Ann Dermatol.
2014 Jun;26(3):385-391.
Two Clinically Unusual Cases of Folliculotropic Mycosis Fungoides: One with and the Other without Syringotropism
- Affiliations
-
- 1Department of Dermatology, School of Medicine, Acibadem University, Istanbul, Turkey. ozgurtimurkaynak@hotmail.com
- 2Department of Dermatology, School of Medicine, Marmara University, Istanbul, Turkey.
- 3Department of Pathology, Cerrahpasa Medical Faculty, Istanbul University, Istanbul, Turkey.
- 4Department of Dermatology, Istanbul Medical Faculty, Istanbul University, Istanbul, Turkey.
- 5Department of Pathology, Istanbul Medical Faculty, Istanbul University, Istanbul, Turkey.
Abstract
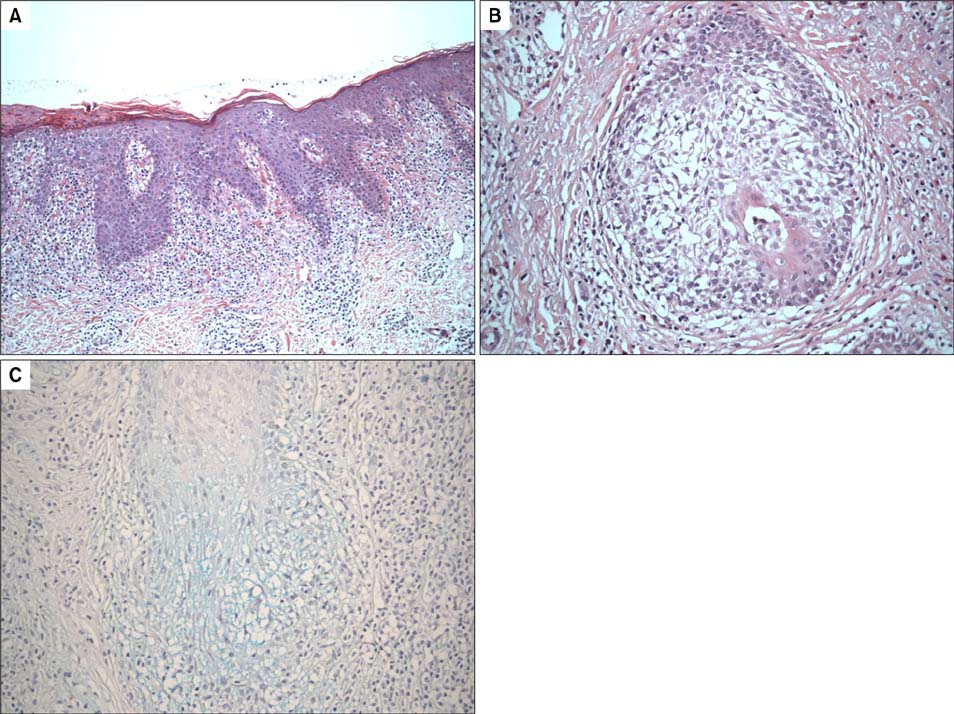
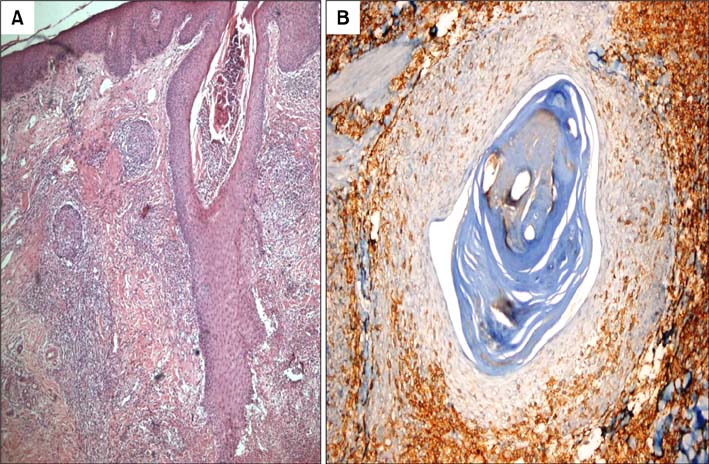
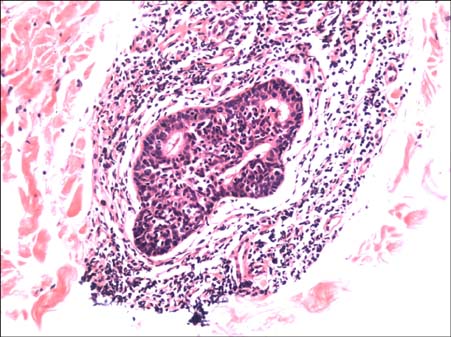
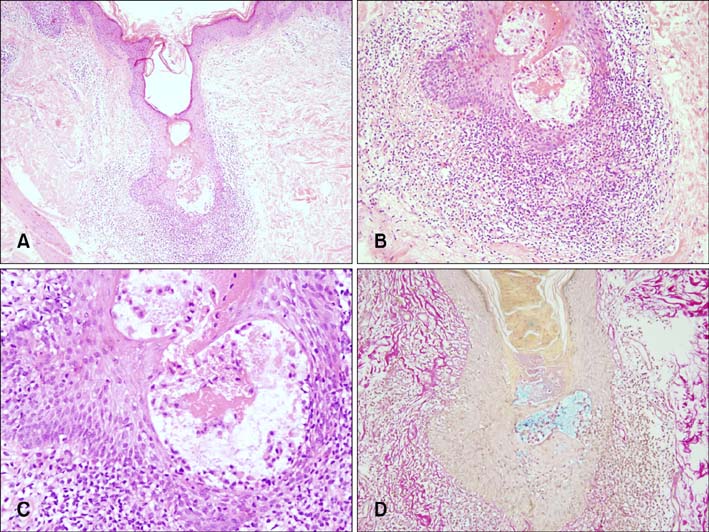
- Mycosis fungoides is the most common form of cutaneous T-cell lymphoma, and it rarely exhibits predilection for hair follicle and eccrine gland infiltration. Here, we present 2 similar cases that display folliculotropism with varying amounts of follicular mucinosis, with and without syringotropism. The features observed in both cases were cystic, comedo-like, acneiform lesions; generalized involvement with loss of body hair; pruritus; and hidradenitis suppurativa-like lesions. Hypohidrosis as well as nail and palmoplantar involvement with lichen planopilaris-like clinical features were unique characteristics of