World J Mens Health.
2016 Dec;34(3):200-208. 10.5534/wjmh.2016.34.3.200.
Lower Urinary Tract Symptoms: Prevalence, Perceptions, and Healthcare-Seeking Behavior amongst Nigerian Men
- Affiliations
-
- 1Department of Surgery, College of Medicine of University of Lagos and Lagos University Teaching Hospital, Lagos, Nigeria. rojewola@unilag.edu.ng rwaleojewola@ yahoo.com
- 2Department of Community Health and Primary Care, College of Medicine of University of Lagos and Lagos University Teaching Hospital, Lagos, Nigeria.
- 3Department of Paediatrics, Ekiti State University & Ekiti State University Teaching Hospital, Ado-Ekiti, Nigeria.
- KMID: 2364203
- DOI: http://doi.org/10.5534/wjmh.2016.34.3.200
Abstract
- PURPOSE
The aim of this study was to determine the prevalence of lower urinary tract symptoms (LUTS) and the factors influencing the healthcare-seeking behavior of men with LUTS.
MATERIALS AND METHODS
A cross-sectional survey was performed of 658 men selected using multi-staged sampling techniques. They were interviewed about LUTS and their healthcare-seeking behavior. The data were analysed using PASW Statistics ver. 18. Associations between specific factors and healthcare-seeking behavior were examined using the chi-square and Fisher exact tests.
RESULTS
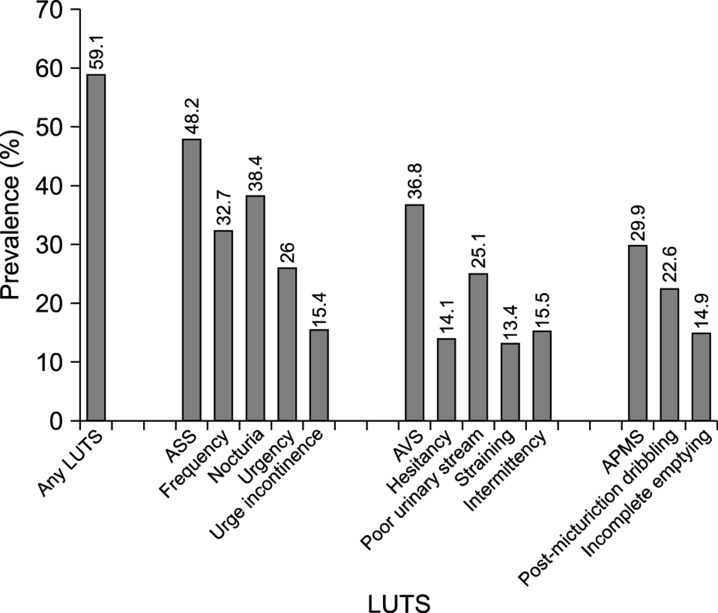
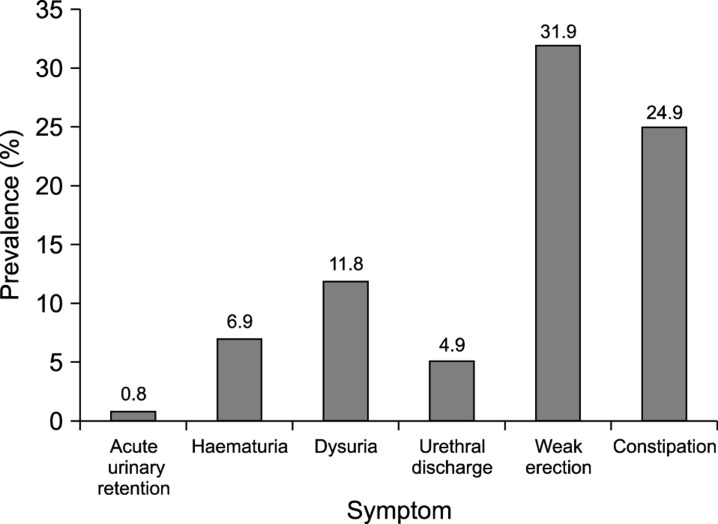
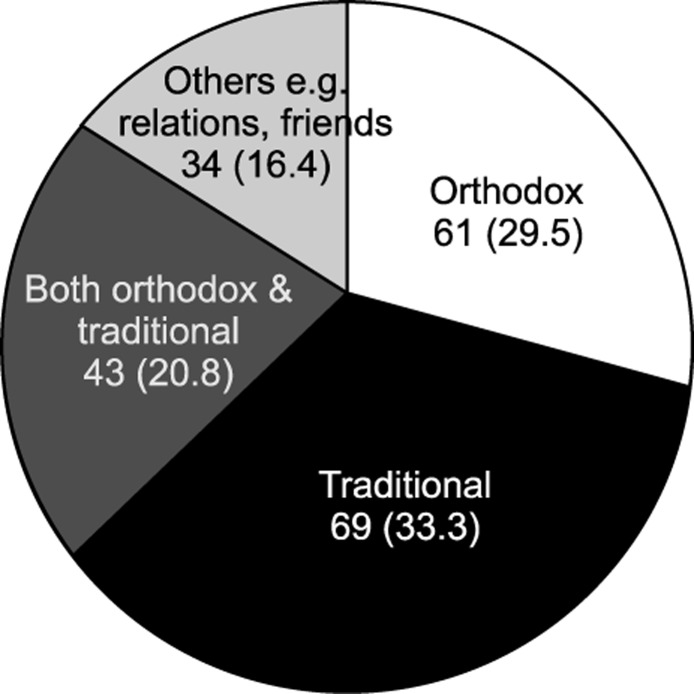
The overall prevalence of LUTS was 59.1%. Storage symptoms (48.2%) were more prevalent than voiding (36.8%) or post-micturition (29.9%) symptoms. Approximately a quarter (25.5%) had a poor quality of life (QoL) score. The average duration of symptoms before seeking help was 3.4 years. Almost half (46.8%) of the men with LUTS had never sought help. Perceptions of LUTS as an inevitable part of ageing, subjective feelings of wellness, financial constraints, and fear of surgery were the most common reasons for not seeking help. The most common reasons for seeking help were to moderate-severe symptoms, impaired QoL, and fear of cancer. Severe LUTS, impaired QoL, and the concomitant presence of erectile dysfunction, dysuria, or haematuria were clinical factors that positively influenced healthcare-seeking behavior.
CONCLUSIONS
In this population-based study, we found that the prevalence of LUTS was very high amongst adult males. However, only about half of these men sought medical attention. Their healthcare-seeking behavior was influenced by severity of symptoms, QoL scores, and socio-demographic factors such as educational status.
