J Rhinol.
2016 Nov;23(2):75-80. 10.18787/jr.2016.23.2.75.
Clinical Implications of Snoring
- Affiliations
-
- 1Department of Otorhinolaryngology, College of Medicine, Hanyang University, Seoul, Korea. shcho@hanyang.ac.kr
- KMID: 2361318
- DOI: http://doi.org/10.18787/jr.2016.23.2.75
Abstract
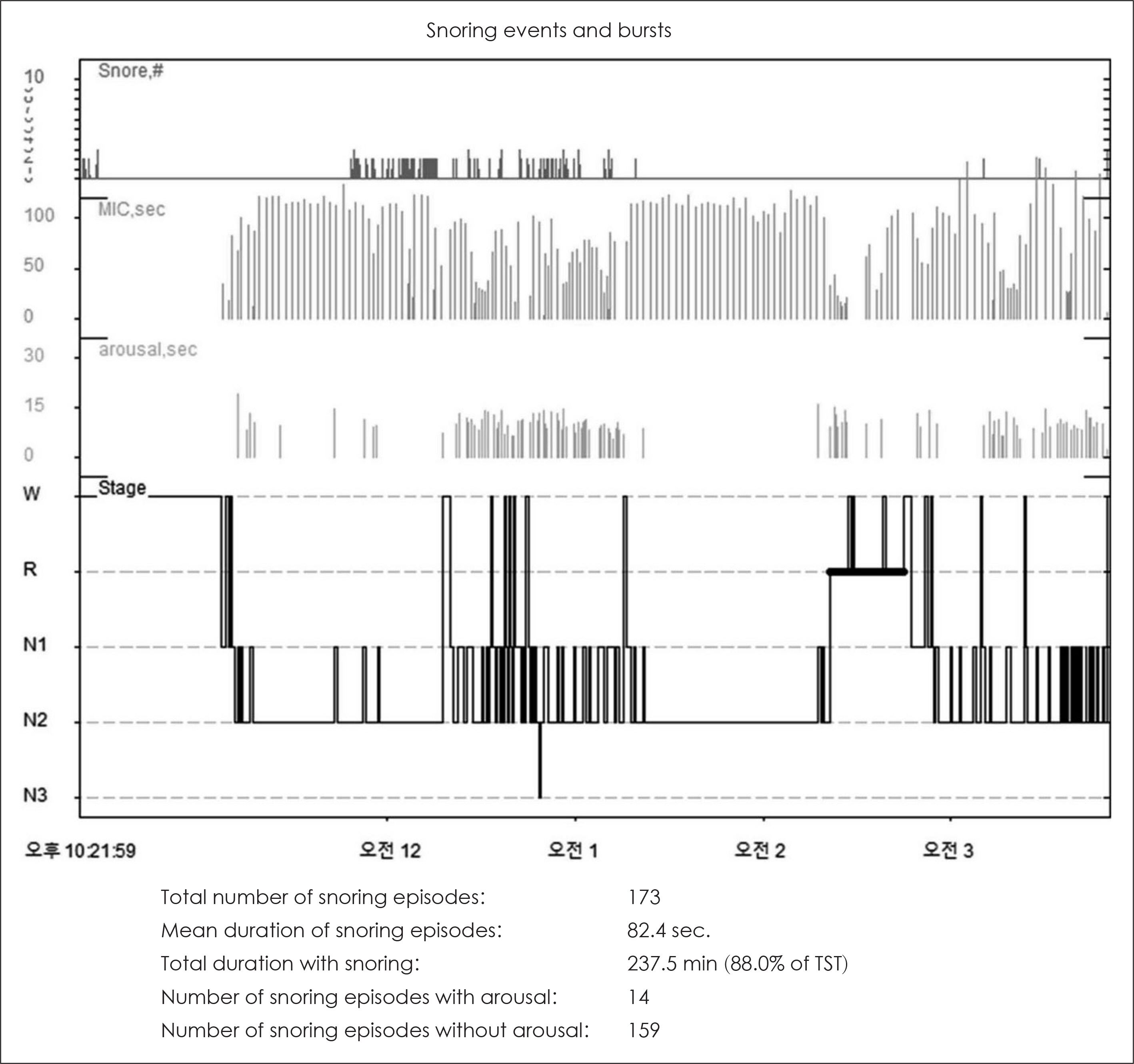
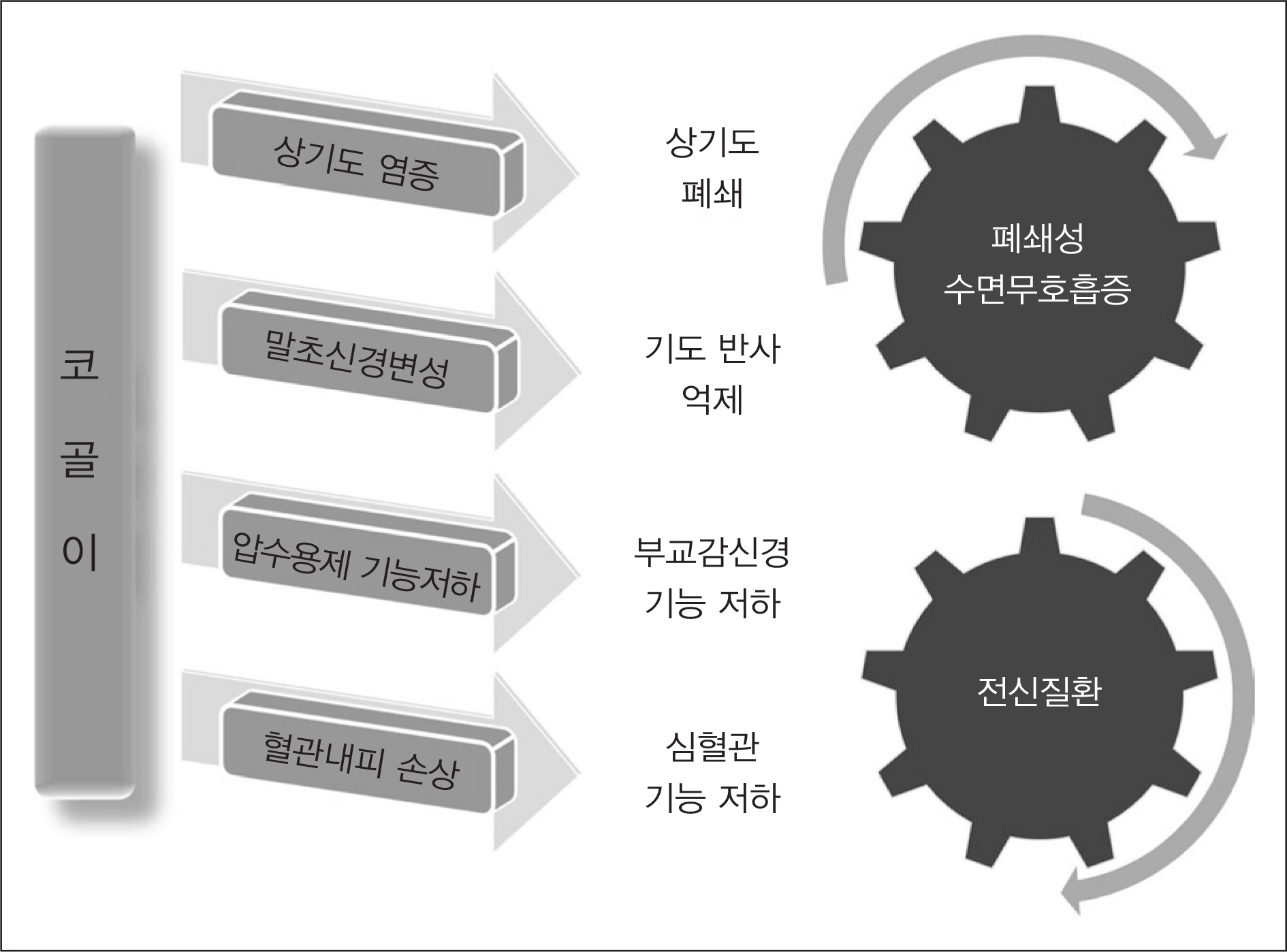
- Snoring is the most common symptom, along with increased daytime sleepiness, in patients with obstructive sleep apnea (OSA). However, doctors often neglect snoring in clinical practice, and snoring is not addressed in the treatment guidelines of OSA. Therefore, study about snoring and its clinical implications in sleep medicine are needed. The natural history of snoring shows that snoring can evolve into OSA, and the most important risk factors for this continuum are obesity and male sex. Snoring can be a social problem causing annoyance and family difficulties. Animal and human studies have shown that snoring involves the four injury mechanisms of upper airway inflammation, peripheral neuropathy, parasympathetic hypofunction, and endothelial injury. Previous studies have reported that systemic diseases such as atherosclerosis, metabolic syndrome, hypertension, and cardiac diseases were comorbid with snoring. However, most of these studies enrolled patients characterized by survey or questionnaire; therefore, data were biased with effects of OSA. Thus, consensus on the definition and detection of snoring is lacking. Additional studies are required to determine the exact clinical implications of snoring.