Healthc Inform Res.
2017 Jan;23(1):43-52. 10.4258/hir.2017.23.1.43.
Applying of Decision Tree Analysis to Risk Factors Associated with Pressure Ulcers in Long-Term Care Facilities
- Affiliations
-
- 1College of Nursing, the Research Institute of Nursing Science, Kyungpook National University, Daegu, Korea.
- 2College of Nursing, Keimyung University, Daegu, Korea. soo1005@kmu.ac.kr
- KMID: 2368984
- DOI: http://doi.org/10.4258/hir.2017.23.1.43
Abstract
OBJECTIVES
The purpose of this study was to use decision tree analysis to explore the factors associated with pressure ulcers (PUs) among elderly people admitted to Korean long-term care facilities.
METHODS
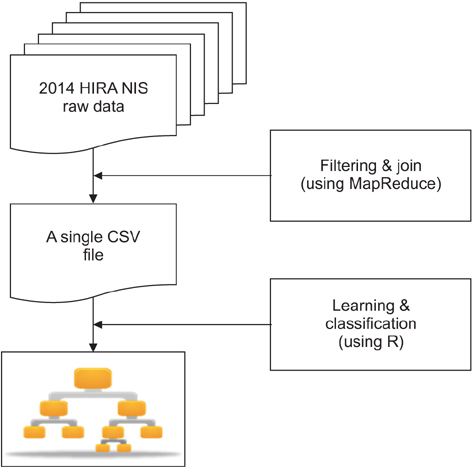
The data were extracted from the 2014 National Inpatient Sample (NIS)"”data of Health Insurance Review and Assessment Service (HIRA). A MapReduce-based program was implemented to join and filter 5 tables of the NIS. The outcome predicted by the decision tree model was the prevalence of PUs as defined by the Korean Standard Classification of Disease-7 (KCD-7; code L89*). Using R 3.3.1, a decision tree was generated with the finalized 15,856 cases and 830 variables.
RESULTS
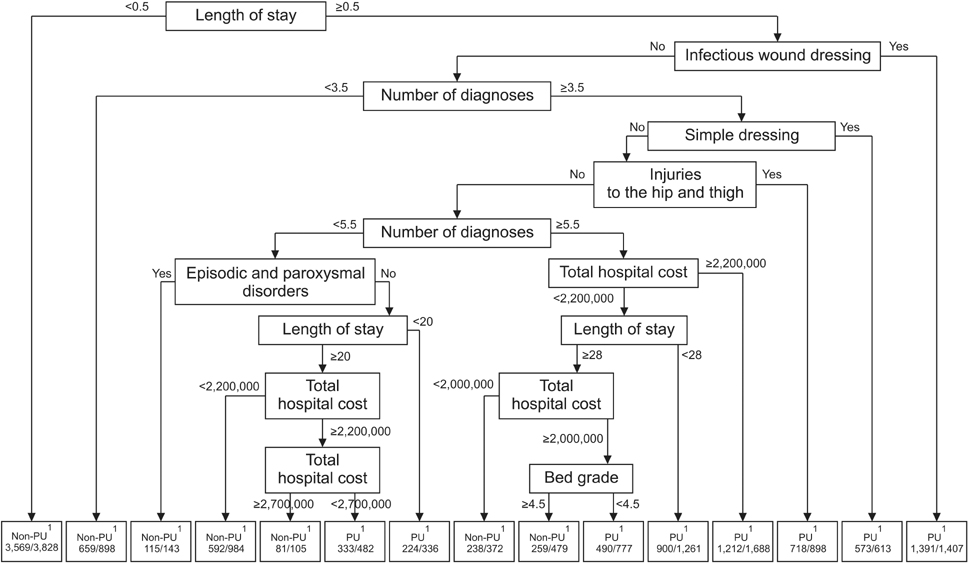
The decision tree displayed 15 subgroups with 8 variables showing 0.804 accuracy, 0.820 sensitivity, and 0.787 specificity. The most significant primary predictor of PUs was length of stay less than 0.5 day. Other predictors were the presence of an infectious wound dressing, followed by having diagnoses numbering less than 3.5 and the presence of a simple dressing. Among diagnoses, "injuries to the hip and thigh" was the top predictor ranking 5th overall. Total hospital cost exceeding 2,200,000 Korean won (US $2,000) rounded out the top 7.
