Ann Surg Treat Res.
2017 Feb;92(2):105-109. 10.4174/astr.2017.92.2.105.
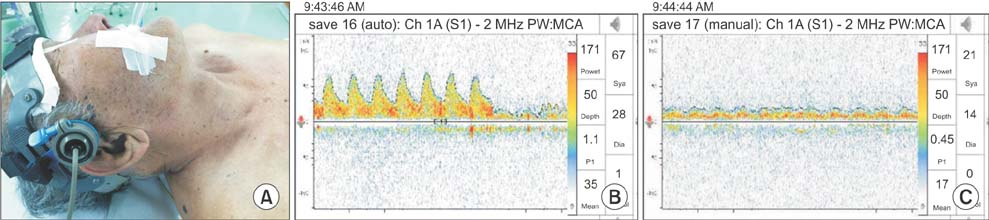
Cerebral monitoring during carotid endarterectomy by transcranial Doppler ultrasonography
- Affiliations
-
- 1Division of Transplantation and Vascular Surgery, Department of Surgery, Yeungnam University Medical Center, Yeungnam University College of Medicine, Daegu, Korea. wsyun@ynu.ac.kr
- KMID: 2367923
- DOI: http://doi.org/10.4174/astr.2017.92.2.105
Abstract
- PURPOSE
To evaluate the efficacy and safety of cerebral monitoring by transcranial Doppler ultrasonography (TCD) for the detection of cerebral ischemia during carotid endarterectomy (CEA).
METHODS
From August 2004 to December 2013, 159 CEAs were performed in a tertiary hospital. All procedures were performed under general anesthesia. Intraoperative TCD was routinely used to detect cerebral ischemia. Of the 159 patients, 102 patients were included in this study, excluding 27 patients who had a poor transtemporal isonation window and 30 patients who used additional cerebral monitoring systems such as electroencephalography or somatosensory evoked potentials. When mean flow velocity in the ipsilateral middle cerebral artery decreased by >50% versus baseline during carotid clamping carotid shunting was selectively performed. The carotid shunt rate and incidence of perioperative (<30 days) stroke or death were investigated by reviewing medical records.
RESULTS
Carotid shunting was performed in 31 of the 102 patients (30%). Perioperative stroke occurred in 2 patients (2%); a minor ischemic stroke caused by embolism in one and an intracerebral hemorrhage in the other. Perioperative death developed in the latter patient.
CONCLUSION
TCD is a safe cerebral monitoring tool to detect cerebral ischemia during CEA. It can reduce use of carotid shunt.
MeSH Terms
Figure
Reference
-
1. North American Symptomatic Carotid Endarterectomy Trial Collaborators. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med. 1991; 325:445–453.2. Endarterectomy for asymptomatic carotid artery stenosis. Executive Committee for the Asymptomatic Carotid Atherosclerosis Study. JAMA. 1995; 273:1421–1428.3. Barnett HJ, Taylor DW, Eliasziw M, Fox AJ, Ferguson GG, Haynes RB, et al. Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med. 1998; 339:1415–1425.4. Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST). Lancet. 1998; 351:1379–1387.5. Halliday A, Mansfield A, Marro J, Peto C, Peto R, Potter J, et al. Prevention of disabling and fatal strokes by successful carotid endarterectomy in patients without recent neurological symptoms: randomised controlled trial. Lancet. 2004; 363:1491–1502.6. Brott TG, Halperin JL, Abbara S, Bacharach JM, Barr JD, Bush RL, et al. 2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease: executive summary. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American Stroke Association, American Association of Neuroscience Nurses, American Association of Neurological Surgeons, American College of Radiology, American Society of Neuroradiology, Congress of Neurological Surgeons, Society of Atherosclerosis Imaging and Prevention, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of NeuroInterventional Surgery, Society for Vascular Medicine, and Society for Vascular Surgery. Circulation. 2011; 124:489–532.7. Liapis CD, Bell PR, Mikhailidis D, Sivenius J, Nicolaides A, Fernandes e Fernandes J, et al. ESVS guidelines. Invasive treatment for carotid stenosis: indications, techniques. Eur J Vasc Endovasc Surg. 2009; 37:4 Suppl. 