jaffin RA, Berman C. The effect of smoking on achieving osseointegration of surfacemodified implants: a clinical report. Int J Oral Maxillofac Implants. 2002; 17:816–9. PMID: 12507241.13. Mellado-Valero A, Ferrer García JC, Herrera Ballester A, Labaig Rueda C. Effects of diabetes on the osseointegration of dental implants. Med Oral Patol Oral Cir Bucal. 2007; 12:E38–43. PMID: 17195826.14. Salvi GE, Carollo-Bittel B, Lang NP. Effects of diabetes mellitus on periodontal and peri-implant conditions: update on associations and risks. J Clin Periodontol. 2008; 35:398–409. DOI: 10.1111/j.1600-051X.2008.01282.x. PMID: 18724865.15. Enkling N, Jöhren P, Klimberg T, Mericske-Stern R, Jervøe-Storm PM, Bayer S, Gülden N, Jepsen S. Open or submerged healing of implants with platform switching: a randomized, controlled clinical trial. J Clin Periodontol. 2011; 38:374–84. DOI: 10.1111/j.1600-051X.2010.01683.x. PMID: 21235615.16. Haas R, Mensdorff-Pouilly N, Watzek G, Mailath M, Lill W, Reichsthaler J, Frey G, Thornton B. Kaplan und Meier - Vergleichsanalyse von 3000 gesetzten implantaten. GOI gesellschaft für orale implantologie. Jahrbuch für Orale Implantologie. 1994. Berlin: Quintessenz;p. 213–25.17. Preiskel HW, Tsolka P. Treatment outcomes in implant therapy: the influence of surgical and prosthodontic experience. Int J Prosthodont. 1995; 8:273–9. PMID: 10348597.18. Zoghbi SA, de Lima LA, Saraiva L, Romito GA. Surgical experience influences 2-stage implant os-seointegration. J Oral Maxillofac Surg. 2011; 69:2771–6. DOI: 10.1016/j.joms.2011.03.031. PMID: 21798649.19. Kohavi D, Azran G, Shapira L, Casap N. Retrospective clinical review of dental implants placed in a university training program. J Oral Implantol. 2004; 30:23–9. DOI: 10.1563/1548-1336(2004)030<0023:RCRODI>2.0.CO;2.20. Melo MD, Shafie H, Obeid G. Implant survival rates for oral and maxillofacial surgery residents: a retrospective clinical review with analysis of resident level of training on implant survival. J Oral Maxillofac Surg. 2006; 64:1185–9. DOI: 10.1016/j.joms.2006.04.014. PMID: 16860207.21. Zupnik J, Kim SW, Ravens D, Karimbux N, Guze K. Factors associated with dental implant survival: a 4-year retrospective analysis. J Periodontol. 2011; 82:1390–5. DOI: 10.1902/jop.2011.100685. PMID: 21417587.22. Chang M, Wennström JL, Odman P, Andersson B. Implant supported single-tooth replacements compared to contralateral natural teeth. Crown and soft tissue dimensions. Clin Oral Implants Res. 1999; 10:185–94. DOI: 10.1034/j.1600-0501.1999.100301.x. PMID: 10522178.23. Reddy MS, Mayfield-Donahoo T, Vanderven FJ, Jeffcoat MK. A comparison of the diagnostic advantages of panoramic radiography and computed tomography scanning for placement of root form dental implants. Clin Oral Implants Res. 1994; 5:22938. DOI: 10.1034/j.1600-0501.1994.050406.x.24. De Bruyn H, Vandeweghe S, Ruyffelaert C, Cosyn J, Sennerby L. Radiographic evaluation of modern oral implants with emphasis on crestal bone level and relevance to peri-implant health. Periodontol 2000. 2013; 62:256–70. DOI: 10.1111/prd.12004. PMID: 23574471.25. Cardaropoli G, Lekholm U, Wennström JL. Tissue alterations at implant-supported single-tooth replacements: a 1-year prospective clinical study. Clin Oral Implants Res. 2006; 17:165–71. DOI: 10.1111/j.1600-0501.2005.01210.x. PMID: 16584412.26. Manz MC. Factors associated with radiographic vertical bone loss around implants placed in a clinical study. Ann Periodontol. 