Urogenit Tract Infect.
2016 Dec;11(3):97-102. 10.14777/uti.2016.11.3.97.
The Effect of Intrarectal Lidocaine Gel Instillation before Transrectal Ultrasound Guided Prostate Biopsy
- Affiliations
-
- 1Goldman Urology Clinic, Incheon, Korea.
- 2Department of Urology, National Police Hospital, Seoul, Korea. drmsk@korea.com
- KMID: 2366145
- DOI: http://doi.org/10.14777/uti.2016.11.3.97
Abstract
- PURPOSE
To compare pain induced by a transrectal ultrasound (TRUS)-guided prostate biopsy in men between using local lidocaine gel or plain lubricant.
MATERIALS AND METHODS
Between January and October of 2014, a total of 63 consecutive patients undergoing TRUS-guided prostate biopsy for elevated prostate-specific antigen (PSA) levels and/or a suspicious digital rectal examination were randomized to two groups: lidocaine group and control group. In the lidocaine group (n=31), patients received 20 ml of 2% lidocaine gel and betadine solution soaked gauze was administered via a transrectal route 10 minutes before the procedure. In the control group (n=32), 20 ml plain lubricant and betadine solution soaked gauze was administrated under the same condition. After the biopsy procedure, patients were asked to rate their pain perception on a 10-point visual analog scale (VAS) score.
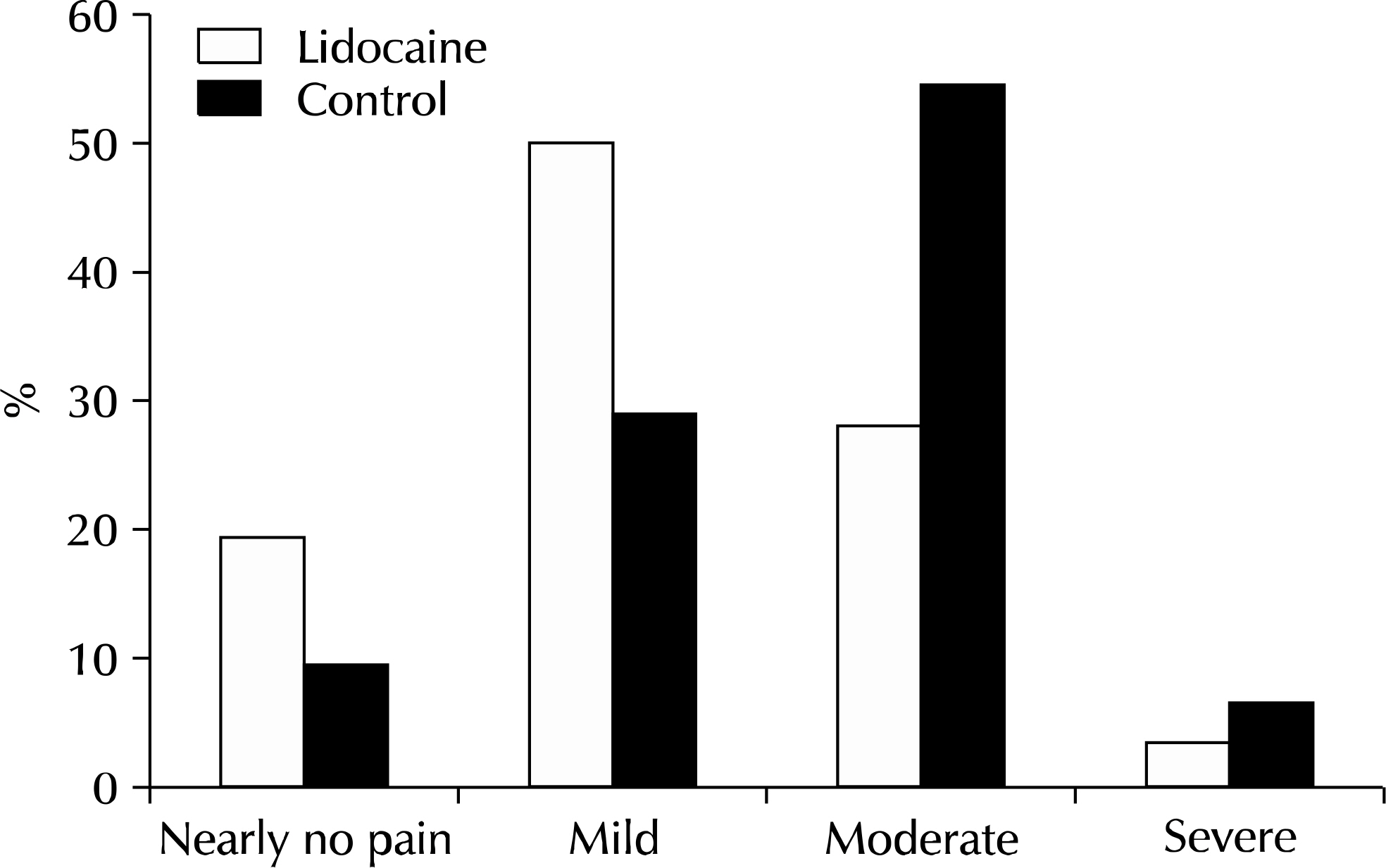
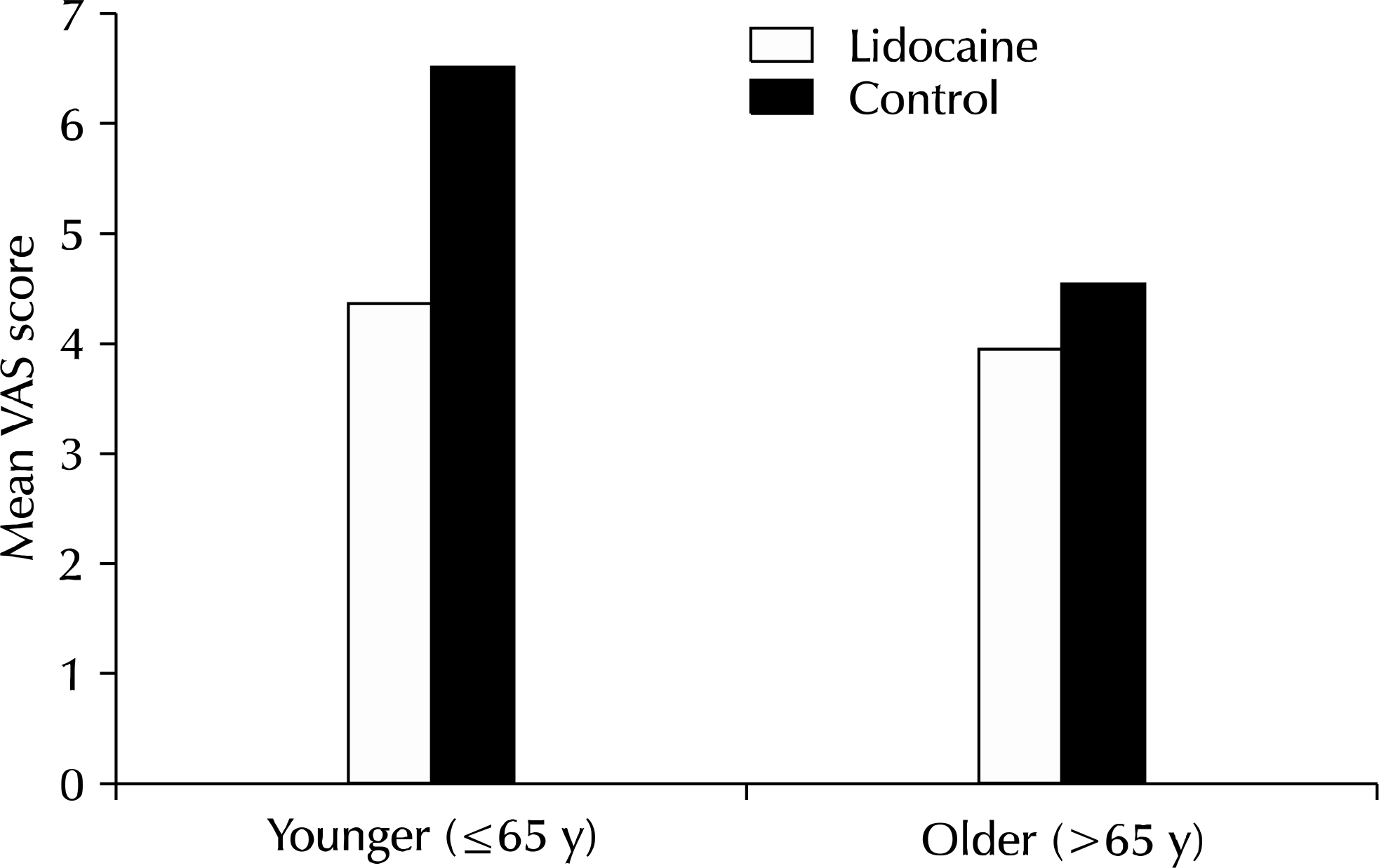
RESULTS
There was no statistically significant difference with the mean patient age, PSA, prostate volume, biopsy duration time between lidocaine group and control group. The mean pain score and number of patients with VAS ≥5 in the lidocaine group (4.14±2.0, 10) were significantly lower than those in the control group (5.78±2.3, 19). In younger men (≤65 years), pain was reported significantly less in the lidocaine group than in the control group. Complication rates were not different between the two groups.
