Investig Clin Urol.
2016 Mar;57(2):129-134. 10.4111/icu.2016.57.2.129.
Vancomycin resistant enterococci in urine cultures: Antibiotic susceptibility trends over a decade at a tertiary hospital in the United Kingdom
- Affiliations
-
- 1Department of Surgery, Urology Unit, University of Melbourne, Melbourne, Australia. Lawrentscuk@gmail.com
- 2Department of Microbiology, Addenbrookes' Hospital, Cambridge University, Cambridge, UK.
- 3Department of Urology, Addenbrookes' Hospital, Cambridge University, Cambridge, UK.
- 4Olivia Newton-John Cancer Research Institute, Austin Health, Melbourne, Australia.
- 5Department of Surgical Oncology, Peter MacCallum Cancer Centre, Melbourne, Australia.
- KMID: 2363135
- DOI: http://doi.org/10.4111/icu.2016.57.2.129
Abstract
- PURPOSE
Enterococci are a common cause of urinary tract infection and vancomycin-resistant strains are more difficult to treat. The purpose of this surveillance program was to assess the prevalence of and determine the risk factors for vancomycin resistance in adults among urinary isolates of Enterococcus sp. and to detail the antibiotic susceptibility profile, which can be used to guide empirical treatment.
MATERIALS AND METHODS
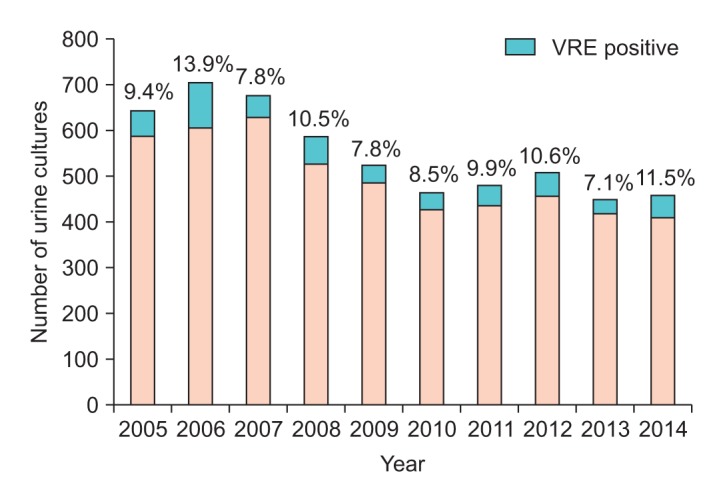
From 2005 to 2014 we retrospectively reviewed 5,528 positive Enterococcus sp. urine cultures recorded in a computerized laboratory results database at a tertiary teaching hospital in Cambridge, United Kingdom.
RESULTS
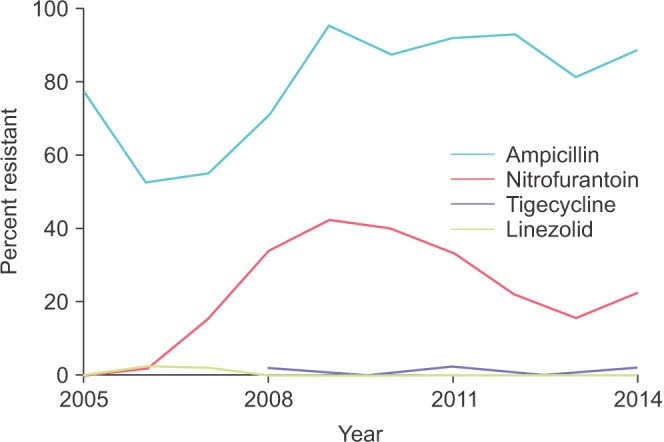
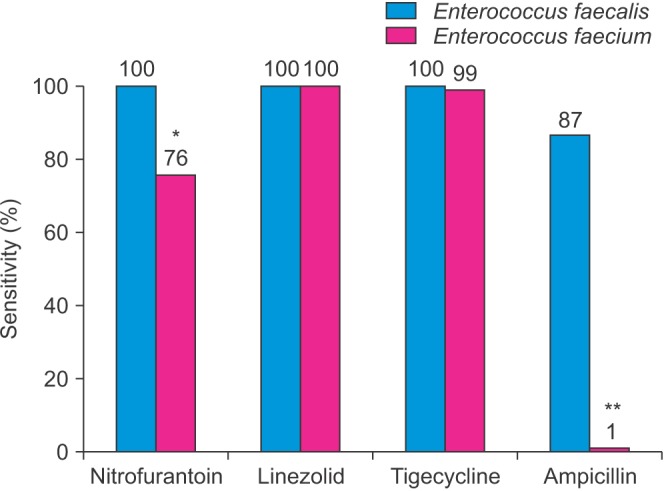
Of these cultures, 542 (9.8%) were vancomycin resistant. No longitudinal trend was observed in the proportion of vancomycin-resistant strains over the course of the study. We observed emerging resistance to nitrofurantoin with rates climbing from near zero to 40%. Ampicillin resistance fluctuated between 50% and 90%. Low resistance was observed for linezolid and quinupristin/dalfopristin. Female sex and inpatient status were identified as risk factors for vancomycin resistance.
CONCLUSIONS
The incidence of vancomycin resistance among urinary isolates was stable over the last decade. Although resistance to nitrofurantoin has increased, it still serves as an appropriate first choice in uncomplicated urinary tract infection caused by vancomycin-resistant Enterococcus sp.
