Yonsei Med J.
2015 Jul;56(4):921-927. 10.3349/ymj.2015.56.4.921.
Association between Fibrinogen and Carotid Atherosclerosis According to Smoking Status in a Korean Male Population
- Affiliations
-
- 1Department of Public Health, Yonsei University Graduate School, Seoul, Korea.
- 2Department of Family Medicine, Seoul Medical Center, Seoul, Korea.
- 3Department of Medical Humanities and Social Medicines, Ajou University School of Medicine, Suwon, Korea.
- 4Department of Preventive Medicine, Yonsei University College of Medicine, Seoul, Korea. hckim@yuhs.ac
- 5Medical Affairs, Novartis Korea Oncology, Seoul, Korea.
- 6Yonsei Cardiovascular Center, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2366330
- DOI: http://doi.org/10.3349/ymj.2015.56.4.921
Abstract
- PURPOSE
Although inconsistent, reports have shown fibrinogen levels to be associated with atherosclerosis. Accordingly, since cigarette smoking is associated with increased levels of fibrinogen and atherosclerosis, it may also affect the association between fibrinogen and atherosclerosis. We investigated the associations between fibrinogen and carotid intima-media thickness (IMT) according to smoking status in a Korean male population.
MATERIALS AND METHODS
Plasma fibrinogen levels were measured in 277 men aged 40-87 years without a history of myocardial infarction or stroke. High-resolution B-mode ultrasonography was used to examine the common carotid arteries. IMT level was analyzed both as a continuous (IMT-max, maximum value; IMT-tpm, 3-point mean value) and categorical variable (higher IMT; presence of plaque). Serial linear and logistic regression models were employed to examine the association between fibrinogen and IMT according to smoking status.
RESULTS
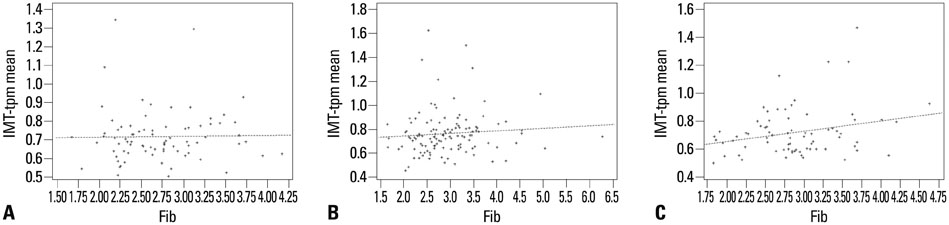
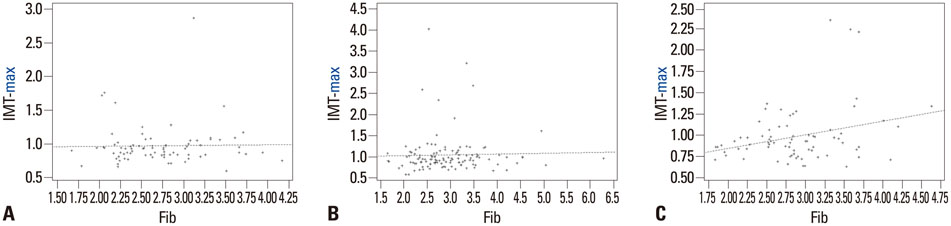
Fibrinogen levels were positively associated with IMT-max (standardized beta=0.25, p=0.021) and IMT-tpm (standardized beta=0.21, p=0.038), even after adjusting for age, body mass index, systolic blood pressure, fasting glucose, and total cholesterol to high-density lipoprotein cholesterol ratio in current smokers (n=75). No significant association between fibrinogen and IMT, however, was noted in former smokers (n=80) or nonsmokers (n=122). Adjusted odds ratios (95% confidence interval) for having plaque per one standard deviation higher fibrinogen level were 2.06 (1.09-3.89) for current smokers, 0.68 (0.43-1.10) for former smokers, and 1.06 (0.60-1.87) for nonsmokers.
CONCLUSION
Our findings suggest that cigarette smoking may modify the association between fibrinogen and carotid atherosclerosis. Further studies are required to confirm this finding in different populations.