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Clinical Review of Commercially-Available Anti-Snoring Devices
Ki-Il Lee, Ji Ho Choi
Korean J Otorhinolaryngol-Head Neck Surg. 2023;66(6):367-374. doi: 10.3342/kjorl-hns.2022.01186.
Reference
-
References
1). Deary V, Ellis JG, Wilson JA, Coulter C, Barclay NL. Simple snoring: not quite so simple after all? Sleep Med Rev. 2014; 18:453–62.
Article2). Koren A, Groselj LD, Fajdiga I. CT comparison of primary snoring and obstructive sleep apnea syndrome: role of pharyngeal narrowing ratio and soft palate-tongue contact in awake patient. Eur Arch Otorhinolaryngol. 2009; 266:727–34.
Article3). Lee JG. Pathophysiology of snoring. Korean J Rhinol. 1995; 2:3–7.4). Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, Kapur VK, et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. J Clin Sleep Med. 2012; 8(5):597–619.
Article5). Cathcart RA, Hamilton DW, Drinnan MJ, Gibson GJ, Wilson JA. Night-to-night variation in snoring sound severity: one night studies are not reliable. Clin Otolaryngol. 2010; 35:198–203.
Article6). Blumen MB, Quera Salva MA, Vaugier I, Leroux K, d'Ortho MP, Barbot F, et al. Is snoring intensity responsible for the sleep partner's poor quality of sleep? Sleep Breath. 2012 Sep; 16(3):903–7.
