Clin Orthop Surg.
2016 Mar;8(1):65-70. 10.4055/cios.2016.8.1.65.
Lumbar Lordosis of Spinal Stenosis Patients during Intraoperative Prone Positioning
- Affiliations
-
- 1Department of Orthopaedic Surgery, Gwangmyeong Sungae Hospital, Gwangmyeong, Korea. java5885@gmail.com
- 2Department of Orthopaedic Surgery, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2363947
- DOI: http://doi.org/10.4055/cios.2016.8.1.65
Abstract
- BACKGROUND
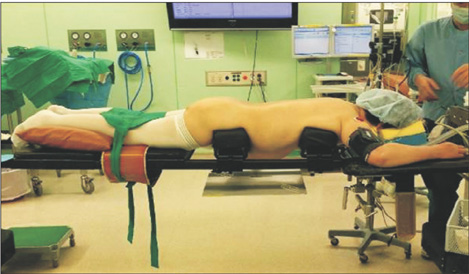
To evaluate the effect of spondylolisthesis on lumbar lordosis on the OSI (Jackson; Orthopaedic Systems Inc.) frame. Restoration of lumbar lordosis is important for maintaining sagittal balance. Physiologic lumbar lordosis has to be gained by intraoperative prone positioning with a hip extension and posterior instrumentation technique. There are some debates about changing lumbar lordosis on the OSI frame after an intraoperative prone position. We evaluated the effect of spondylolisthesis on lumbar lordosis after an intraoperative prone position.
METHODS
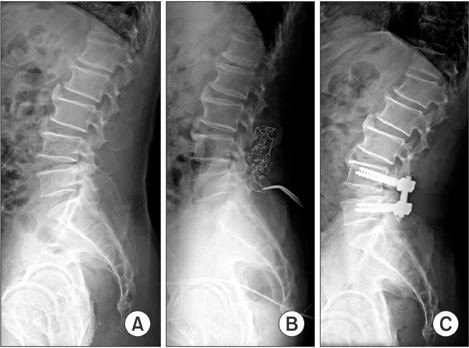
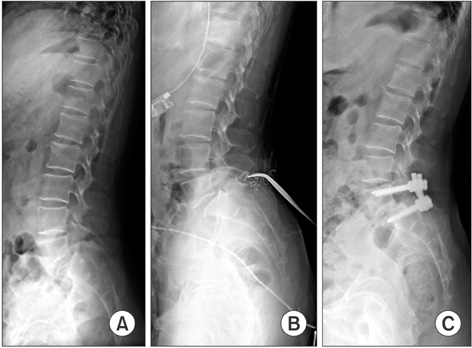
Sixty-seven patients, who underwent spinal fusion at the Department of Orthopaedic Surgery of Gwangmyeong Sungae Hospital between May 2007 and February 2012, were included in this study. The study compared lumbar lordosis on preoperative upright, intraoperative prone and postoperative upright lateral X-rays between the simple stenosis (SS) group and spondylolisthesis group. The average age of patients was 67.86 years old. The average preoperative lordosis was 43.5degrees (+/- 14.9degrees), average intraoperative lordosis was 48.8degrees (+/- 13.2degrees), average postoperative lordosis was 46.5degrees (+/- 16.1degrees) and the average change on the frame was 5.3degrees (+/- 10.6degrees).
RESULTS
Among all patients, 24 patients were diagnosed with simple spinal stenosis, 43 patients with spondylolisthesis (29 degenerative spondylolisthesis and 14 isthmic spondylolisthesis). Between the SS group and spondylolisthesis group, preoperative lordosis, intraoperative lordosis and postoperative lordosis were significantly larger in the spondylolisthesis group. The ratio of patients with increased lordosis on the OSI frame compared to preoperative lordosis was significantly higher in the spondylolisthesis group. The risk of increased lordosis on frame was significantly higher in the spondylolisthesis group (odds ratio, 3.325; 95% confidence interval, 1.101 to 10.039; p = 0.033).
CONCLUSIONS
Intraoperative lumbar lordosis on the OSI frame with a prone position was larger in the SS patients than the spondylolisthesis patients, which also produced a larger postoperative lordosis angle after posterior spinal fusion surgery. An increase in lumbar lordosis on the OSI frame should be considered during posterior spinal fusion surgery, especially in spondylolisthesis patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Lenke LG. Sagittal balance. J Neurosurg Spine. 2014; 20(5):512.2. Jean L. Influence of age and sagittal balance of the spine on the value of the pelvic incidence. Eur Spine J. 2014; 23(7):1394–1399.
Article3. Baghdadi YM, Larson AN, Dekutoski MB, et al. Sagittal balance and spinopelvic parameters after lateral lumbar interbody fusion for degenerative scoliosis: a case-control study. Spine (Phila Pa 1976). 2014; 39(3):E166–E173.4. Barrey C, Roussouly P, Le Huec JC, D'Acunzi G, Perrin G. Compensatory mechanisms contributing to keep the sagittal balance of the spine. Eur Spine J. 2013; 22:Suppl 6. S834–S841.