CONCLUSIONS
Intrarectal lidocaine gel is a simple, safe, and efficacious for reducing pain and discomfort during the TRUS-guided prostate biopsy procedure. It appears to have an enhanced effect, especially in younger than in older men.
Keyword
MeSH Terms
Figure
Reference
-
1.Aus G., Hermansson CG., Hugosson J., Pedersen KV. Transrectal ultrasound examination of the prostate: complications and acceptance by patients. Br J Urol. 1993. 71:457–9.
Article2.Clements R., Aideyan OU., Griffiths GJ., Peeling WB. Side effects and patient acceptability of transrectal biopsy of the prostate. Clin Radiol. 1993. 47:125–6.
Article3.Collins GN., Lloyd SN., Hehir M., McKelvie GB. Multiple transrectal ultrasound-guided prostatic biopsies—true morbidity and patient acceptance. Br J Urol. 1993. 71:460–3.
Article4.Jones JS., Oder M., Zippe CD. Saturation prostate biopsy with periprostatic block can be performed in office. J Urol. 2002. 168:2108–10.
Article5.Walker AE., Schelvan C., Rockall AG., Rickards D., Kellett MJ. Does pericapsular lignocaine reduce pain during transrectal ultrasonography-guided biopsy of the prostate? BJU Int. 2002. 90:883–6.
Article6.Schostak M., Christoph F., Muller M., Heicappell R., Goessl G., Staehler M, et al. Optimizing local anesthesia during 10-core biopsy of the prostate. Urology. 2002. 60:253–7.
Article7.Issa MM., Bux S., Chun T., Petros JA., Labadia AJ., Anastasia K, et al. A randomized prospective trial of intrarectal lidocaine for pain control during transrectal prostate biopsy: the Emory University experience. J Urol. 2000. 164:397–9.
Article8.Saad F., Sabbagh R., McCormack M., Peloquin F. A prospective randomized trial comparing lidocaine and lubricating gel on pain level in patients undergoing transrectal ultrasound prostate biopsy. Can J Urol. 2002. 9:1592–4.9.Stirling BN., Shockley KF., Carothers GG., Maatman TJ. Comparison of local anesthesia techniques during transrectal ultrasound-guided biopsies. Urology. 2002. 60:89–92.
Article10.Rodriguez A., Kyriakou G., Leray E., Lobel B., Guille F. Prospective study comparing two methods of anaesthesia for prostate biopsies: apex periprostatic nerve block versus intrarectal lidocaine gel: review of the literature. Eur Urol. 2003. 44:195–200.
Article11.Ehrenstrom Reiz GM., Reiz SL. EMLA—a eutectic mixture of local anaesthetics for topical anaesthesia. Acta Anaesthesiol Scand. 1982. 26:596–8.12.Holst A., Evers H. Experimental studies of new topical anaesthetics on the oral mucosa. Swed Dent J. 1985. 9:185–91.13.Ohlsen L., Englesson S., Evers H. An anaesthetic lidocaine/prilocaine cream (EMLA) for epicutaneous application tested for cutting split skin grafts. Scand J Plast Reconstr Surg. 1985. 19:201–9.
