J Korean Foot Ankle Soc.
2016 Dec;20(4):152-157. 10.14193/jkfas.2016.20.4.152.
Shortening Scarf Osteotomy for Treatment of Hallux Rigidus Deformity
- Affiliations
-
- 1Department of Orthopedic Surgery, Pohang St. Mary's Hospital, Pohang, Korea. OSbonelee@gmail.com
- KMID: 2362762
- DOI: http://doi.org/10.14193/jkfas.2016.20.4.152
Abstract
- PURPOSE
To evaluate the effect of shortening scarf osteotomy on pain relief and range of motion (ROM) of the first metatarsophalangeal joint in hallux rigidus patients.
MATERIALS AND METHODS
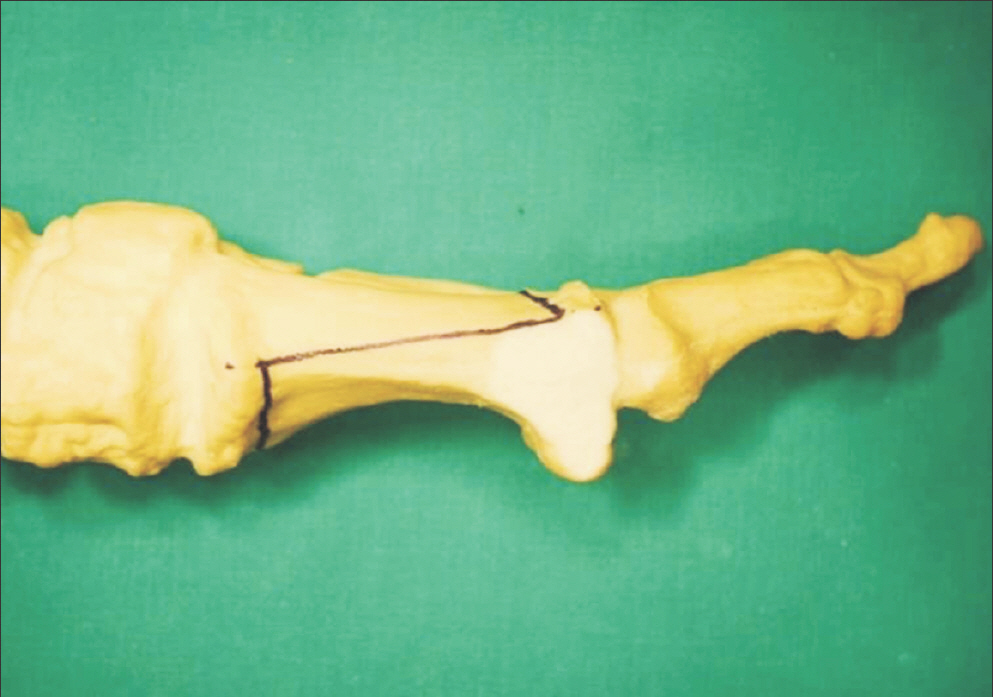
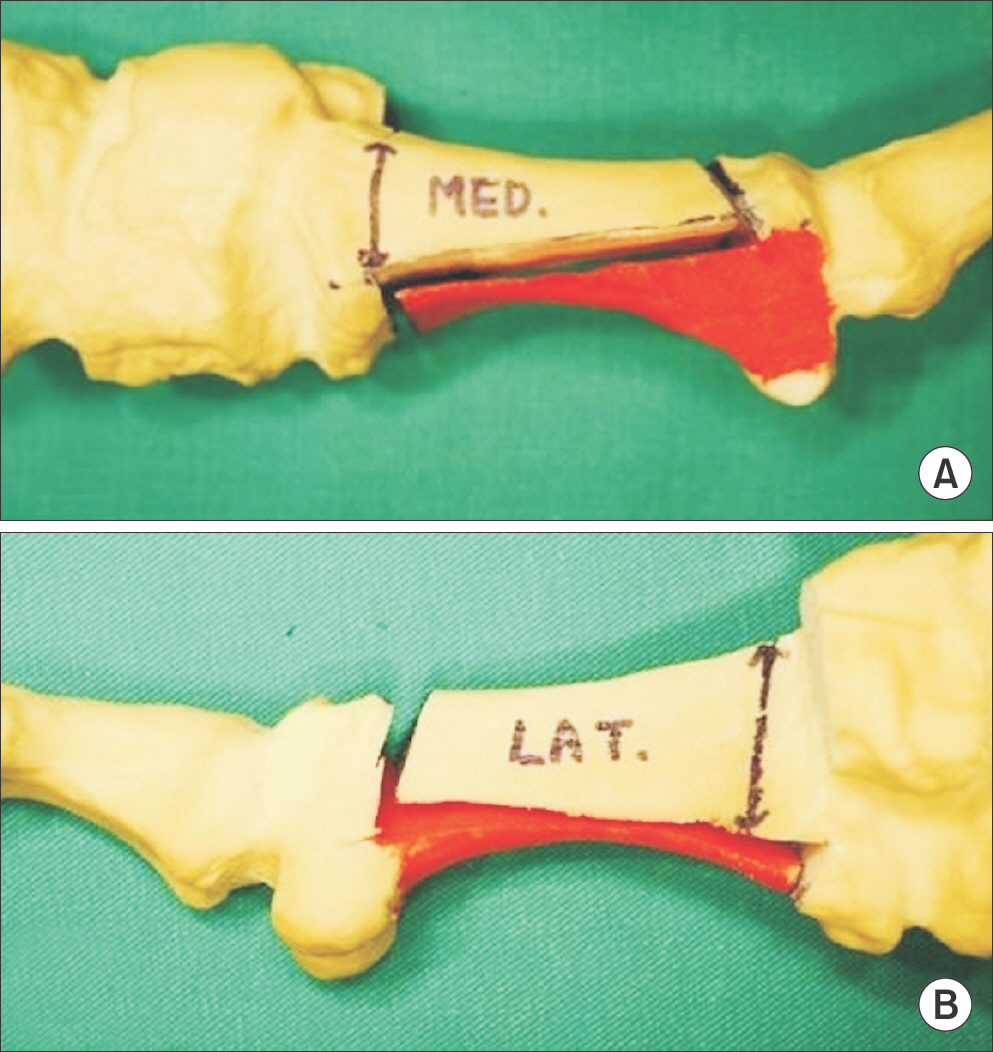
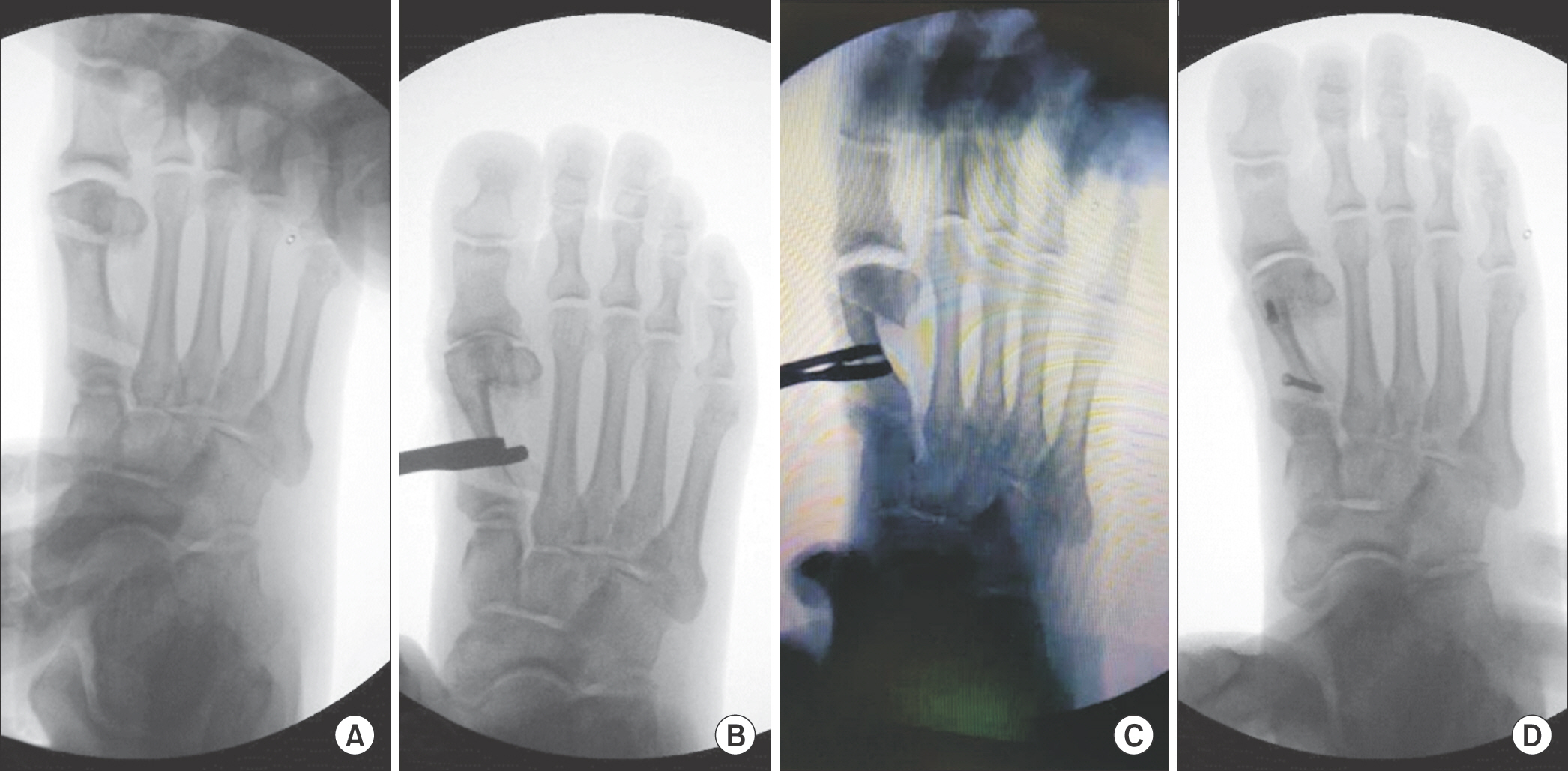
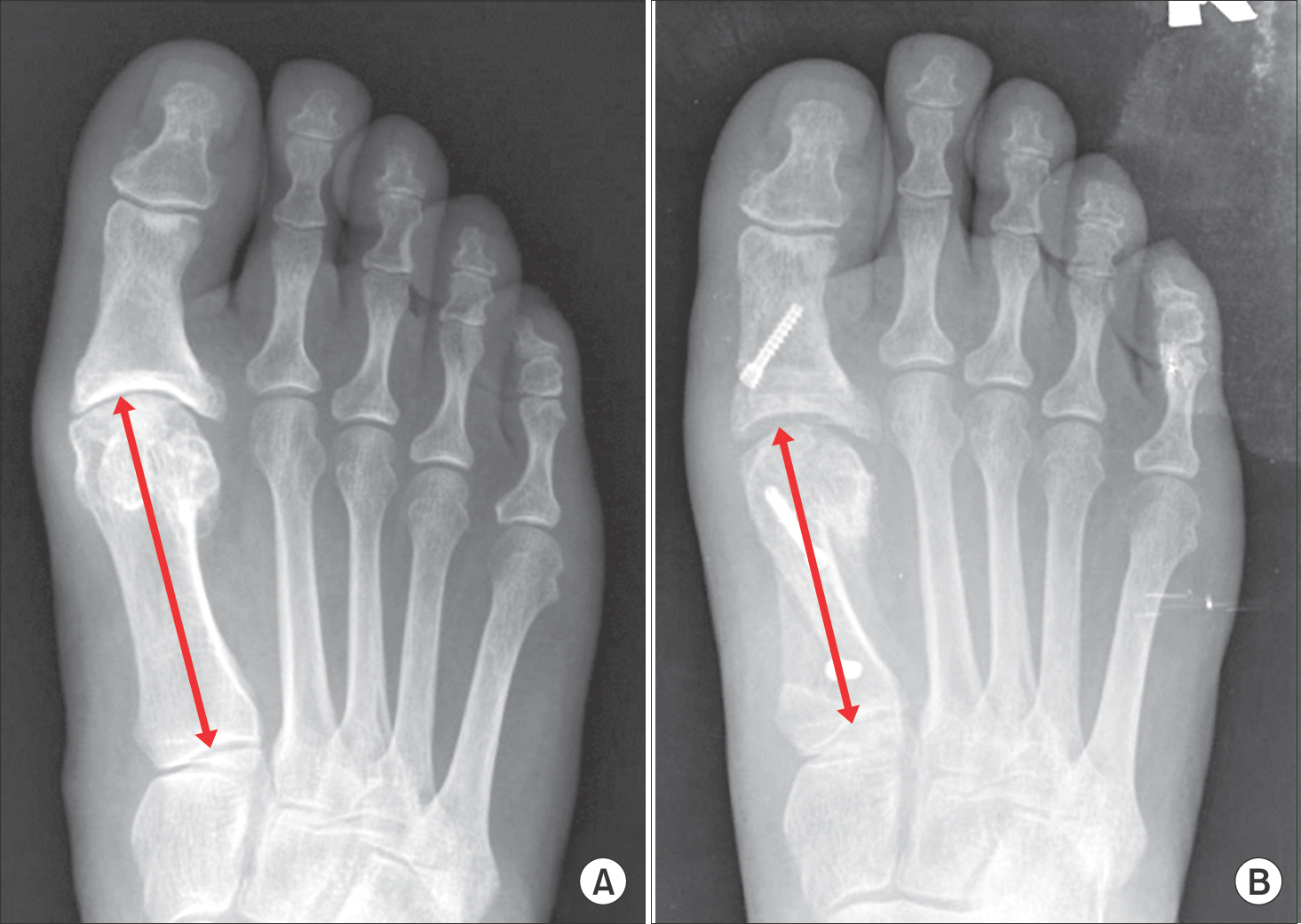
Twenty-three cases of 19 patients who had been treated with shortening scarf osteotomy for the hallux rigidus between January 2007 and December 2013 were reviewed. The mean follow-up period was 21.4 months, and the mean age was 59.2 years. The first metatarsal bone was shortened until the ROM of the first metatarsophalangeal joint was greater than 80° or 40° of dorsiflexion. The length shortened by scarf osteotomy was measured. The authors also measured and compared the joint interval difference of the standing foot using an anteroposterior radiography. Moreover, the difference of ROM of the first metatarsophalangeal joint between the preoperative and final follow-up periods was also compared. The clinical results were evaluated and compared using the American Orthopaedic Foot and Ankle Society (AOFAS) scoring system and visual analogue scale (VAS) score.