the first case. Despite the well-known aggressive behavior of follicular mycosis fungoides, the presented cases had a subtle, slowly progressive, but persistent, clinical course. Folliculotropic and syringotropic mycosis fungoides are variants of cutaneous T-cell lymphoma. Clinical presentations might be challenging, and multiple, deep biopsy specimens containing adnexal structures are required for this critical diagnosis. Aggressive treatment may not be necessary in cases having an indolent course, especially in those with syringotropism.
Keyword
MeSH Terms
Figure
Reference
-
1. Willemze R, Jaffe ES, Burg G, Cerroni L, Berti E, Swerdlow SH, et al. WHO-EORTC classification for cutaneous lymphomas. Blood. 2005; 105:3768–3785.
Article2. Yost JM, Do TT, Kovalszki K, Su L, Anderson TF, Gudjonsson JE. Two cases of syringotropic cutaneous T-cell lymphoma and review of the literature. J Am Acad Dermatol. 2009; 61:133–138.
Article3. Hitchcock MG, Burchette JL Jr, Olsen EA, Ratech H, Kamino H. Eccrine gland infiltration by mycosis fungoides. Am J Dermatopathol. 1996; 18:447–453.
Article4. Hodak E, Feinmesser M, Segal T, Yosipovitch G, Lapidoth M, Maron L, et al. Follicular cutaneous T-cell lymphoma: a clinicopathological study of nine cases. Br J Dermatol. 1999; 141:315–322.
Article5. Rongioletti F, Smoller B. The histologic value of adnexal (eccrine gland and follicle) infiltration in mycosis fungoides. J Cutan Pathol. 2000; 27:406–409.