1–19.8. Hans SS, Jareunpoon O. Prospective evaluation of electroencephalography, carotid artery stump pressure, and neurologic changes during 314 consecutive carotid endarterectomies performed in awake patients. J Vasc Surg. 2007; 45:511–515.9. Lawrence PF, Alves JC, Jicha D, Bhirangi K, Dobrin PB. Incidence, timing, and causes of cerebral ischemia during carotid endarterectomy with regional anesthesia. J Vasc Surg. 1998; 27:329–334.10. McCarthy RJ, Walker R, McAteer P, Budd JS, Horrocks M. Patient and hospital benefits of local anaesthesia for carotid endarterectomy. Eur J Vasc Endovasc Surg. 2001; 22:13–18.11. Stoughton J, Nath RL, Abbott WM. Comparison of simultaneous electroencephalographic and mental status monitoring during carotid endarterectomy with regional anesthesia. J Vasc Surg. 1998; 28:1014–1021.12. Chongruksut W, Vaniyapong T, Rerkasem K. Routine or selective carotid artery shunting for carotid endarterectomy (and different methods of monitoring in selective shunting). Cochrane Database Syst Rev. 2014; (6):CD000190.13. GALA Trial Collaborative Group. Lewis SC, Warlow CP, Bodenham AR, Colam B, Rothwell PM, et al. General anaesthesia versus local anaesthesia for carotid surgery (GALA): a multicentre, randomised controlled trial. Lancet. 2008; 372:2132–2142.14. Hafner CD, Evans WE. Carotid endarterectomy with local anesthesia: results and advantages. J Vasc Surg. 1988; 7:232–239.15. Cao P, Giordano G, Zannetti S, De Rango P, Maghini M, Parente B, et al. Transcranial Doppler monitoring during carotid endarterectomy: is it appropriate for selecting patients in need of a shunt? J Vasc Surg. 1997; 26:973–979.16. Ali AM, Green D, Zayed H, Halawa M, El-Sakka K, Rashid HI. Cerebral monitoring in patients undergoing carotid endarterectomy using a triple assessment technique. Interact Cardiovasc Thorac Surg. 2011; 12:454–457.17. Moritz S, Kasprzak P, Arlt M, Taeger K, Metz C. Accuracy of cerebral monitoring in detecting cerebral ischemia during carotid endarterectomy: a comparison of transcranial Doppler sonography, nearinfrared spectroscopy, stump pressure, and somatosensory evoked potentials. Anesthesiology. 2007; 107:563–569.18. Artru AA, Strandness DE Jr. Delayed carotid shunt occlusion detected by electroencephalographic monitoring. J Clin Monit. 1989; 5:119–122.19. Blackshear WM Jr, Di Carlo V, Seifert KB, Connar RG. Advantages of continuous electroencephalographic monitoring during carotid artery surgery. J Cardiovasc Surg (Torino). 1986; 27:146–153.20. Cho I, Smullens SN, Streletz LJ, Fariello RG. The value of intraoperative EEG monitoring during carotid endarterectomy. Ann Neurol. 1986; 20:508–512.21. Ackerstaff RG, Moons KG, van de Vlasakker CJ, Moll FL, Vermeulen FE, Algra A, et al. Association of intraoperative transcranial doppler monitoring variables with stroke from carotid endarterectomy. Stroke. 2000; 31:1817–1823.22. Pennekamp CW, Moll FL, de Borst GJ. The potential benefits and the role of cerebral monitoring in carotid endarterectomy. Curr Opin Anaesthesiol. 2011; 24:693–697.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Near-Infrared Spectroscopy versus Transcranial Doppler-Based Monitoring in Carotid Endarterectomy
- Cerebral Oxygen Saturation Monitoring during Carotid Endarterectomy: A case report
- Transcranial Doppler Monitoring in Subarachnoid Hemorrhage
- The Efficacy of Electroencephalography and Somatosensory Evoked Potential Monitoring for Detecting Cerebral Ischemia during Carotid Endarterectomy under Regional Anesthesia
- General principles of carotid Doppler ultrasonography