Keyword
MeSH Terms
-
Aged
Drug Resistance, Bacterial
England
Female
Gram-Positive Bacterial Infections/drug therapy/*microbiology
Hospitalization/statistics & numerical data
Humans
Male
Microbial Sensitivity Tests
Middle Aged
Retrospective Studies
Risk Factors
Tertiary Care Centers
Urinalysis
Urinary Tract Infections/drug therapy/*microbiology
*Vancomycin Resistance
Vancomycin-Resistant Enterococci/drug effects/*isolation & purification
Figure
Reference
-
1. Heintz BH, Cho S, Fujioka A, Li J, Halilovic J. Evaluation of the treatment of vancomycin-resistant enterococcal urinary tract infections in a large academic medical center. Ann Pharmacother. 2013; 47:159–169. PMID: 23341161.
Article2. Heintz BH, Halilovic J, Christensen CL. Vancomycin-resistant enterococcal urinary tract infections. Pharmacotherapy. 2010; 30:1136–1149. PMID: 20973687.
Article3. Lloyd-Smith P, Younger J, Lloyd-Smith E, Green H, Leung V, Romney MG. Economic analysis of vancomycin-resistant enterococci at a Canadian hospital: assessing attributable cost and length of stay. J Hosp Infect. 2013; 85:54–59. PMID: 23920443.
Article4. Werner G, Coque TM, Hammerum AM, Hope R, Hryniewicz W, Johnson A, et al. Emergence and spread of vancomycin resistance among enterococci in Europe. Euro Surveill. 2008; 13(47):pii: 19046.
Article5. Center for Disease Control and Prevention. Information for the public about VRE. 2008 [Internet]. Atlanta (GA): Center for Disease Control and Prevention;2016. cited 2016 Jan 15. Available from: http://www.cdc.gov/ncidod/dhqp/ar_VRE_publicFAQ.html.6. DiazGranados CA, Zimmer SM, Klein M, Jernigan JA. Comparison of mortality associated with vancomycin-resistant and vancomycin-susceptible enterococcal bloodstream infections: a meta-analysis. Clin Infect Dis. 2005; 41:327–333. PMID: 16007529.
Article7. Khair HN, VanTassell P, Henderson JP, Warren DK, Marschall J. CDC Prevention Epicenters Program. Vancomycin resistance has no influence on outcomes of enterococcal bacteriuria. J Hosp Infect. 2013; 85:183–188. PMID: 23998947.