Article5. Galbusera F, Wilke HJ, Brayda-Bruno M, Costa F, Fornari M. Influence of sagittal balance on spinal lumbar loads: a numerical approach. Clin Biomech (Bristol, Avon). 2013; 28(4):370–377.
Article6. Johnson RD, Valore A, Villaminar A, Comisso M, Balsano M. Sagittal balance and pelvic parameters: a paradigm shift in spinal surgery. J Clin Neurosci. 2013; 20(2):191–196.
Article7. Morvan G, Mathieu P, Vuillemin V, et al. Standardized way for imaging of the sagittal spinal balance. Eur Spine J. 2011; 20:Suppl 5. 602–608.
Article8. Aebi M. Sagittal balance of the spine: consequences for the treatment of the degenerative spine. Eur Spine J. 2011; 20:Suppl 5. 555.
Article9. Labelle H, Mac-Thiong JM, Roussouly P. Spino-pelvic sagittal balance of spondylolisthesis: a review and classification. Eur Spine J. 2011; 20:Suppl 5. 641–646.
Article10. Angevine PD, Bridwell KH. Sagittal imbalance. Neurosurg Clin N Am. 2006; 17(3):353–363.
Article11. Mathias M, Rougier PR. In healthy subjects, the sitting position can be used to validate the postural effects induced by wearing a lumbar lordosis brace. Ann Phys Rehabil Med. 2010; 53(8):511–519.
Article12. Jang JS, Lee SH, Min JH, Maeng DH. Influence of lumbar lordosis restoration on thoracic curve and sagittal position in lumbar degenerative kyphosis patients. Spine (Phila Pa 1976). 2009; 34(3):280–284.
Article13. Lee JH, Lee JH, Yoon KS, Kang SB, Jo CH. Effect of intraoperative position used in posterior lumbar interbody fusion on the maintenance of lumbar lordosis. J Neurosurg Spine. 2008; 8(3):263–270.
Article14. Benfanti PL, Geissele AE. The effect of intraoperative hip position on maintenance of lumbar lordosis: a radiographic study of anesthetized patients and unanesthetized volunteers on the Wilson frame. Spine (Phila Pa 1976). 1997; 22(19):2299–2303.
Article15. Levine D, Whittle MW. The effects of pelvic movement on lumbar lordosis in the standing position. J Orthop Sports Phys Ther. 1996; 24(3):130–135.
Article16. Peterson MD, Nelson LM, McManus AC, Jackson RP. The effect of operative position on lumbar lordosis: a radiographic study of patients under anesthesia in the prone and 90-90 positions. Spine (Phila Pa 1976). 1995; 20(12):1419–1424.17. Bundy J, Hernandez T, Zhou H, Chutkan N. The effect of body mass index on lumbar lordosis on the Mizuho OSI Jackson spinal table. Evid Based Spine Care J. 2010; 1(1):35–40.
Article18. Harimaya K, Lenke LG, Mishiro T, Bridwell KH, Koester LA, Sides BA. Increasing lumbar lordosis of adult spinal deformity patients via intraoperative prone positioning. Spine (Phila Pa 1976). 2009; 34(22):2406–2412.
Article19. Wang TP, Zheng ZM, Liu H, Zhang KB, Wang H. Correlation of adult spinal sagittal imbalance and life quality. Zhonghua Yi Xue Za Zhi. 2012; 92(21):1481–1485.20. Marsicano JG, Lenke LG, Bridwell KH, Chapman M, Gupta P, Weston J. The lordotic effect of the OSI frame on operative adolescent idiopathic scoliosis patients. Spine (Phila Pa 1976). 1998; 23(12):1341–1348.
Article21. Tan SB, Kozak JA, Dickson JH, Nalty TJ. Effect of operative position on sagittal alignment of the lumbar spine. Spine (Phila Pa 1976). 1994; 19(3):314–318.
Article22. Tribus CB, Belanger TA, Zdeblick TA. The effect of operative position and short-segment fusion on maintenance of sagittal alignment of the lumbar spine. Spine (Phila Pa 1976). 1999; 24(1):58–61.
Article23. Vialle R, Ilharreborde B, Dauzac C, Lenoir T, Rillardon L, Guigui P. Is there a sagittal imbalance of the spine in isthmic spondylolisthesis? A correlation study. Eur Spine J. 2007; 16(10):1641–1649.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparision of Lumbar Lordosis According to Different Operative Positions
- A Case of Coexisting Cervical and Lumbar Spinal Stenosis
- Radiographic Results of Single Level Transforaminal Lumbar Interbody Fusion in Degenerative Lumbar Spine Disease: Focusing on Changes of Segmental Lordosis in Fusion Segment
- The Influence of Central Venous Pressure on Blood Loss during Spinal Fusion in Prone Position
- Loss of the Sagittal angle in the Instrumented Segments after Pedicular Screw Fixation of the Degenerative Lumbar Diseases