CONCLUSIONS
These results support previous studies that showed length of stay, comorbidity, and total hospital cost were associated with PUs. Moreover, wound dressings were commonly used to treat PUs. They also show that machine learning, such as a decision tree, could effectively predict PUs using big data.
MeSH Terms
Figure
Cited by 2 articles
-
Machine Learning to Compare Frequent Medical Problems of African American and Caucasian Diabetic Kidney Patients
Yong-Mi Kim, Pranay Kathuria, Dursun Delen
Healthc Inform Res. 2017;23(4):241-248. doi: 10.4258/hir.2017.23.4.241.Comparison of Models for the Prediction of Medical Costs of Spinal Fusion in Taiwan Diagnosis-Related Groups by Machine Learning Algorithms
Ching-Yen Kuo, Liang-Chin Yu, Hou-Chaung Chen, Chien-Lung Chan
Healthc Inform Res. 2018;24(1):29-37. doi: 10.4258/hir.2018.24.1.29.
Reference
-
1. National Pressure Ulcer Advisory Panel. European Pressure Ulcer Advisory Panel. Pan Pacific Pressure Injury Alliance. Prevention and treatment of pressure ulcers: quick reference guide. 2nd ed. Perth, Australia: Cambridge Media;2014.2. Demarre L, Verhaeghe S, Annemans L, Van Hecke A, Grypdonck M, Beeckman D. The cost of pressure ulcer prevention and treatment in hospitals and nursing homes in Flanders: a cost-of-illness study. Int J Nurs Stud. 2015; 52(7):1166–1179.
Article3. Gunningberg L, Stotts NA. Tracking quality over time: what do pressure ulcer data show? Int J Qual Health Care. 2008; 20(4):246–253.
Article4. Lyder CH, Ayello EA. Pressure ulcers: a patient safety issue. In : Hughes RG, editor. Patient safety and quality: an evidence-based handbook for nurses. Rockville (MD): Agency for Healthcare Research and Quality;2008.5. Mueller C, Karon SL. ANA nurse sensitive quality indicators for long-term care facilities. J Nurs Care Qual. 2004; 19(1):39–47.
Article6. Keelaghan E, Margolis D, Zhan M, Baumgarten M. Prevalence of pressure ulcers on hospital admission among nursing home residents transferred to the hospital. Wound Repair Regen. 2008; 16(3):331–336.
Article7. National Health Insurance Service. Long-term care insurance [Internet]. Wonju, Korea: National Health Insurance Service;2010. cited at 2017 Jan 23. Available from: http://longtermcare.or.kr/npbs/e/e/100/index.web.8. Korean Health Industry Development Institute. KHISS current state of long term care facilities [Internet]. Cheongju, Korea: Korean Health Industry Development Institute;2014. cited at 2017 Jan 23. Available from: http://www.khiss.go.kr/treeManager.do?task=treeFrm&vw_cd=MT_ITITLE&list_id=358_E&htxt_code=125369725751510746110771881221239.9. Lahmann NA, Tannen A, Kuntz S, Raeder K, Schmitz G, Dassen T, et al. Mobility is the key! Trends and associations of common care problems in German long-term care facilities from 2008 to 2012. Int J Nurs Stud. 2015; 52(1):167–174.
Article10. Shin JH, Hyun TK. Nurse staffing and quality of care of nursing home residents in Korea. J Nurs Scholarsh. 2015; 47(6):555–564.
Article11. Coleman S, Gorecki C, Nelson EA, Closs SJ, Defloor T, Halfens R, et al. Patient risk factors for pressure ulcer development: systematic review. Int J Nurs Stud. 2013; 50(7):974–1003.
Article12. Murdoch TB, Detsky AS. The inevitable application of big data to health care. JAMA. 2013; 309(13):1351–1352.
Article13. Kim L, Kim JA, Kim S. A guide for the utilization of Health Insurance Review and Assessment Service National Patient Samples. Epidemiol Health. 2014; 36:e2014008.
Article14. Frost & Sullivan. Drowning in big data? Reducing information technology complexities and costs for healthcare organizations [Internet]. Mountain View (CA): Frost & Sullivan;2011. cited at 2017 Jan 23. Available from: https://www.emc.com/collateral/analyst-reports/frostsullivan-reducing-information-technology-complexities-ar.pdf.15. Raghupathi W, Raghupathi V. Big data analytics in healthcare: promise and potential. Health Inf Sci Syst. 2014; 2:3.
