Perinatology.
2016 Dec;27(4):244-250. 10.14734/PN.2016.27.4.244.
Clinical Outcomes of Renal Pelvis Dilatation in Very Low Birth Weight Infants
- Affiliations
-
- 1Department of Pediatrics, Yonsei University College of Medicine, Seoul, Korea. smlee@yuhs.ac
- KMID: 2367036
- DOI: http://doi.org/10.14734/PN.2016.27.4.244
Abstract
- PURPOSE
The aim of this study was to evaluate this clinical outcome of neonatal pelvis dilatation in very low birth weight (VLBW) infants.
METHODS
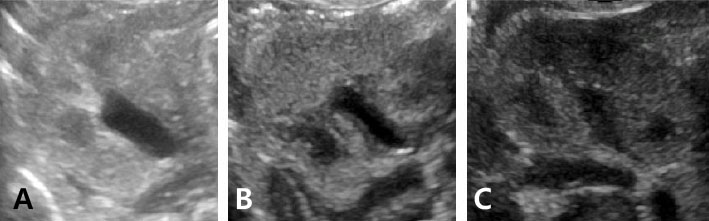
The medical records of 127 VLBW infants admitted to two neonatal intensive care units from January 2012 to December 2014 were retrospectively analyzed. Renal pelvis dilatation was diagnosed via ultrasound examination with cases divided into 3 groups: mild (dilatation of 5-10 mm), moderate (11-15 mm) and severe (≥15 mm). The correlation between the 3 dilatation groups and progression into hydronephrosis was evaluated.
RESULTS
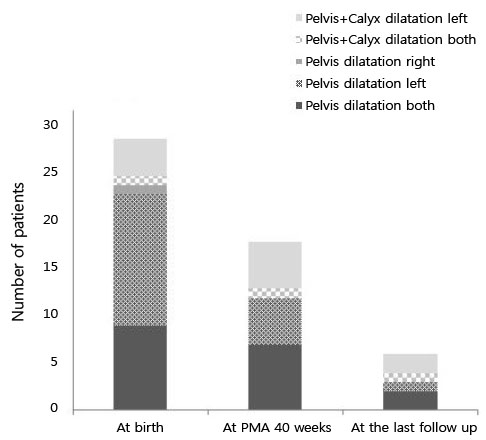
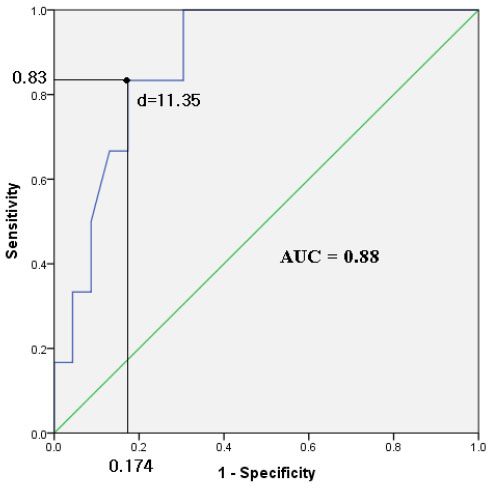
Among the 127 premature infants, renal pelvis dilatation was identified in 29 (22.8%) on ultrasound examination performed, on average 13.3 days after birth, combined with calyceal ectasia in 5 (3.9%) infants. At a postmenstrual age of 40 weeks, 18 infants (14.2%) had renal pelvis dilatation, 6 (5%) infants accompanied by a dilatation of the calyx. On the last follow-up performed when children were not older than 2 years old, renal pelvis dilatation had resolved to within normal limits in 23 (79%) infants while persisting in 6 (21%) infants; 1 mild, 3 moderate, and 2 severe pelvis dilatation. The median time-to-recovery of dilatation was 10.5 months (Kaplan-Meier curve), regardless of the severity of dilatation at birth. Based on receiver operating curve analysis, a cutoff diameter of renal dilatation at birth of 11.35 mm predicted persisting severe dilatation at the final follow-up (sensitivity 83.3%, specificity 82.6%).
CONCLUSION
Although premature infants with dilatation of mild severity were all recovered, some of those with moderate-to-severe dilatation progressed to hydronephrosis. Therefore careful follow-up of premature infants with renal pelvis dilatation is recommended.
MeSH Terms
Figure
Reference
-
1. Nguyen HT, Benson CB, Bromley B, Campbell JB, Chow J, Coleman B, et al. Multidisciplinary consensus on the classification of prenatal and postnatal urinary tract dilation (UTD classification system). J Pediatr Urol. 2014; 10:982–998.
Article2. Mami C, Paolata A, Palmara A, Marrone T, Berte LF, Marseglia L, et al. Outcome and management of isolated moderate renal pelvis dilatation detected at postnatal screening. Pediatr Nephrol. 2009; 24:2005–2008.
Article3. Scott JE, Wright B, Wilson G, Pearson IA, Matthews JN, Rose PG. Measuring the fetal kidney with ultrasonography. Br J Urol. 1995; 76:769–774.
Article4. Gunn TR, Mora JD, Pease P. Antenatal diagnosis of urinary tract abnormalities by ultrasonography after 28 weeks' gestation: incidence and outcome. Am J Obstet Gynecol. 1995; 172:479–486.
