J Korean Soc Radiol.
2017 Jan;76(1):78-82. 10.3348/jksr.2017.76.1.78.
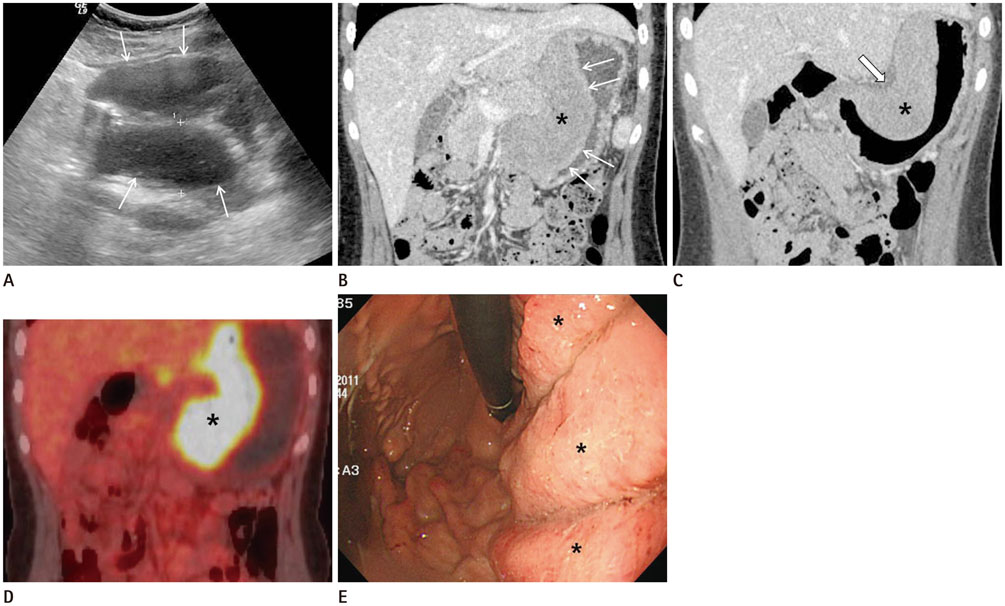
Imaging Findings of Isolated Myeloid Sarcoma of the Stomach in a Nonleukemic Child: A Case Report and Literature Review
- Affiliations
-
- 1Department of Radiology, Chonnam National University Hospital, Chonnam National University Medical School, Hwasun, Korea. sheo@jnu.ac.kr
- 2Department of Radiology, Chonnam National University Hwasun Hospital, Chonnam National University Medical School, Hwasun, Korea.
- KMID: 2365056
- DOI: http://doi.org/10.3348/jksr.2017.76.1.78
Abstract
- Myeloid sarcoma is an extramedullary solid neoplasm composed of myeloid precursor cells. This tumor usually occurs simultaneously with or following the onset of acute leukemia. Rarely, it can be the first manifestation of acute myeloid leukemia. The tumor can occur anywhere in the body. However, primary involvement of the stomach without evidence of leukemia is exceedingly rare, and to the best of our knowledge, imaging features of isolated myeloid sarcoma of the stomach have not been reported in children. This case illustrates the imaging appearances of isolated myeloid sarcoma that initially manifested as gastric submucosal wall thickening and discusses the differential diagnosis, in a 15-year-old girl without evidence of hematologic malignancy.
MeSH Terms
Figure
Reference
-
1. Meis JM, Butler JJ, Osborne BM, Manning JT. Granulocytic sarcoma in nonleukemic patients. Cancer. 1986; 58:2697–2709.2. Dusenbery KE, Howells WB, Arthur DC, Alonzo T, Lee JW, Kobrinsky N, et al. Extramedullary leukemia in children with newly diagnosed acute myeloid leukemia: a report from the Children’s Cancer Group. J Pediatr Hematol Oncol. 2003; 25:760–768.3. Guermazi A, Feger C, Rousselot P, Merad M, Benchaib N, Bourrier P, et al. Granulocytic sarcoma (chloroma): imaging findings in adults and children. AJR Am J Roentgenol. 2002; 178:319–325.4. Choi EK, Ha HK, Park SH, Lee SJ, Jung SE, Kim KW, et al. Granulocytic sarcoma of bowel: CT findings. Radiology. 2007; 243:752–759.5. Yilmaz AF, Saydam G, Sahin F, Baran Y. Granulocytic sarcoma: a systematic review. Am J Blood Res. 2013; 3:265–270.6. Huang XL, Tao J, Li JZ, Chen XL, Chen JN, Shao CK, et al. Gastric myeloid sarcoma without acute myeloblastic leukemia. World J Gastroenterol. 2015; 21:2242–2248.7. Toma P, Granata C, Rossi A, Garaventa A. Multimodality imaging of Hodgkin disease and non-Hodgkin lymphomas in children. Radiographics. 2007; 27:1335–1354.8. Patnana M, Sevrukov AB, Elsayes KM, Viswanathan C, Lubner M, Menias CO. Inflammatory pseudotumor: the great mimicker. AJR Am J Roentgenol. 2012; 198:W217–W227.9. Levy AD, Remotti HE, Thompson WM, Sobin LH, Miettinen M. Gastrointestinal stromal tumors: radiologic features with pathologic correlation. Radiographics. 2003; 23:283–304. 456quiz 532.10. Kim SJ, Kim WS, Cheon JE, Shin SM, Youn BJ, Kim IO, et al. Inflammatory myofibroblastic tumors of the abdomen as mimickers of malignancy: imaging features in nine children. AJR Am J Roentgenol. 2009; 193:1419–1424.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Isolated Granulocytic Sarcoma of the Ovary in Nonleukemic Patients
- Isolated Myeloid Sarcoma in the Nasal Cavity Without Bone Marrow Involvement in a 5-Year-Old Child
- Collision Tumor Composed of a Granulocytic Sarcoma and an Adenocarcinoma of the Stomach: A Case Report
- Intraparenchymal Myeloid Sarcoma and Subsequent Spinal Myeloid Sarcoma for Acute Myeloblastic Leukemia
- Nonleukemic Granulocytic Sarcoma of the Ileum: A Case Report