Article16. Bellazzi R, Zupan B. Predictive data mining in clinical medicine: current issues and guidelines. Int J Med Inform. 2008; 77(2):81–97.
Article17. Pedrassani de Lira C, Toniazzo de Abreu LL, Veiga Silva AC, Mazzuchello LL, Rosa MI, Comunello E, et al. Use of data mining to predict the risk factors associated with osteoporosis and osteopenia in women. Comput Inform Nurs. 2016; 34(8):369–375.
Article18. Raju D, Su X, Patrician PA, Loan LA, McCarthy MS. Exploring factors associated with pressure ulcers: a data mining approach. Int J Nurs Stud. 2015; 52(1):102–111.
Article19. Kang Y, McHugh MD, Chittams J, Bowles KH. Utilizing home healthcare electronic health records for telehomecare patients with heart failure: a decision tree approach to detect associations with rehospitalizations. Comput Inform Nurs. 2016; 34(4):175–182.
Article20. Michelet D, Andreu-Gallien J, Skhiri A, Bonnard A, Nivoche Y, Dahmani S. Factors affecting recovery of postoperative bowel function after pediatric laparoscopic surgery. J Anaesthesiol Clin Pharmacol. 2016; 32(3):369–375.
Article21. Kim SR, Kim HK, Kim JY, Kim HY, Ko SH, Park M. Smoking cessation failure among Korean adolescents. J Sch Nurs. 2016; 32(3):155–163.
Article22. Ramezankhani A, Pournik O, Shahrabi J, Khalili D, Azizi F, Hadaegh F. Applying decision tree for identification of a low risk population for type 2 diabetes. Tehran Lipid and Glucose Study. Diabetes Res Clin Pract. 2014; 105(3):391–398.
Article23. Lee TT, Lin KC, Mills ME, Kuo YH. Factors related to the prevention and management of pressure ulcers. Comput Inform Nurs. 2012; 30(9):489–495.
Article24. Dean J, Ghemawat S. MapReduce: simplified data processing on large clusters. Commun ACM. 2008; 51(1):107–113.25. Korea Ministry of Food and Drug Society. Regulation on drug classification numbers [Internet]. Cheongju, Korea: Ministry of Food and Drug Society;2013. cited at 2017 Jan 4. Available from: http://www.mfds.go.kr/index.do?mid=1015&pageNo=6&seq=6325&sitecode=2013-04-05&cmd=v.26. Korean Standard Statistical Classification. The standard of classification of disease and cause of death [Internet]. Daejeon, Korea: Korean Standard Statistical Classification;2016. cited at 2017 Jan 2. Available from: https://kssc.kostat.go.kr:8443/ksscNew_web/link.do?gubun=004.27. Baratloo A, Hosseini M, Negida A, El Ashal G. Part 1: Simple definition and calculation of accuracy, sensitivity and specificity. Emerg (Tehran). 2015; 3(2):48–49.28. Graves N, Birrell F, Whitby M. Effect of pressure ulcers on length of hospital stay. Infect Control Hosp Epidemiol. 2005; 26(3):293–297.
Article29. Santamaria N, Carville K, Prentice J, Ellis I, Ellis T, Lewin G, et al. Pressure ulcer prevalence and its relationship to comorbidity in nursing home residents: results from phase 1 of the PRIME Trial. Prim Intent Aust J Wound Manag. 2005; 13(3):107–116.30. Dealey C, Posnett J, Walker A. The cost of pressure ulcers in the United Kingdom. J Wound Care. 2012; 21(6):261–266.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors Affecting Pressure Ulcer among Inpatients in Long Term Care Facilities: Adults with Cognitive Impairment
- Evaluation of Risk for Pressure Ulcers Using the Braden Scale in Elderly Patients Receiving Long-Term Care
- Ownership of Long-Term Care Facility and Incidence of Pressure Ulcers among Republic of Korea
- Risk Factors for Pressure Ulcer by Electrodes in Long-term Electroencephalography Monitoring
- Effects of excretion care with a smart automatic defecation treatment system on skin humidity, incontinence-associated dermatitis, and pressure ulcers of patients with incontinence residing in long-term care facilities: Non-equivalent control group non-synchronized design