RESULTS
The mean shortening length was about 6.5 mm (range, 4∼9 mm). The joint space has been increased to 1.8 mm, and the ROM of the first metatarsophalangeal joint has also been increased to 18.4° after the operation. In three cases, the postoperative ROM has been decreased to less 10°. The AOFAS score has been improved from 41.7 (range, 32∼55) to 86.2 (range, 65∼95), and the VAS score was also decreased from 3.7 (range, 3∼5) to 1.3 (range, 0∼3). Two cases have shown no decrease in pain even after the operation.
CONCLUSION
Shortening scarf osteotomy was found to decrease joint pain by decompressing the pressure of the first metatarsophalangeal joint. This osteotomy also helped improve the ROM of the first metatarsophalangeal joint. Shortening scarf osteotomy can be considered one of the effective methods for joint preservation.
MeSH Terms
Figure
Reference
-
1.Haddad SL. The use of osteotomies in the treatment of hallux limitus and hallux rigidus. Foot Ankle Clin. 2000. 5:629–61.2.Polzer H., Polzer S., Brumann M., Mutschler W., Regauer M. Hallux rigidus: joint preserving alternatives to arthrodesis - a review of the literature. World J Orthop. 2014. 5:6–13.
Article3.Ronconi P., Monachino P., Baleanu PM., Favilli G. Distal oblique osteotomy of the first metatarsal for the correction of hallux limitus and rigidus deformity. J Foot Ankle Surg. 2000. 39:154–60.
Article4.Migues A., Slullitel G. Joint-preserving procedure for moderate hallux rigidus. Foot Ankle Clin. 2012. 17:459–71.
Article5.Malerba F., Milani R., Sartorelli E., Haddo O. Distal oblique first metatarsal osteotomy in grade 3 hallux rigidus: a long-term fol-lowup. Foot Ankle Int. 2008. 29:677–82.
Article6.Coughlin MJ., Shurnas PS. Hallux rigidus1 Grading and long-term results of operative treatment. J Bone Joint Surg Am. 2003. 85:2072–88.7.Mann RA., Clanton TO. Hallux rigidus: treatment by cheilectomy. J Bone Joint Surg Am. 1988. 70:400–6.8.Mann RA., Coughlin MJ., DuVries HL. Hallux rigidus: a review of the literature and a method of treatment. Clin Orthop Relat Res. 1979. 142:57–63.9.Kilmartin TE. Phalangeal osteotomy versus first metatarsal decompression osteotomy for the surgical treatment of hallux rigidus: a prospective study of age-matched and condition-matched patients. J Foot Ankle Surg. 2005. 44:2–12.
Article10.Barouk LS. Forefoot reconstruction. Paris: Springer-Verlag;2006.11.Deland JT., Williams BR. Surgical management of hallux rigidus. J Am Acad Orthop Surg. 2012. 20:347–58.
Article12.Desmarchelier R., Besse JL., Fessy MH. French Association of Foot Surgery (AFCP). Scarf osteotomy versus metatarsophalangeal arthrodesis in forefoot first ray disorders: comparison of functional outcomes. Orthop Traumatol Surg Res. 2012. 98(6 Suppl):S77–84.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Scarf Osteotomy for the Treatment of Recurred Hallux Valgus
- Treatment Results of Hallux Valgus Deformity by Parallel-Shaped Modified Scarf Osteotomy
- Operative Treatment of the Bilateral 1,4th Brachymetatarsia with Painful Callosity and Hallux Varus using Massive Metatarsal Axial Shortening: A Case Report
- Result of Joint Preserving Surgery Using Axial Shortening Metatarsal Osteotomy for the Treatment of Severe Hallux Valgus and Claw Toes Deformity in Advanced Rheumatoid Arthritis
- Modified Proximal Scarf Osteotomy for Hallux Valgus