Keyword
MeSH Terms
-
Adult
Aged
Aged, 80 and over
Asian Continental Ancestry Group/*statistics & numerical data
Atherosclerosis/*ultrasonography
Blood Pressure
Body Mass Index
Carotid Artery Diseases/*blood/epidemiology/ultrasonography
Carotid Artery, Common
*Carotid Intima-Media Thickness
Cholesterol/blood
Cholesterol, HDL
Cross-Sectional Studies
Fibrinogen/*analysis
Humans
Lipoproteins, HDL/blood
Logistic Models
Male
Middle Aged
Republic of Korea/epidemiology
Risk Factors
Sex Factors
Smoking/*adverse effects/blood/epidemiology
Surveys and Questionnaires
Cholesterol
Cholesterol, HDL
Lipoproteins, HDL
Fibrinogen
Figure
Reference
-
1. Fibrinogen Studies Collaboration. Danesh J, Lewington S, Thompson SG, Lowe GD, Collins R, et al. Plasma fibrinogen level and the risk of major cardiovascular diseases and nonvascular mortality: an individual participant meta-analysis. JAMA. 2005; 294:1799–1809.2. de Moerloose P, Boehlen F, Neerman-Arbez M. Fibrinogen and the risk of thrombosis. Semin Thromb Hemost. 2010; 36:7–17.
Article3. Green D, Foiles N, Chan C, Schreiner PJ, Liu K. Elevated fibrinogen levels and subsequent subclinical atherosclerosis: the CARDIA Study. Atherosclerosis. 2009; 202:623–631.
Article4. Páramo JA, Beloqui O, Roncal C, Benito A, Orbe J. Validation of plasma fibrinogen as a marker of carotid atherosclerosis in subjects free of clinical cardiovascular disease. Haematologica. 2004; 89:1226–1231.5. Grebe MT, Luu B, Sedding D, Heidt MC, Kemkes-Matthes B, Schaefer CA, et al. Fibrinogen promotes early atherosclerotic changes of the carotid artery in young, healthy adults. J Atheroscler Thromb. 2010; 17:1003–1008.
Article6. Green D, Chan C, Kang J, Liu K, Schreiner P, Jenny NS, et al. Longitudinal assessment of fibrinogen in relation to subclinical cardiovascular disease: the CARDIA study. J Thromb Haemost. 2010; 8:489–495.
Article7. Lorenz MW, Markus HS, Bots ML, Rosvall M, Sitzer M. Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis. Circulation. 2007; 115:459–467.
Article8. Hayashi S. Significance of plasma D-dimer in relation to the severity of atherosclerosis among patients evaluated by non-invasive indices of cardio-ankle vascular index and carotid intima-media thickness. Int J Hematol. 2010; 92:76–82.
Article9. Sekikawa A, Ueshima H, Kadowaki T, El-Saed A, Okamura T, Takamiya T, et al. Less subclinical atherosclerosis in Japanese men in Japan than in White men in the United States in the post-World War II birth cohort. Am J Epidemiol. 2007; 165:617–624.
Article10. Choi H, Cho DH, Shin HH, Park JB. Association of high sensitivity C-reactive protein with coronary heart disease prediction, but not with carotid atherosclerosis, in patients with hypertension. Circ J. 2004; 68:297–303.
Article11. Kannel WB, D'Agostino RB, Belanger AJ. Fibrinogen, cigarette smoking, and risk of cardiovascular disease: insights from the Framingham Study. Am Heart J. 1987; 113:1006–1010.
Article12. Meade TW, Imeson J, Stirling Y. Effects of changes in smoking and other characteristics on clotting factors and the risk of ischaemic heart disease. Lancet. 1987; 2:986–988.
Article13. Bazzano LA, He J, Muntner P, Vupputuri S, Whelton PK. Relationship between cigarette smoking and novel risk factors for cardiovascular disease in the United States. Ann Intern Med. 2003; 138:891–897.
Article14. Leone A. Smoking, haemostatic factors, and cardiovascular risk. Curr Pharm Des. 2007; 13:1661–1667.
Article15. Unverdorben M, von Holt K, Winkelmann BR. Smoking and atherosclerotic cardiovascular disease: part II: role of cigarette smoking in cardiovascular disease development. Biomark Med. 2009; 3:617–653.
Article16. Borissoff JI, Spronk HM, ten Cate H. The hemostatic system as a modulator of atherosclerosis. N Engl J Med. 2011; 364:1746–1760.
Article17. Ernst E. Fibrinogen as a cardiovascular risk factor--interrelationship with infections and inflammation. Eur Heart J. 1993; 14:Suppl K. 82–87.18. Woodward M, Lowe GD, Rumley A, Tunstall-Pedoe H. Fibrinogen as a risk factor for coronary heart disease and mortality in middle-aged men and women. The Scottish Heart Health Study. Eur Heart J. 1998; 19:55–62.
Article19. Kannel WB. Overview of hemostatic factors involved in atherosclerotic cardiovascular disease. Lipids. 2005; 40:1215–1220.
Article20. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972; 18:499–502.
