Allergy Asthma Respir Dis.
2016 Mar;4(2):149-153. 10.4168/aard.2016.4.2.149.
Right middle lobe syndrome caused by eosinophilic mucoid impaction in adults
- Affiliations
-
- 1Division of Pulmonary, Allergy, and Critical Care Medicine, Department of Internal Medicine, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, Anyang, Korea. luxjhee@gmail.com
- 2Department of Radiology, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, Anyang, Korea.
- KMID: 2361289
- DOI: http://doi.org/10.4168/aard.2016.4.2.149
Abstract
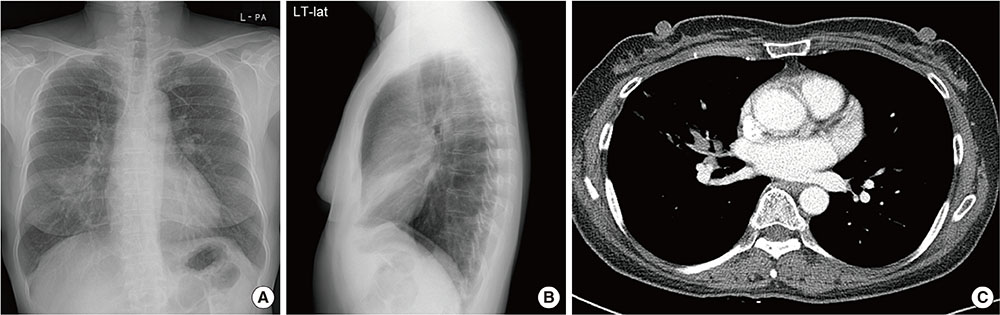
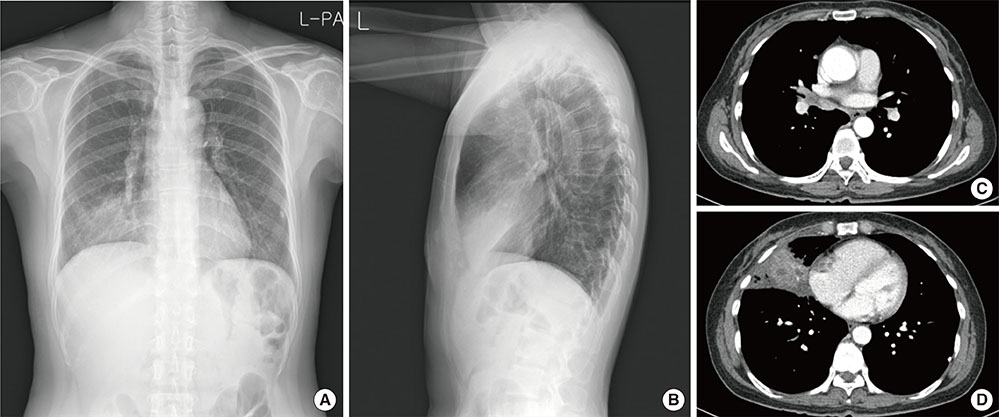
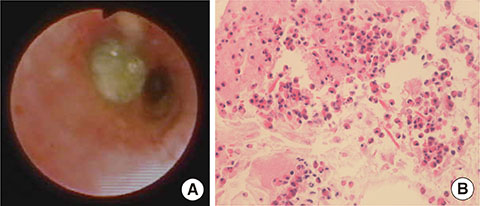
- Right middle lobe syndrome (RMLS) is defined as a transient or recurrent, chronic collapse of the middle lobe of the right lung by certain pathologic conditions. RMLS is a relatively uncommon condition having multiple etiologies and various clinical presentations. Two patients were referred to Hallym University Sacred Heart Hospital, one for the treatment of coughing and the other for the treatment of pneumonia. A diagnosis of RMLS was identified through X-ray and computed tomography image evaluation for each condition. Bronchoscopy revealed mucus obstruction in the right middle lobe bronchus. Biopsy of the aspirated mucus showed mucus containing many eosinophils and Charcot-Leyden crystals. After removal of impacted mucus, clinical and radiological improvements were observed in both patients. Therefore, eosinophilic mucus impaction can be considered a potential cause of RMLS, irrespective of any underlying asthmatic symptoms.
MeSH Terms
Figure
Reference
-
1. Gudbjartsson T, Gudmundsson G. Middle lobe syndrome: a review of clinicopathological features, diagnosis and treatment. Respiration. 2012; 84:80–86.