Article7). Chan CH, Wong BM, Tang JL, Ng DK. Gender difference in snoring and how it changes with age: systematic review and meta-regression. Sleep Breath. 2012; 16:977–86.
Article8). Ng DK, Chan CH, Ng EP. Natural history of snoring in Hong Kong adolescents. J Paediatr Child Health. 2014; 50:596–604.
Article9). Li AM, Zhu Y, Au CT, Lee DL, Ho C, Wing YK. Natural history of primary snoring in school-aged children: a 4-year follow-up study. Chest. 2013; 143:729–35.10). Berger G, Berger R, Oksenberg A. Progression of snoring and obstructive sleep apnoea: the role of increasing weight and time. Eur Respir J. 2009; 33:338–45.
Article11). Dreher A, Rader T, Patscheider M, Klemens C, Schmidt M, Baker F, et al. The annoyance of snoring. Eur Arch Otorhinolaryngol. 2009; 266(2):293–6.
Article12). Zarhin D. Sleep as a Gendered Family Affair: Snoring and the “Dark Side” of Relationships. Qual Health Res. In press.13). Boynton G, Vahabzadeh A, Hammoud S, Ruzicka DL, Chervin RD. Validation of the STOP-BANG Questionnaire among Patients Referred for Suspected Obstructive Sleep Apnea. J Sleep Disord Treat Care. 2013; 23(2):1–20.14). Kang K, Park KS, Kim JE, Kim SW, Kim YT, Kim JS, et al. Usefulness of the Berlin Questionnaire to identify patients at high risk for obstructive sleep apnea: a population-based door-to-door study. Sleep Breath. 2013; 17:803–10.