Article5. Herndon CD. Antenatal hydronephrosis: differential diagnosis, evaluation, and treatment options. ScientificWorldJournal. 2006; 6:2345–2365.
Article6. Nguyen HT, Herndon CD, Cooper C, Gatti J, Kirsch A, Kokorowski P, et al. The Society for Fetal Urology consensus statement on the evaluation and management of antenatal hydronephrosis. J Pediatr Urol. 2010; 6:212–231.
Article7. Duncan KA. Antenatal renal pelvic dilatation; the long-term outlook. Clin Radiol. 2007; 62:134–139.
Article8. Hothi DK, Wade AS, Gilbert R, Winyard PJ. Mild fetal renal pelvis dilatation: much ado about nothing? Clin J Am Soc Nephrol. 2009; 4:168–177.9. Grignon A, Filion R, Filiatrault D, Robitaille P, Homsy Y, Boutin H, et al. Urinary tract dilatation in utero: classification and clinical applications. Radiology. 1986; 160:645–647.
Article10. Ismaili K, Hall M, Donner C, Thomas D, Vermeylen D, Avni FE, et al. Results of systematic screening for minor degrees of fetal renal pelvis dilatation in an unselected population. Am J Obstet Gynecol. 2003; 188:242–246.
Article11. Cheng AM, Phan V, Geary DF, Rosenblum ND. Outcome of isolated antenatal hydronephrosis. Arch Pediatr Adolesc Med. 2004; 158:38–40.
Article12. Bouzada MC, Oliveira EA, Pereira AK, Leite HV, Rodrigues AM, Fagundes LA, et al. Diagnostic accuracy of fetal renal pelvis anteroposterior diameter as a predictor of uropathy: a prospective study. Ultrasound Obstet Gynecol. 2004; 24:745–749.
Article13. Masson P, De Luca G, Tapia N, Le Pommelet C, Es Sathi A, Touati K, et al. Postnatal investigation and outcome of isolated fetal renal pelvis dilatation. Arch Pediatr. 2009; 16:1103–1110.14. Onen A, Jayanthi VR, Koff SA. Long-term followup of prenatally detected severe bilateral newborn hydronephrosis initially managed nonoperatively. J Urol. 2002; 168:1118–1120.
Article15. Karnak I, Woo LL, Shah SN, Sirajuddin A, Ross JH. Results of a practical protocol for management of prenatally detected hydronephrosis due to ureteropelvic junction obstruction. Pediatr Surg Int. 2009; 25:61–67.
Article16. Bajpai M, Chandrasekharam VV. Nonoperative management of neonatal moderate to severe bilateral hydronephrosis. J Urol. 2002; 167:662–665.
Article17. Park YJ, Mun SJ, Bae CW, Lee BH, Kim JI. Post-natal outcome of fetal hydronephrosis detected with prenatal ultrasonography. J Korean Pediatr Soc. 2002; 45:1213–1218.18. Chen SY, Su YT, Wu CY. Nonobstructive dilation of urinary tract and later development of obstruction: report of one case. Pediatr Neonatol. 2010; 51:353–355.
Article19. Odibo AO, Marchiano D, Quinones JN, Riesch D, Egan JF, Macones GA. Mild pyelectasis: evaluating the relationship between gestational age and renal pelvic anterior-posterior diameter. Prenat Diagn. 2003; 23:824–827.
Article20. Policiano C, Djokovic D, Carvalho R, Monteiro C, Melo MA, Graça LM. Ultrasound antenatal detection of urinary tract anomalies in the last decade: outcome and prognosis. J Matern Fetal Neonatal Med. 2015; 28:959–963.
Article21. Chitty LS, Altman DG. Charts of fetal size: kidney and renal pelvis measurements. Prenat Diagn. 2003; 23:891–897.
Article22. Riccabona M. Assessment and management of newborn hydronephrosis. World J Urol. 2004; 22:73–78.
Article23. Arena S, Magno C, Montalto AS, Russo T, Mami C, Baldari S, et al. Long-term follow-up of neonatally diagnosed primary megaureter: rate and predictors of spontaneous resolution. Scand J Urol Nephrol. 2012; 46:201–207.
Article24. Ismaili K, Avni FE, Wissing KM, Hall M. Brussels Free University Perinatal Nephrology Study. Group Long-term clinical outcome of infants with mild and moderate fetal pyelectasis: validation of neonatal ultrasound as a screening tool to detect significant nephrouropathies. J Pediatr. 2004; 144:759–765.25. Dremsek PA, Gindl K, Voitl P, Strobl R, Hafner E, Geissler W, et al. Renal pyelectasis in fetuses and neonates: diagnostic value of renal pelvis diameter in pre- and postnatal sonographic screening. AJR Am J Roentgenol. 1997; 168:1017–1019.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Study of Prematurity and Low Birth Weight Infants
- Clinical and Statistical Observation for Low Birth Weight Infants
- Clinical and statistical observation for very low birth weight infants
- Clinical Evaluation of Postnatal Weight Gain in Premature and Low Birth Weight Infants
- Rehospitalization of Low-birth-weight Infants Who Were Discharged from NICU