MeSH Terms
Figure
Cited by 1 articles
-
Factors Influencing Health Information Orientation in Middle-aged Community-dwelling
Jae Lan Shim, Youn-Jung Son
Korean J Health Promot. 2017;17(1):38-46. doi: 10.15384/kjhp.2017.17.1.38.
Reference
-
1. Jacobsen SJ, Guess HA, Panser L, Girman CJ, Chute CG, Oesterling JE, et al. A population-based study of health care-seeking behavior for treatment of urinary symptoms. The Olmsted County study of urinary symptoms and health status among men. Arch Fam Med. 1993; 2:729–735. PMID: 8111497.
Article2. Hunter DJ, Berra-Unamuno A. Treatment-seeking behaviour and stated preferences for prostatectomy in Spanish men with lower urinary tract symptoms. Br J Urol. 1997; 79:742–748. PMID: 9158513.
Article3. Girman CJ, Jacobsen SJ, Tsukamoto T, Richard F, Garraway WM, Sagnier PP, et al. Health-related quality of life associated with lower urinary tract symptoms in four countries. Urology. 1998; 51:428–436. PMID: 9510348.
Article4. Sarma AV, Wei JT, Jacobson DJ, Dunn RL, Roberts RO, Girman CJ, et al. Comparison of lower urinary tract symptom severity and associated bother between community-dwelling black and white men: the Olmsted County study of urinary symptoms and health status and the flint men's health study. Urology. 2003; 61:1086–1091. PMID: 12809866.
Article5. Ladha A, Khan RS, Malik AA, Khan SF, Khan B, Khan IN, et al. The health seeking behaviour of elderly population in a poor-urban community of Karachi, Pakistan. J Pak Med Assoc. 2009; 59:89–92. PMID: 19260571.6. Tinuade O, Iyabo RA, Durotoye O. Health-care-seeking behaviour for childhood illnesses in a resource-poor setting. J Paediatr Child Health. 2010; 46:238–242. PMID: 20337870.
Article7. Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. 2006; 50:1306–1314. discussion 1314-5. PMID: 17049716.
Article8. Boyle P, Robertson C, Mazzetta C, Keech M, Hobbs FD, Fourcade R, et al. The prevalence of male urinary incontinence in four centres: the UREPIK study. BJU Int. 2003; 92:943–947. PMID: 14632852.
Article9. Lee YS, Lee KS, Jung JH, Han DH, Oh SJ, Seo JT, et al. Prevalence of overactive bladder, urinary incontinence, and lower urinary tract symptoms: results of Korean EPIC study. World J Urol. 2011; 29:185–190. PMID: 19898824.