Article15). Thornton AT, Singh P, Ruehland WR, Rochford PD. AASM criteria for scoring respiratory events: interaction between apnea sensor and hypopnea definition. Sleep. 2012; 35:425–32.
Article16). Park CY, Hong JH, Lee JH, Lee KE, Cho HS, Lim SJ, et al. Clinical usefulness of watch-PAT for assessing the surgical results of obstructive sleep apnea syndrome. J Clin Sleep Med. 2014; 10(1):43–7.
Article17). Almendros I, Acerbi I, Puig F, Montserrat JM, Navajas D, Farré R. Upper-airway inflammation triggered by vibration in a rat model of snoring. Sleep. 2007; 30:225–7.
Article18). Hagander L, Harlid R, Svanborg E. Quantitative sensory testing in the oropharynx: a means of showing nervous lesions in patients with obstructive sleep apnea and snoring. Chest. 2009; 136:481–9.19). Schöbel C, Fietze I, Glos M, Schary I, Blau A, Baumann G, et al. Nocturnal snoring decreases daytime baroreceptor sensitivity. Respir Med. 2014; 108:1049–55.
Article20). Cho JG, Witting PK, Verma M, Wu BJ, Shanu A, Kairaitis K, Amis TC, Wheatley JR. Tissue vibration induces carotid artery endothelial dysfunction: a mechanism linking snoring and carotid atherosclerosis? Sleep. 2011; 34:751–7.
Article21). Lee YH, Kweon SS, Choi BY, Kim MK, Chun BY, Shin DH, et al. Self-reported snoring and carotid atherosclerosis in middle-aged and older adults: the Korean Multi-Rural Communities Cohort Study. J Epidemiol. 2014; 24:281–6.
Article22). Leineweber C, Kecklund G, Akerstedt T, Janszky I, Orth-Gomér K. Snoring and the metabolic syndrome in women. Sleep Med. 2003; 4:531–6.
Article23). Shin C, Kim J, Kim J, Lee S, Shim J, In K, et al. Association of habitual snoring with glucose and insulin metabolism in nonobese Korean adult men. Am J Respir Crit Care Med. 2005; 171:287–91.
Article24). Kim J, Yi H, Shin KR, Kim JH, Jung KH, Shin C. Snoring as an independent risk factor for hypertension in the nonobese population: the Korean Health and Genome Study. Am J Hypertens. 2007; 20:819–24.
Article25). Endeshaw Y, Rice TB, Schwartz AV, Stone KL, Manini TM, Satter-field S, et al. Snoring, daytime sleepiness, and incident cardiovascular disease in the health, aging, and body composition study. Sleep. 2013; 36:1737–45.
Article26). Li D, Liu D, Wang X, He D. Self-reported habitual snoring and risk of cardiovascular disease and all-cause mortality. Atherosclerosis. 2014; 235:189–95.
Article27). Li M, Li K, Zhang XW, Hou WS, Tang ZY. Habitual snoring and risk of stroke: A metaanalysis of prospective studies. Int J Cardiol. 2015; 185:46–9.
Article28). Yeboah J, Redline S, Johnson C, Tracy R, Ouyang P, Blumenthal RS, et al. Association between sleep apnea, snoring, incident cardiovascular events and all-cause mortality in an adult population: MESA. Atherosclerosis. 2011; 219:963–8.
Article29). Marshall NS, Wong KK, Cullen SR, Knuiman MW, Grunstein RR. Snoring is not associated with all-cause mortality, incident cardiovascular disease, or stroke in the Busselton Health Study. Sleep. 2012; 35:1235–40.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Implications of Snoring Time (%) in Patients with Obstructive Sleep Apnea
- Treatment of Snoring and the Change of Surgical Treatment
- Prevalence of Snoring and Factors Affecting Habitual Snoring in Korean Adults
- The Relationship between Snoring Noise and Hearing Impairment in Snorers and Their Spouses
- Snoring and Sleep Apnea