Article2. Kim HC, Kim HS, Lee SJ, Jeong YY, Jeon KN, Lee JD, et al. Endobronchial tuberculosis pre-senting as right middle lobe syndrome: clinical characteristics and bronchoscopic findings in 22 cases. Yonsei Med J. 2008; 49:615–619.
Article3. Kim HO, Ma JE, Lee SJ, Cho YJ, Jeong YY, Jeon KN, et al. Causes of right middle lobe syndrome: recent experience in local tertiary hospital for several years. Tuberc Respir Dis. 2007; 62:192–196.
Article4. Eskenasy A, Eana-Iorgulescu L. Pathology of the middle lobe syndromes. A histopathological and pathogenetic analysis of sixty surgically-cured cases. Med Interne. 1982; 20:73–80.5. Kim YJ, You DK, Park HY, Cho JM, Park YM, Shin MY, et al. Analysis of the etiologies, ra-diologic findings, bronchoscopic findings, and clinical courses of right middle lobe syn-drome in children. Pediatr Allergy Respir Dis. 2004; 14:342–349.6. Agarwal R, Chakrabarti A, Shah A, Gupta D, Meis JF, Guleria R, et al. Allergic bronchopul-monary aspergillosis: review of literature and proposal of new diagnostic and classification cri-teria. Clin Exp Allergy. 2013; 43:850–873.
Article7. Einarsson JT, Einarsson JG, Isaksson H, Gudbjartsson T, Gudmundsson G. Middle lobe syndrome: a nationwide study on clinicopathological features and surgical treatment. Clin Respir J. 2009; 3:77–81.
Article8. Lee NH, Lee HL, Kim SK, Chang JK, Sung SK, Lee WY. Chest computerized tomographic scan and flexible fiberopticbronchoscopy in the diagnosis of middle lobe syndrome. Tuberc Respir Dis. 1992; 39:236–241.
Article9. Priftis KN, Anthracopoulos MB, Mermiri D, Papadopoulou A, Xepapadaki P, Tsakanika C, et al. Bronchial hyperresponsiveness, atopy, and bronchoalveolar lavage eosinophils in persistent middle lobe syndrome. Pediatr Pulmonol. 2006; 41:805–811.
Article10. Lee J. Formation of airway mucus; synthesis, exocytosis and dilution of gel-forming mu-cins. Korean J Asthma Allergy Clin Immunol. 2012; 32:73–80.11. Rubin BK, Priftis KN, Schmidt HJ, Henke MO. Secretory hyperresponsiveness and pul-mo-nary mucus hypersecretion. Chest. 2014; 146:496–507.
Article12. Kim EJ, Park JE, Kim DH, Lee J. Plastic bronchitis in an adult with asthma. Tuberc Respir Dis. 2012; 73:122–126.
Article13. Shah A, Behera S, Panjabi C. Middle lobe syndrome: a rare presentation of allergic bron-chopulmonary aspergillosis. Eur Ann Allergy Clin Immunol. 2014; 46:147–151.14. Rogers DF. Airway mucus hypersecretion in asthma: an undervalued pathology? Curr Opin Pharmacol. 2004; 4:241–250.
Article15. Nagata K, Iwasaki Y, Yamada T, Yuba T, Kohno K, Hosogi S, et al. Severe asthma compli-cated with large mucoid impaction: successful removal with balloon catheter. Nihon Kokyuki Gakkai Zasshi. 2004; 42:914–918.16. Chun YH, Kang SS, Bang KW, Kim HS, Lee EK, Yoon JS, et al. Usefulness of flexible bron-choscopy in treatment of atelectasis in children. Allergy Asthma Respir Dis. 2013; 1:274–279.
Article17. Seo CD, Oh SH, Youn J, Song YH, Kwon JW, Kim BJ, et al. Mucus plug in a child with asthma. Korean J Asthma Allergy Clin Immunol. 2010; 30:50–54.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Obstructive Pneumonia due to Unknown Eosinophilic Mucoid Impaction of Bronchi: a Case Report
- Middle Lobe Syndrome Caused by Occult Foreign Body in the Bronchus Intermedius: A case report
- A Rare Case of Bronchiectasis with Mucoid Impaction Caused by Schizophyllum commune in an Immunocompetent Woman in South Korea
- Reccurent Unilateral Lung Collapse in an Asthmatic Child
- Pulmonary Consolidation Pattern on the Chest CT: Malignant vs Benign