2000; 5:137–51. DOI: 10.1902/annals.2000.5.1.137. PMID: 11885173.27. Roos J, Sennerby L, Lekholm U, Jemt T, Gröndahl K, Albrektsson T. A qualitative and quantitative method for evaluating implant success: a 5-year retrospective analysis of the Brånemark implant. Int J Oral Maxillofac Implants. 1997; 12:504–14. PMID: 9274079.28. Heitz-Mayfield LJ, Huynh-Ba G. History of treated periodontitis and smoking as risks for implant therapy. Int J Oral Maxillofac Implants. 2009; 24(Suppl):39–68. PMID: 19885434.29. Bain CA, Moy PK. The association between the failure of dental implants and cigarette smoking. Int J Oral Maxillofac Implants. 1993; 8:609–15. PMID: 8181822.30. Wennström JL, Palmer RM. Consensus report of session C. Lang NP, Karring T, Lindhe J, editors. Proceedings of the 3rd European Workshop on Periodontology. Berlin: Quintessenz Verlags;1999. p. 255–9. PMCID: PMC104388.31. Berglundh T, Persson L, Klinge B. A systematic review of the incidence of biological and technical complications in implant dentistry reported in prospective longitudinal studies of at least 5 years. J Clin Periodontol. 2002; 29:197–212. DOI: 10.1034/j.1600-051X.29.s3.12.x. PMID: 12787220.32. Ekfeldt A, Christiansson U, Eriksson T, Lindén U, Lundqvist S, Rundcrantz T, Johansson LA, Nilner K, Billström C. A retrospective analysis of factors associated with multiple implant failures in maxillae. Clin Oral Implants Res. 2001; 12:462–7. DOI: 10.1034/j.1600-0501.2001.120505.x. PMID: 11564105.33. Schwartz-Arad D, Dolev E. The challenge of endosseous implants placed in the posterior partially edentulous maxilla: a clinical report. Int J Oral Maxillofac Implants. 2000; 15:261–4. PMID: 10795459.34. Koo KT, Lee EJ, Kim JY, Seol YJ, Han JS, Kim TI, Lee YM, Ku Y, Wikesjö UM, Rhyu IC. The effect of internal versus external abutment connection modes on crestal bone changes around dental implants: a radiographic analysis. J Periodontol. 2012; 83:1104–9. DOI: 10.1902/jop.2011.110456. PMID: 22145806.35. Peñarrocha-Diago MA, Flichy-Fernández AJ, Alonso-González R, Peñarrocha-Oltra D, BalaguerMartínez J, Peñarrocha-Diago M. Influence of implant neck design and implant-abutment connection type on peri-implant health. Radiological study. Clin Oral Implants Res. 2013; 24:1192–200. PMID: 22925048.36. Vázquez Álvarez R, Pérez Sayáns M, Gayoso Diz P, García García A. Factors affecting peri-implant bone loss: a post-five-year retrospective study. Clin Oral Implants Res. 2015; 26:1006–14. DOI: 10.1111/clr.12416. PMID: 24978819.37. Abrahamsson I, Berglundh T. Effects of different implant surfaces and designs on marginal bone level alterations: a review. Clin Oral Implants Res. 2009; 20:207–15. DOI: 10.1111/j.1600-0501.2009.01783.x. PMID: 19663966.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Influence of crown-to-implant ratio on periimplant marginal bone loss in the posterior region: a five-year retrospective study
- Comparison of marginal bone loss of dental implants and adjacent teeth in the same interproximal unit: a retrospective study with follow-up over 2 years after prosthesis delivery
- Long-term effect of implant-abutment connection type on marginal bone loss and survival of dental implants
- Retrospective study on marginal bone loss around maxillary anterior implants with or without bone graft
- RADIOGRAGHIC STUDY OF MARGINAL BONE LOSS AROUND OSSEOINTEGRATED IMPLANTS AFTER FUNCTIONAL LOADING