Article6. van Doorn R, Scheffer E, Willemze R. Follicular mycosis fungoides, a distinct disease entity with or without associated follicular mucinosis: a clinicopathologic and follow-up study of 51 patients. Arch Dermatol. 2002; 138:191–198.7. Gómez-Diez S, Maldonado C, Fueyo A, Vázquez-López F, Fresno MF, Pérez-Oliva N. Folliculotropic mycosis fungoides. Study of four cases. Actas Dermosifiliogr. 2007; 98:486–490.
Article8. Gerami P, Rosen S, Kuzel T, Boone SL, Guitart J. Folliculotropic mycosis fungoides: an aggressive variant of cutaneous T-cell lymphoma. Arch Dermatol. 2008; 144:738–746.9. Lehman JS, Cook-Norris RH, Weed BR, Weenig RH, Gibson LE, Weaver AL, et al. Folliculotropic mycosis fungoides: single-center study and systematic review. Arch Dermatol. 2010; 146:607–613.10. Muniesa C, Estrach T, Pujol RM, Gallardo F, Garcia-Muret P, Climent J, et al. Folliculotropic mycosis fungoides: clinicopathological features and outcome in a series of 20 cases. J Am Acad Dermatol. 2010; 62:418–426.
Article11. Gerami P, Guitart J. The spectrum of histopathologic and immunohistochemical findings in folliculotropic mycosis fungoides. Am J Surg Pathol. 2007; 31:1430–1438.
Article12. Thein M, Ravat F, Orchard G, Calonje E, Russell-Jones R. Syringotropic cutaneous T-cell lymphoma: an immunophenotypic and genotypic study of five cases. Br J Dermatol. 2004; 151:216–226.
Article13. van Doorn R, Van Haselen CW, van Voorst Vader PC, Geerts ML, Heule F, de Rie M, et al. Mycosis fungoides: disease evolution and prognosis of 309 Dutch patients. Arch Dermatol. 2000; 136:504–510.14. Talpur R, Bassett R, Duvic M. Prevalence and treatment of Staphylococcus aureus colonization in patients with mycosis fungoides and Sézary syndrome. Br J Dermatol. 2008; 159:105–112.
Article15. Kazakov DV, Burg G, Kempf W. Clinicopathological spectrum of mycosis fungoides. J Eur Acad Dermatol Venereol. 2004; 18:397–415.
Article16. Resnik KS, Kantor GR, Lessin SR, Kadin ME, Chooback L, Cooper HS, et al. Mycosis fungoides palmaris et plantaris. Arch Dermatol. 1995; 131:1052–1056.
Article17. Topf S, Lüftl M, Neisius U, Brabletz T, Simon M Jr, Schuler G, et al. Mycosis fungoides palmaris et plantaris--an unusual variant of cutaneous T-cell lymphoma. Eur J Dermatol. 2006; 16:84–86.18. Grande-Sarpa H, Callis Duffin KP, Florell SR. Onychodystrophy and tumor-stage mycosis fungoides confined to a single digit: report of a case and review of nail findings in cutaneous T-cell lymphoma. J Am Acad Dermatol. 2008; 59:154–157.
Article19. Matsuoka Y, Yoneda K, Katsuura J, Moriue T, Nakai K, Sadahira C, et al. Successful treatment of follicular cutaneous T-cell lymphoma without mucinosis with narrow-band UVB irradiation. J Eur Acad Dermatol Venereol. 2007; 21:1121–1122.
Article20. Olsen E, Vonderheid E, Pimpinelli N, Willemze R, Kim Y, Knobler R, et al. ISCL/EORTC. Revisions to the staging and classification of mycosis fungoides and Sezary syndrome: a proposal of the International Society for Cutaneous Lymphomas (ISCL) and the cutaneous lymphoma task force of the European Organization of Research and Treatment of Cancer (EORTC). Blood. 2007; 110:1713–1722.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Folliculotropic Mycosis Fungoides in 20 Korean Cases: Clinical and Histopathologic Features and Response to Ultraviolet A-1 and/or Photodynamic Therapy
- Classic Mycosis Fungoides Concomitant with Hypopigmented Mycosis Fungoides
- Follicular Mycosis Fungoides Mimicking Milia
- A Case of Hypopigmented Mycosis Fungoides
- A Case of Mycosis Fungoides Palmaris et Plantaris