Article10. Kim TH, Han DH, Lee KS. The prevalence of lower urinary tract symptoms in Korean men aged 40 years or older: a population-based survey. Int Neurourol J. 2014; 18:126–132. PMID: 25279239.
Article11. Huh JS, Kim YJ, Kim SD. Prevalence of benign prostatic hyperplasia on Jeju Island: analysis from a cross-sectional community-based survey. World J Mens Health. 2012; 30:131–137. PMID: 23596600.
Article12. Cunningham-Burley S, Allbutt H, Garraway WM, Lee AJ, Russell EB. Perceptions of urinary symptoms and healthcare-seeking behaviour amongst men aged 40-79 years. Br J Gen Pract. 1996; 46:349–352. PMID: 8983253.13. Lee E, Yoo KY, Kim Y, Shin Y, Lee C. Prevalence of lower urinary tract symptoms in Korean men in a community-based study. Eur Urol. 1998; 33:17–21. PMID: 9471036.
Article14. Sarma AV, Burke JP, Jacobson DJ, McGree ME, St. Sauver J, Girman CJ, et al. Associations between diabetes and clinical markers of benign prostatic hyperplasia among community-dwelling Black and White men. Diabetes Care. 2008; 31:476–482. PMID: 18071006.
Article15. Lee EH, Chun KH, Lee Y. Benign prostatic hyperplasia in community-dwelling elderly in Korea. J Korean Acad Nurs. 2005; 35:1508–1513.
Article16. Sarma AV, Wallner L, Jacobsen SJ, Dunn RL, Wei JT. Health seeking behavior for lower urinary tract symptoms in black men. J Urol. 2008; 180:227–232. PMID: 18499182.
Article17. Emberton M, Marberger M, de la Rosette J. Understanding patient and physician perceptions of benign prostatic hyperplasia in Europe: the Prostate Research on Behaviour and Education (PROBE) Survey. Int J Clin Pract. 2008; 62:18–26. PMID: 18028388.
Article18. Kim HH, Kong KA, Lee HJ, Yoon H, Lee BE, Moon OR, et al. Relationship of socioeconomic factors with medical utilization for lower urinary tract symptoms and benign prostatic hyperplasia in a South Korean community. J Prev Med Public Health. 2006; 39:141–148. PMID: 16615269.19. Olapade-Olaopa EO, Onawola KA. Challenges for urology in sub-Saharan Africa in 2006. J Mens Health Gend. 2006; 3:109–116.
Article20. Opoku SY, Benwell M, Yarney J. Knowledge, attitudes, beliefs, behaviour and breast cancer screening practices in Ghana, West Africa. Pan Afr Med J. 2012; 11:28. PMID: 22514762.21. Chijioke A, Makusidi AM, Rafiu MO. Factors influencing hemodialysis and outcome in severe acute renal failure from Ilorin, Nigeria. Saudi J Kidney Dis Transpl. 2012; 23:391–396. PMID: 22382247.22. Williams DL, Tortu S, Thomson J. Factors associated with delays to diagnosis and treatment of breast cancer in women in a Louisiana urban safety net hospital. Women Health. 2010; 50:705–718. PMID: 21170814.
Article23. Onwujekwe OE, Uzochukwu BS, Obikeze EN, Okoronkwo I, Ochonma OG, Onoka CA, et al. Investigating determinants of out-of-pocket spending and strategies for coping with payments for healthcare in southeast Nigeria. BMC Health Serv Res. 2010; 10:67. PMID: 20233454.
Article24. Onwujekwe O, Hanson K, Ichoku H, Uzochukwu B. Financing incidence analysis of household out-of-pocket spending for healthcare: getting more health for money in Nigeria. Int J Health Plann Manage. 2014; 29:e174–e185. PMID: 23390079.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lower Urinary Tract Symptoms: Prevalence and Factors Associated with Help-Seeking in Male Primary Care Attendees
- The Urinary Tract Microbiome in Male Genitourinary Diseases: Focusing on Benign Prostate Hyperplasia and Lower Urinary Tract Symptoms
- Sociodemographic Factors Related to Lower Urinary Tract Symptoms in Men: A Korean Community Health Survey
- Prevalence, Risk Factors, Quality of Life, and Health-Care Seeking Behaviors of Female Urinary Incontinence: Results From the 4th Korean National Health and Nutrition Examination Survey VI (2007-2009)
- The Prevalence of Lower Urinary Tract Symptoms in Korean Men Aged 40 Years or Older: A Population-Based Survey