Korean J Ophthalmol.
2016 Feb;30(1):60-65. 10.3341/kjo.2016.30.1.60.
The Stabilization of Postoperative Exo-drift in Intermittent Exotropia after Surgical Treatment
- Affiliations
-
- 1Department of Ophthalmology, Eulji General Hospital, Eulji University School of Medicine, Seoul, Korea.
- 2Department of Ophthalmology, Yeungnam University College of Medicine, Daegu, Korea. mmk@med.yu.ac.kr
- KMID: 2363892
- DOI: http://doi.org/10.3341/kjo.2016.30.1.60
Abstract
- PURPOSE
To investigate the long-term clinical course of intermittent exotropia after surgical treatment to determine whether and when postoperative exo-drift stabilizes, and the required postsurgery follow-up duration in cases of intermittent exotropia.
METHODS
We retrospectively reviewed the medical records of patients diagnosed with intermittent exotropia who underwent surgical treatment between January 1992 and January 2006 at Yeungnam University Hospital and postoperatively performed regular follow-up examinations for up to 7 years. We also analyzed the difference in exo-drift stabilization, according to surgical procedure.
RESULTS
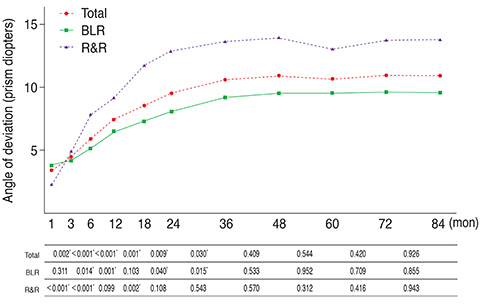
A total of 101 patients were enrolled in the study. Thirty-one patients underwent lateral rectus recession and medial rectus resection (R&R) and 70 patients underwent bilateral lateral rectus recession (BLR). The postoperative angles of deviation increased significantly during the initial 36 months, but no subsequent significant changes were observed for up to 84 months. Follow-ups for 7 years revealed that more than 50% of the total amount of exo-drift was observed within the first postoperative year. In addition, the angles of deviation at 1 year correlated with those at 7 years postoperatively (Pearson correlation coefficient r = 0.517, p < 0.001). No significant exo-drift was observed after 36 months in patients who underwent BLR, whereas after 18 months in patients who underwent R&R.
CONCLUSIONS
The minimum postoperative follow-up required after surgical treatment to ensure stable results is 36 months. In particular, careful follow-up is necessary during the first postoperative year to detect rapid exo-drift. Patients who underwent BLR required a longer follow-up than those who underwent R&R to ensure stable postoperative alignment.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Characteristics of Patients Who Are Not Responsive to Alternate Patching for Overcorrected Intermittent Exotropia
Jung Yup Kim, Hae Rang Kim, Soo Jung Lee
Korean J Ophthalmol. 2018;32(4):319-327. doi: 10.3341/kjo.2017.0086.
Reference
-
1. Figueira EC, Hing S. Intermittent exotropia: comparison of treatments. Clin Experiment Ophthalmol. 2006; 34:245–251.2. Ekdawi NS, Nusz KJ, Diehl NN, Mohney BG. Postoperative outcomes in children with intermittent exotropia from a population-based cohort. J AAPOS. 2009; 13:4–7.3. Kim WJ, Kim MM. The clinical course of recurrent intermittent exotropia following one or two surgeries over 24 months postoperatively. Eye (Lond). 2014; 28:819–824.4. Scott WE, Keech R, Mash AJ. The postoperative results and stability of exodeviations. Arch Ophthalmol. 1981; 99:1814–1818.5. Choi J, Chang JW, Kim SJ, Yu YS. The long-term survival analysis of bilateral lateral rectus recession versus unilateral recession-resection for intermittent exotropia. Am J Ophthalmol. 2012; 153:343–351.e1.6. Pineles SL, Ela-Dalman N, Zvansky AG, et al. Long-term results of the surgical management of intermittent exotropia. J AAPOS. 2010; 14:298–304.7. Maruo T, Kubota N, Sakaue T, Usui C. Intermittent exotropia surgery in children: long term outcome regarding changes in binocular alignment. A study of 666 cases. Binocul Vis Strabismus Q. 2001; 16:265–270.8. Mun HJ, Kim MM. Comparison of surgical results between bilateral recession and unilateral recession-resection in 25 PD intermittent exotropia. J Korean Ophthalmol Soc. 2002; 43:2202–2207.9. Park KH, Kim SY. Clinical characteristics of patients that experience different rates of exodrift after strabismus surgery for intermittent exotropia and the effect of the rate of exodrift on final ocular alignment. J AAPOS. 2013; 17:54–58.10. Leow PL, Ko ST, Wu PK, Chan CW. Exotropic drift and ocular alignment after surgical correction for intermittent exotropia. J Pediatr Ophthalmol Strabismus. 2010; 47:12–16.11. Kordic H, Sturm V, Landau K. Long-term follow-up after surgery for exodeviation. Klin Monbl Augenheilkd. 2009; 226:315–320.12. Kwon J, Kim SH, Cho YA. Postoperative stabilization of the strabismic angle in intermittent exotropia. Korean J Ophthalmol. 2012; 26:446–450.13. Lim SH, Hong JS, Kim MM. Prognostic factors for recurrence with unilateral recess-resect procedure in patients with intermittent exotropia. Eye (Lond). 2011; 25:449–454.14. Lim SH, Hwang BS, Kim MM. Prognostic factors for recurrence after bilateral rectus recession procedure in patients with intermittent exotropia. Eye (Lond). 2012; 26:846–852.15. Yang X, Man TT, Tian QX, et al. Long-term postoperative outcomes of bilateral lateral rectus recession vs unilateral recession-resection for intermittent exotropia. Int J Ophthalmol. 2014; 7:1043–1047.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Postoperative Stabilization of the Strabismic Angle in Intermittent Exotropia
- Postoperative Exotropic Drift: Comparison of Surgical Methods Combined with Lateral Rectus Muscle Recession in Exotropia
- The Change in Deviation Angle with Time Course after Surgical Correction of Intermittent Exotropia
- The Relationship Between Velocity of Early Exotropic Drift and Recurrence
- The Surgical Outcome of Intermittent Exotropia and the Prognostic Factors