Article14.Sonmez K., Demirogullari B., Ekingen G., Turkyilmaz Z., Karabulut R., Başaklar AC, et al. Randomized, placebo-controlled treatment of anal fissure by lidocaine, EMLA, and GTN in children. J Pediatr Surg. 2002. 37:1313–6.15.Wu CL., Carter HB., Naqibuddin M., Fleisher LA. Effect of local anesthetics on patient recovery after transrectal biopsy. Urology. 2001. 57:925–9.
Article16.Soloway MS., Obek C. Periprostatic local anesthesia before ultrasound guided prostate biopsy. J Urol. 2000. 163:172–3.
Article17.Zisman A., Leibovici D., Kleinmann J., Siegel YI., Lindner A. The impact of prostate biopsy on patient well-being: a prospective study of pain, anxiety and erectile dysfunction. J Urol. 2001. 165:445–54.18.Desgrandchamps F., Meria P., Irani J., Desgrippes A., Teillac P., Le Duc A. The rectal administration of lidocaine gel and tolerance of transrectal ultrasonography-guided biopsy of the prostate: a prospective randomized placebo-controlled study. BJU Int. 1999. 83:1007–9.
Article19.Institute for Clinical Systems Improvement (Work Group Leader Carns P, Mayo Clinic). Health care guideline: assessment and management of acute pain. Bloomington: ICSI Inc.;2002.20.Issa MM., Ritenour C., Greenberger M., Hollabaugh R Jr., Steiner M. The prostate anesthetic block for outpatient prostate surgery. World J Urol. 1998. 16:378–83.
Article21.Hollabaugh RS Jr., Dmochowski RR., Steiner MS. Neuroanatomy of the male rhabdosphincter. Urology. 1997. 49:426–34.
Article22.Hollabaugh RS Jr., Dmochowski RR., Kneib TG., Steiner MS. Preservation of putative continence nerves during radical retropubic prostatectomy leads to more rapid return of urinary continence. Urology. 1998. 51:960–7.
Article23.Moll F., Karenberg A., Rathert P. The historic interaction of urology and anaesthesia. De Historia Urol Eur. 2001. 8:73–94.24.Tammelin LE., Lofgren N. The action of anesthetics upon interfaces; on the mechanism of anesthesia. Acta Chem Scand. 1947. 1:871–83.
Article25.Djavan B., Waldert M., Zlotta A., Dobronski P., Seitz C., Remzi M, et al. Safety and morbidity of first and repeat transrectal ultrasound guided prostate needle biopsies: results of a prospective European prostate cancer detection study. J Urol. 2001. 166:856–60.
Article26.Rodriguez LV., Terris MK. Risks and complications of transrectal ultrasound guided prostate needle biopsy: a prospective study and review of the literature. J Urol. 1998. 160:2115–20.
Article27.Wall PD., Woolf CJ. Muscle but not cutaneous C-afferent input produces prolonged increases in the excitability of the flexion reflex in the rat. J Physiol. 1984. 356:443–58.
Article28.Mense S. Nociception from skeletal muscle in relation to clinical muscle pain. Pain. 1993. 54:241–89.
Article29.Edwards RR., Fillingim RB., Ness TJ. Age-related differences in endogenous pain modulation: a comparison of diffuse noxious inhibitory controls in healthy older and younger adults. Pain. 2003. 101:155–65.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Two Local Anesthestic Methods for Transrectal Ultrasound Guided Prostate Biopsy: Periprostatic Injection of Lidocaine and Rectal Instillation of Lidocaine Gel
- Analgesic Efficacy of Intrarectal Instillation of Lidocaine Gel prior to Transrectal Ultrasound Guided Prostate Biopsy: A Prospective Randomized Trial
- Effect of Sedation Anesthesia With Intravenous Propofol on Transrectal Ultrasound-Guided Prostate Biopsy Outcomes
- Combination of intrarectal heated lidocaine gel and periprostatic nerve block for pain control during transrectal ultrasound-guided prostate biopsy: A prospective randomized trial
- The Effects of Combination of Intrarectal Lidocaine-gel with Periprostatic Lidocaine Injection on the Pain Relief in Repeated Transrectal Prostate Biopsy