J Clin Neurol.
2017 Jan;13(1):32-37. 10.3988/jcn.2017.13.1.32.
Analysis of Risk Factors for Cerebral Microinfarcts after Carotid Endarterectomy and the Relevance of Delayed Cerebral Infarction
- Affiliations
-
- 1Department of Surgery, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea. twkwon2@amc.seoul.kr
- 2Department of Neurology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea.
- KMID: 2364895
- DOI: http://doi.org/10.3988/jcn.2017.13.1.32
Abstract
- BACKGROUND AND PURPOSE
Carotid endarterectomy (CEA) is performed to prevent cerebral infarction, but a common side effect is cerebral microinfarcts. This study aimed to identify the variables related to the production of microinfarcts during CEA as well as determine their association with delayed postoperative infarction.
METHODS
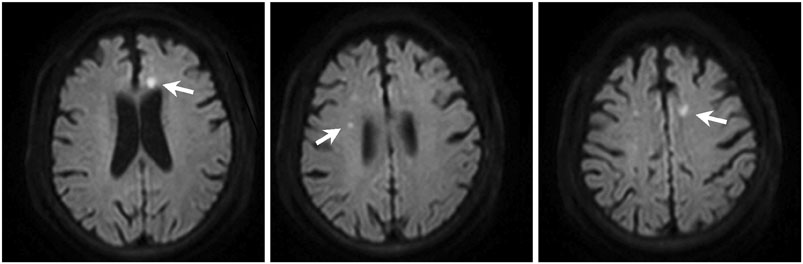
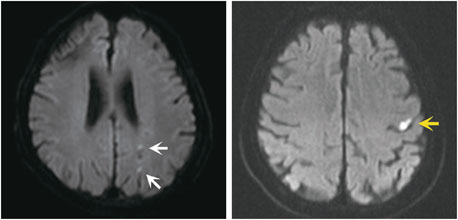
This was a retrospective review of data collected prospectively from 548 patients who underwent CEA. The clinical characteristics of the patients and the incidence rates and causes of microinfarcts were analyzed. Microinfarcts were diagnosed by diffusion-weighted magnetic resonance imaging. The presence of delayed postoperative infarction was compared between microinfarct-positive and microinfarct-negative groups.
RESULTS
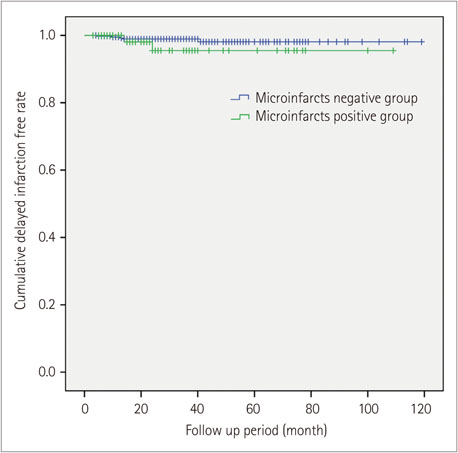
In total, 76 (13.86%) patients were diagnosed with microinfarcts. Preoperative neurological symptoms were significantly related to the incidence of microinfarcts [odds ratio (OR)=2.93, 95% confidence interval (CI)=1.72-5.00, p<0.001]. Shunt insertion during CEA was the only significant procedure-related risk factor (OR=1.42, 95% CI=1.00-2.19, p=0.05). The presence of microinfarcts did not significantly increase the incidence of delayed postoperative infarction (p=0.204).
CONCLUSIONS
In the present study, risk factors for microinfarcts after CEA included preoperative symptoms and intraoperative shunt insertion. Microinfarcts were not associated with delayed postoperative infarction.
MeSH Terms
Figure
Reference
-
1. North American Symptomatic Carotid Endarterectomy Trial Collaborators. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med. 1991; 325:445–453.2. Halliday A, Mansfield A, Marro J, Peto C, Peto R, Potter J, et al. Prevention of disabling and fatal strokes by successful carotid endarterectomy in patients without recent neurological symptoms: randomised controlled trial. Lancet. 2004; 363:1491–1502.
Article3. Rothwell PM, Gutnikov SA, Warlow CP. European Carotid Surgery Trialist's Collaboration. Reanalysis of the final results of the European Carotid Surgery Trial. Stroke. 2003; 34:514–523.
Article4. Gupta N, Corriere MA, Dodson TF, Chaikof EL, Beaulieu RJ, Reeves JG, et al. The incidence of microemboli to the brain is less with endarterectomy than with percutaneous revascularization with distal filters or flow reversal. J Vasc Surg. 2011; 53:316–322.