Article21. Yanase T, Nasu S, Mukuta Y, Shimizu Y, Nishihara T, Okabe T, et al. Evaluation of a new carotid intima-media thickness measurement by B-mode ultrasonography using an innovative measurement software, intimascope. Am J Hypertens. 2006; 19:1206–1212.
Article22. Lemne C, Jogestrand T, de Faire U. Carotid intima-media thickness and plaque in borderline hypertension. Stroke. 1995; 26:34–39.
Article23. Castelli WP, Abbott RD, McNamara PM. Summary estimates of cholesterol used to predict coronary heart disease. Circulation. 1983; 67:730–734.
Article24. Chang HS, Kim HC, Ahn SV, Hur NW, Suh I. Impact of multiple cardiovascular risk factors on the carotid intima-media thickness in young adults: the Kangwha Study. J Prev Med Public Health. 2007; 40:411–417.
Article25. Kim HC, Kim DJ, Huh KB. Association between nonalcoholic fatty liver disease and carotid intima-media thickness according to the presence of metabolic syndrome. Atherosclerosis. 2009; 204:521–525.
Article26. Fowkes FG, Lee AJ, Lowe GD, Riemersma RA, Housley E. Inter-relationships of plasma fibrinogen, low-density lipoprotein cholesterol, cigarette smoking and the prevalence of cardiovascular disease. J Cardiovasc Risk. 1996; 3:307–311.
Article27. Tuut M, Hense HW. Smoking, other risk factors and fibrinogen levels. evidence of effect modification. Ann Epidemiol. 2001; 11:232–238.
Article28. Barua RS, Sy F, Srikanth S, Huang G, Javed U, Buhari C, et al. Effects of cigarette smoke exposure on clot dynamics and fibrin structure: an ex vivo investigation. Arterioscler Thromb Vasc Biol. 2010; 30:75–79.
Article29. Collet JP, Allali Y, Lesty C, Tanguy ML, Silvain J, Ankri A, et al. Altered fibrin architecture is associated with hypofibrinolysis and premature coronary atherothrombosis. Arterioscler Thromb Vasc Biol. 2006; 26:2567–2573.
Article30. Lord ST. Molecular mechanisms affecting fibrin structure and stability. Arterioscler Thromb Vasc Biol. 2011; 31:494–499.31. Yanbaeva DG, Dentener MA, Creutzberg EC, Wesseling G, Wouters EF. Systemic effects of smoking. Chest. 2007; 131:1557–1566.
Article32. Yarnell JW, Sweetnam PM, Rumley A, Lowe GD. Lifestyle and hemostatic risk factors for ischemic heart disease: the Caerphilly Study. Arterioscler Thromb Vasc Biol. 2000; 20:271–279.33. Kohler HP, Grant PJ. Plasminogen-activator inhibitor type 1 and coronary artery disease. N Engl J Med. 2000; 342:1792–1801.
Article34. Howard G, Burke GL, Szklo M, Tell GS, Eckfeldt J, Evans G, et al. Active and passive smoking are associated with increased carotid wall thickness. The Atherosclerosis Risk in Communities Study. Arch Intern Med. 1994; 154:1277–1282.
Article35. Ferrucci L, Corsi A, Lauretani F, Bandinelli S, Bartali B, Taub DD, et al. The origins of age-related proinflammatory state. Blood. 2005; 105:2294–2299.
Article36. Kramer A, Jansen AC, van Aalst-Cohen ES, Tanck MW, Kastelein JJ, Zwinderman AH. Relative risk for cardiovascular atherosclerotic events after smoking cessation: 6-9 years excess risk in individuals with familial hypercholesterolemia. BMC Public Health. 2006; 6:262.
Article37. Dobson AJ, Alexander HM, Heller RF, Lloyd DM. How soon after quitting smoking does risk of heart attack decline? J Clin Epidemiol. 1991; 44:1247–1253.
Article38. Hur NW, Kim HC, Nam CM, Jee SH, Lee HC, Suh I. Smoking cessation and risk of type 2 diabetes mellitus: Korea Medical Insurance Corporation Study. Eur J Cardiovasc Prev Rehabil. 2007; 14:244–249.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- High Sensitivity CRP, Fibrinogen and Homocysteine in Relation to Carotid Intima-media Thickness in Acute Ischemic Stroke
- Plasma Fibrinogen Level is Associated with Carotid Plaque Progression in Type 2 Diabetic Patients
- Carotid Atherosclerosis as a Marker of Atherosclerosis of the Thoracic Aorta in the Elderly
- Relationship between Carotid Atherosclerosis and Chlamydia Pneumoniae Seropositivity in Type 2 Diabetes
- Correlation between Intima-Media Thickness in Carotid Artery and the Extent of Coronary Atherosclerosis