Blood Res.
2016 Dec;51(4):217-219. 10.5045/br.2016.51.4.217.
Copper deficiency mimicking myelodysplastic syndrome
- Affiliations
-
- 1Laboratory of Clinical-Chemistry, Hematology and Microbiology, ASST Valle Olona, Gallarate Hospital, Varese, Italy.
- KMID: 2364308
- DOI: http://doi.org/10.5045/br.2016.51.4.217
Abstract
- No abstract available.
MeSH Terms
Figure
Reference
-
1. Halfdanarson TR, Kumar N, Li CY, Phyliky RL, Hogan WJ. Hematological manifestations of copper deficiency: a retrospective review. Eur J Haematol. 2008; 80:523–531. PMID: 18284630.
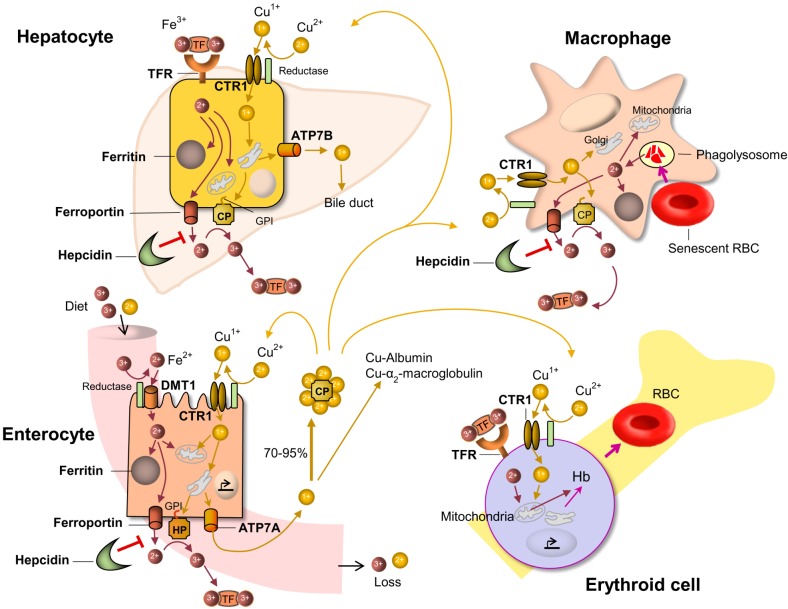
Article2. Collins JF, Prohaska JR, Knutson MD. Medtabolic crossroads of iron and copper. Nutr Rev. 2010; 68:133–147. PMID: 20384844.3. Klevay LM. “Myelodysplasia,” myeloneuropathy, and copper deficiency. Mayo Clin Proc. 2006; 81:132.
Article4. Green R. Anemias beyond B12 and iron deficiency: the buzz about other B's, elementary, and nonelementary problems. Hematology Am Soc Hematol Educ Program. 2012; 2012:492–498. PMID: 23233624.
Article5. Lazarchick J. Update on anemia and neutropenia in copper deficiency. Curr Opin Hematol. 2012; 19:58–60. PMID: 22080848.
Article6. Gregg XT, Reddy V, Prchal JT. Copper deficiency masquerading as myelodysplastic syndrome. Blood. 2002; 100:1493–1495. PMID: 12149237.
Article7. Simon SR, Branda RF, Tindle BF, Burns SL. Copper deficiency and sideroblastic anemia associated with zinc ingestion. Am J Hematol. 1988; 28:181–183. PMID: 3407636.
Article8. D'Angelo G. Plasma cell and iron granules. Haematologica. 1996; 81:588. PMID: 9009447.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Azathioprine-induced Myelodysplasia Mimicking Myelodysplastic Syndrome
- Sweet's Syndrome with Myelodysplastic Syndrome Progressing to Acute Myelogenous Leukemia
- Classifications and prognostic scoring systems in myelodysplastic syndrome
- Micronutrient Deficiency Syndrome: Zinc, Copper and Selenium
- Hair Heavy Metal Contents in Mentally Retarded Children IV: In Association with Copper