Article5. Lopez OL, Jagust WJ, Dulberg C, Becker JT, DeKosky ST, Fitzpatrick A, et al. Risk factors for mild cognitive impairment in the Cardiovascular Health Study Cognition Study: part 2. Arch Neurol. 2003; 60:1394–1399.
Article6. Yamashita H, Fujikawa T, Takami H, Yanai I, Okamoto Y, Morinobu S, et al. Long-term prognosis of patients with major depression and silent cerebral infarction. Neuropsychobiology. 2010; 62:177–181.
Article7. Wilson TJ, Pandey AS, Stetler WR Jr, Davis MC, Giles DA, Chaudhary N, et al. Dual antiplatelet therapy plus postoperative heparin and dextran is safe and effective for reducing risk of embolic stroke during aneurysm coiling. Acta Neurochir (Wien). 2014; 156:855–859.
Article8. Kuliha M, Roubec M, Procházka V, Jonszta T, Hrbáč T, Havelka J, et al. Randomized clinical trial comparing neurological outcomes after carotid endarterectomy or stenting. Br J Surg. 2015; 102:194–201.
Article9. Stork JL, Levi CR, Chambers BR, Abbott AL, Donnan GA. Possible determinants of early microembolism after carotid endarterectomy. Stroke. 2002; 33:2082–2085.
Article10. Levi CR, Roberts AK, Fell G, Hoare MC, Royle JP, Chan A, et al. Transcranial Doppler microembolus detection in the identification of patients at high risk of perioperative stroke. Eur J Vasc Endovasc Surg. 1997; 14:170–176.
Article11. King A, Markus HS. Doppler embolic signals in cerebrovascular disease and prediction of stroke risk: a systematic review and meta-analysis. Stroke. 2009; 40:3711–3717.
Article12. Mantese VA, Timaran CH, Chiu D, Begg RJ, Brott TG. CREST Investigators. The Carotid Revascularization Endarterectomy versus Stenting Trial (CREST): stenting versus carotid endarterectomy for carotid disease. Stroke. 2010; 41:10 Suppl. S31–S34.13. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial TOAST Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993; 24:35–41.
Article14. Gaunt ME, Brown L, Hartshorne T, Bell PR, Naylor AR. Unstable carotid plaques: preoperative identification and association with intraoperative embolisation detected by transcranial Doppler. Eur J Vasc Endovasc Surg. 1996; 11:78–82.
Article15. Shin S, Kwon TW, Cho YP, Shin JH, Yi A, Kim H, et al. Preoperative magnetic resonance angiography as a predictive test for cerebral ischemia during carotid endarterectomy. World J Surg. 2013; 37:663–670.
Article16. Palombo G, Faraglia V, Stella N, Giugni E, Bozzao A, Taurino M. Late evaluation of silent cerebral ischemia detected by diffusion-weighted MR imaging after filter-protected carotid artery stenting. AJNR Am J Neuroradiol. 2008; 29:1340–1343.
Article17. Vermeer SE, Prins ND, den Heijer T, Hofman A, Koudstaal PJ, Breteler MM. Silent brain infarcts and the risk of dementia and cognitive decline. N Engl J Med. 2003; 348:1215–1222.
Article18. Vermeer SE, Hollander M, van Dijk EJ, Hofman A, Koudstaal PJ, Breteler MM. Rotterdam Scan Study. Silent brain infarcts and white matter lesions increase stroke risk in the general population: the Rotterdam Scan Study. Stroke. 2003; 34:1126–1129.
Article19. Wolf O, Heider P, Heinz M, Poppert H, Sander D, Greil O, et al. Microembolic signals detected by transcranial Doppler sonography during carotid endarterectomy and correlation with serial diffusion-weighted imaging. Stroke. 2004; 35:e373–e375.
Article20. Levi CR, O'Malley HM, Fell G, Roberts AK, Hoare MC, Royle JP, et al. Transcranial Doppler detected cerebral microembolism following carotid endarterectomy. High microembolic signal loads predict postoperative cerebral ischaemia. Brain. 1997; 120(Pt 4):621–629.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cerebral Oxygen Saturation Monitoring during Carotid Endarterectomy: A case report
- Hyperacute hyperperfusion intracerebral hemorrhage complicating carotid endarterectomy: A case report
- Endovascular Treatment of Occlusive Cerebrovascular Diseases
- Anesthetic Management of Carotid Endarterectomy under EEG and SEP Monitoring
- Relationship between Carotid Artery Plaque Measured by Ultrasound and Cerebral infarction in Patients with Non-insulin Dependent Diabetes