Article8. Dancer SJ. Controlling hospital-acquired infection: focus on the role of the environment and new technologies for decontamination. Clin Microbiol Rev. 2014; 27:665–690. PMID: 25278571.
Article9. Pereira GH, Muller PR, Zanella RC, de Jesus Castro Lima M, Torchio DS, Levin AS. Outbreak of vancomycin-resistant enterococci in a tertiary hospital: the lack of effect of measures directed mainly by surveillance cultures and differences in response between Enterococcus faecium and Enterococcus faecalis. Am J Infect Control. 2010; 38:406–409. PMID: 20006408.
Article11. Zhanel GG, Laing NM, Nichol KA, Palatnick LP, Noreddin A, Hisanaga T, et al. Antibiotic activity against urinary tract infection (UTI) isolates of vancomycin-resistant enterococci (VRE): results from the 2002 North American Vancomycin Resistant Enterococci Susceptibility Study (NAVRESS). J Antimicrob Chemother. 2003; 52:382–388. PMID: 12888592.
Article12. Garrison MW, Mutters R, Dowzicky MJ. In vitro activity of tigecycline and comparator agents against a global collection of Gram-negative and Gram-positive organisms: tigecycline Evaluation and Surveillance Trial 2004 to 2007. Diagn Microbiol Infect Dis. 2009; 65:288–299. PMID: 19733459.
Article13. Nix DE, Matthias KR. Should tigecycline be considered for urinary tract infections? A pharmacokinetic re-evaluation. J Antimicrob Chemother. 2010; 65:1311–1312. PMID: 20378673.
Article14. Rivera AM, Boucher HW. Current concepts in antimicrobial therapy against select gram-positive organisms: methicillin-resistant Staphylococcus aureus, penicillin-resistant pneumococci, and vancomycin-resistant enterococci. Mayo Clin Proc. 2011; 86:1230–1243. PMID: 22134942.15. Toner L, Papa N, Aliyu SH, Dev H, Lawrentschuk N, Al-Hayek S. Extended-spectrum beta-lactamase-producing Enterobacteriaceae in hospital urinary tract infections: incidence and antibiotic susceptibility profile over 9 years. World J Urol. 2015; 10. 28. [Epub]. DOI: 10.1007/s00345-015-1718-x.16. Toner L, Papa N, Aliyu SH, Dev H, Lawrentschuk N, Al-Hayek S. Candida growth in urine cultures: a contemporary analysis of species and antifungal susceptibility profiles. QJM. 2015; 11. 4. [Epub]. DOI: 10.1093/qjmed/hcv202.17. De Angelis G, Cataldo MA, De Waure C, Venturiello S, La Torre G, Cauda R, et al. Infection control and prevention measures to reduce the spread of vancomycin-resistant enterococci in hospitalized patients: a systematic review and meta-analysis. J Antimicrob Chemother. 2014; 69:1185–1192. PMID: 24458513.
Article18. Brolund A. Overview of ESBL-producing Enterobacteriaceae from a Nordic perspective. Infect Ecol Epidemiol. 2014; 10. 1. 4:DOI: 10.3402/iee.v4.24555.
Article19. Wang JL, Hsueh PR. Therapeutic options for infections due to vancomycin-resistant enterococci. Expert Opin Pharmacother. 2009; 10:785–796. PMID: 19351228.
Article20. Therapeutic Guidelines Limited. Acute cystitis in adults. eTG complete [Internet]. Melbourne (GA): Therapeutic Guidelines Limited;2015 Apr 29. Available from: http://www.tg.org.au/.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Transplantation of a kidney from a donor with vancomycin-resistant Enterococci
- In Vitro Activities of Daptomycin Against Recent Clinical Isolates of Methicillin-resistant Staphylococci and Vancomycin-resistant Enterococci in Korea
- Trends of Antimicrobial Susceptibility Test for Bacterias Isolated from Blood, Urine, Stool, and Cerebrospinal Fluid(1997~2001)
- Resistance Mechanism and Epidemiology of Vancomycin-resistant Enterococci
- Vancomycin-resistant Staphylococcus aureus